 |
|
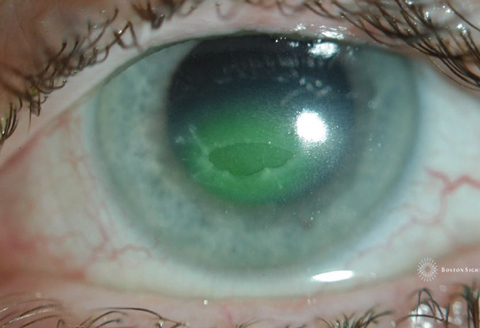
Because insulin-like growth factors contribute to epithelial cell development from limbal stem cells, topical administration of insulin can kick-start the process. Image courtesy of Alan Kwok, OD. Click image to enlarge. |
Corneal defects that fail to improve in the two weeks following injury are known as persistent epithelial defects (PED). Causes of this rare instance of hindered epithelialization include altered epithelial adhesion, limbal stem cell deficiency, trauma, medications and infections. There are several noninvasive treatments for PED, such as autologous serum and topical insulin, the latter having less evidence of its efficacy, until recently. This study demonstrates that topical insulin may actually be the more effective treatment option for this sight-threatening condition.
The retrospective data analysis included 61 patients treated with topical insulin (case group) and 23 treated with autologous serum (control group) for PED resistant to conventional treatment. The researchers sought to determine the percentage of patients who reached epithelization, as well as when and how quickly they did so.
Epithelization was achieved in 51 patients on insulin but only 11 on autologous serum. Re-epithelization also occurred much faster in patients in the insulin group with a mean time of 33 days (range four to 124), while the autologous serum group had a mean time of 83 days (range 13 to 231) until re-epithelization.
Amniotic membrane transplantation (AMT) is a surgical procedure often mandatory for patients whose eyes don’t respond to treatment and face a risk of perforation. This study’s results showed the need for AMT was significantly lower in the insulin group. In addition, PED recurrence was also much less common in patients treated with insulin compared with autologous serum (11% vs. 43%).
“A decrease in the need for AMT with topical insulin should be considered as an important step toward epithelization,” the researchers wrote in their study. “For this reason, we have adopted insulin treatment as a first choice within second-line treatment options, that is, when epithelization is not achieved in two weeks with standard initial treatment. It would also seem to us an effective and valid first line of treatment option to avoid prolonging the re-epithelialization of PED and the appearance of possible associated complications.”
In this dataset, topical insulin presented significantly better epithelization outcomes than autologous serum eye drops. Consider this treatment option for those rare cases of PED you may come across in your practice to help speed up the recovery process and prevent further damage while still achieving optimal visual outcomes.
Diaz-Valle D, Burgos-Blasco B, Rego-Lorca D, et al. Comparison of the efficacy of topical insulin with autologous serum eye drops in persistent epithelial defects of the cornea. ACTA Ophthalmologica. August 18, 2021. [Epub ahead of print]. |

