43rd Annual Technology ReportCheck out the other feature articles in this month's report:- Glaucoma: How to Build a Better Baseline - The Many Uses of Orbital Ultrasonography - Is OCT-A Right For My Practice? |
Getting reimbursed by insurance doesn’t guarantee you won’t be audited—or that you’ll pass if you are. The hard truth is, regardless of how you bill, an audit may be in your future.
Still, you can lower your chances of failing an audit by tightening up your diagnostic testing protocols, which includes knowing what tests are warranted, when they aren’t necessary and how to document for them properly.
Be a Rule Follower
To pass an audit, you must comply with the rules set by each payer (i.e., insurance company), establish medical necessity and document appropriately.
Although some payers’ rules are similar to Medicare, medical necessity rules vary. For each payer, you need to acquire a Local Coverage Determination (LCD) or provider agreement to know which diagnostic tests you can perform and which diagnosis codes are covered.
Diagnostic tests can be done on the same day as an exam/office visit (992XX or 920XX) if both the diagnostic test and exam/office visit are medically necessary.
For certain procedures, such as amniotic membranes, a prior authorization may be necessary from the insurance carrier.
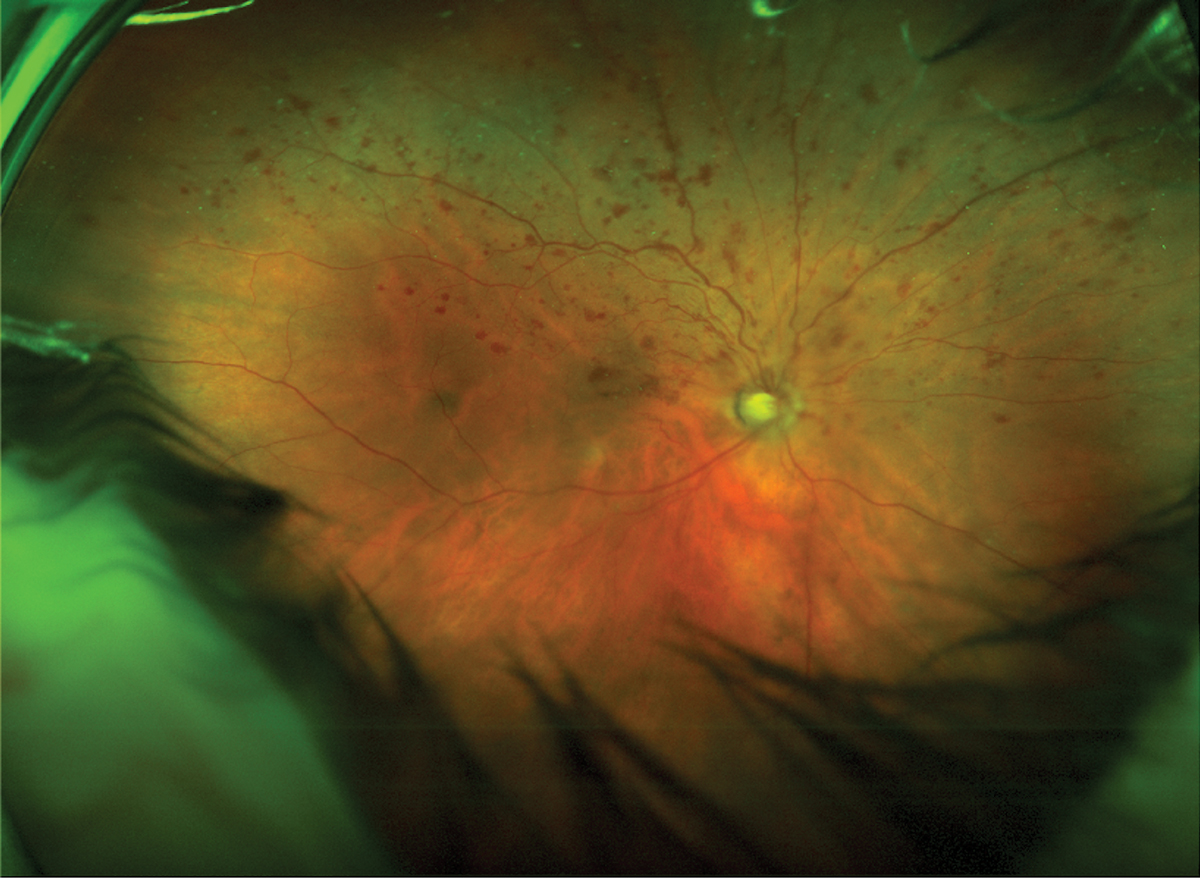 |
| Interpretation and report of widefield imaging taken in office: Clinical findings/diagnosis: H34.8310 tributary (branch) retinal vein occlusion, right eye, with macular edema. |
Ensure Necessity
Claims for diagnostic tests may be rejected if the insurance company determines the test was not medically necessary. A test is only medically necessary if it helps clinical decision-making and management. For example, some insurers may not consider retinal photography for a patient with diabetes without diabetic retinopathy to be useful for decision-making and management, and they may flag the imaging as not medically necessary. On the other hand, photographing diabetic retinopathy over an appropriate period of time to track changes noted after a physical retinal examination helps with clinical decision-making and management and would be considered medically necessary.
The medical necessity of any test must be crystal clear to an auditor. Thus, all documentation in the interpretation and report (I&R) of the patient’s medical record needs to reflect to a potential auditor why the doctor ordered a diagnostic test and how it aided the clinical decision-making and patient management.
Order First, Run Second
Before performing any test, the doctor must first order it. At the end of each exam in my office, we order all of the tests we know will be necessary at the next exam based on what is medically necessary for that case.
For initial exams, unscheduled exams or during the instances when additional testing is necessary the day-of, we will order tests to be performed on that day.
Regardless of the circumstances, you must order and enter tests into the record prior to performing the actual test. Further, you can only interpret the test after it’s completed.
Another must for your records: always sign your test orders. If the test is ordered during an exam record, the doctor’s signature at the end of the exam will suffice. If the test is ordered on a day when the exam is not performed, it’s essential that the doctor still sign the order.
If a patient comes in with vision insurance and needs a diagnostic test billed to their medical insurance, you have three options:
1. Ask the patient for permission to bill the exam and diagnostic test under their medical insurance. It is always the patient’s choice if they want to use their vision insurance if one of their complaints is refractive in nature on a given day. If a patient has both a refractive and a medical complaint, you cannot force them to use their medical insurance for the exam if they have vision insurance.
2. Bill the exam to vision insurance and the diagnostic test to medical insurance using coordination of benefit. With this option, you will have to collect both the vision insurance and medical insurance copays (if there are any) that day.
3. Perform only the exam that day and bill it to vision insurance. Have the patient return on another day to perform the diagnostic test (and maybe an office visit, if medically necessary) and bill it to medical insurance. You will collect the vision insurance copay (if applicable) at the first visit and medical insurance copay (if applicable) at the second visit.
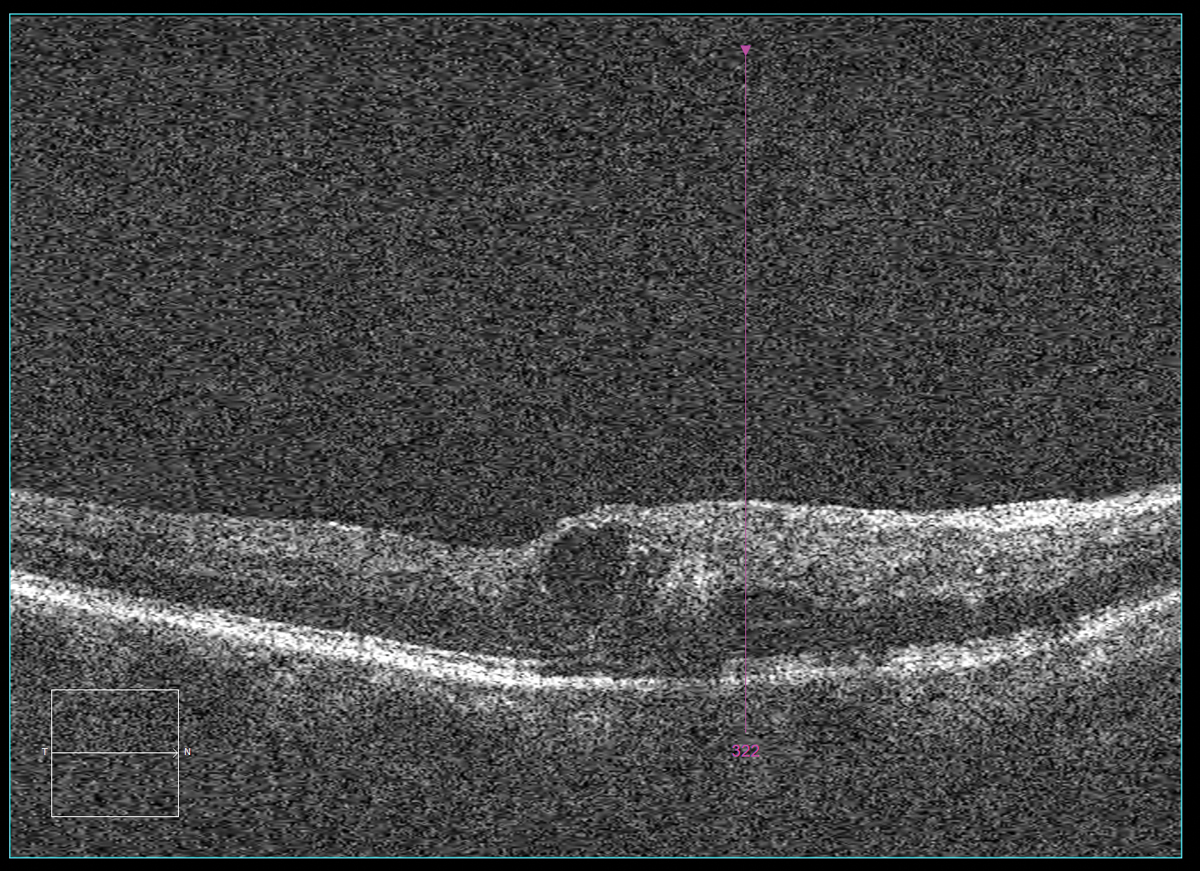 |
| Interpretation and report of OCT performed at the surgeon’s office the next day: Clinical findings/diagnosis: H34.8310 tributary (branch) retinal vein occlusion, right eye, with macular edema. |
Don’t Skimp on Paperwork
Most tests have a global fee that equals the sum of the technical and professional components. Simply put, the technical component covers the cost of equipment, maintenance and technician services. The professional component is the I&R document. This may be very similar to the assessment and plan of the exam and must contain the following:
- Clinical findings/diagnosis
- Reliability of the test
- Comparative data/change in condition
- Clinical management (i.e., how the test affected patient care and physician decision making going forward)
Without the I&R, the provider is not entitled to the full global fee for the test. Whenever a current procedural terminology (CPT) code states “with interpretation and report,” this information must be included in the chart documentation. For example, optic nerve OCT, retinal OCT, visual field and fundus photography all require I&R. However, not all tests have this stipulation. Gonioscopy, for one, does not require an I&R. Also, if you perform more than one test that requires an I&R on a given day, each test will require its own I&R.
Avoid Testing Taboos
Although clinicians order diagnostic tests numerous times on a typical day, misuse of tests and their documentation can be common, regardless of the best of intentions. Here are four red flags to avoid:
1. Don’t perform “screening” photography and then bill the photo to medical insurance if pathology is found. This is inappropriate for two reasons. One, a screening test must be completely different than the test billed to medical insurance (although it can be performed on the same piece of equipment). Two, a test must be ordered before the test is performed.
2. It is only appropriate to bill a patient’s symptom as a diagnosis if you can’t find the cause of the symptom or if the cause of the symptom does not have an ICD-10 code. If the cause of the symptom does not provide reimbursement for the test, it is not appropriate to bill the symptom just to get paid. For example, the diagnosis of external hordeolum (H00.01__) generally does not pay for an external ocular photo (92285). However, edema of the eyelid (H02.84__) generally does pay for an external ocular photo (92285). If your patient has an external hordeolum on their right upper eyelid (H00.011), you cannot use the diagnosis of edema of right upper eyelid (H02.841) to get paid for the external ocular photo. Because the eyelid edema is a symptom of the external hordeolum, it would be wrong to bill for eyelid edema.
3. Don’t enter an incorrect diagnosis into the patient’s chart just to get paid for a test. Not only is that against insurance company rules, but that diagnosis will follow the patient for the rest of their life and can affect insurance coverage and/or premiums in the future.
4. If it doesn’t help with your clinical decision-making and management, don’t repeat a test that was already done at another doctor’s office just because you didn’t get the chance to bill for it.
In instances where you are comanaging a patient with another doctor, you should get a copy of the patient’s records with all tests performed from the comanaging doctor. For example, if a glaucoma surgeon did optic nerve OCT imaging a week earlier and you have a copy of the test, in most cases, it would be inappropriate to repeat the OCT since you wouldn’t normally perform a weekly optic nerve OCT on a glaucoma patient.
On the other hand, if a retina surgeon did a macular OCT two weeks prior on a patient with cystoid macular edema (CME) and then gave the patient an anti-VEGF injection, it may be appropriate for you to repeat the macular OCT two weeks later to confirm the CME has improved or resolved.
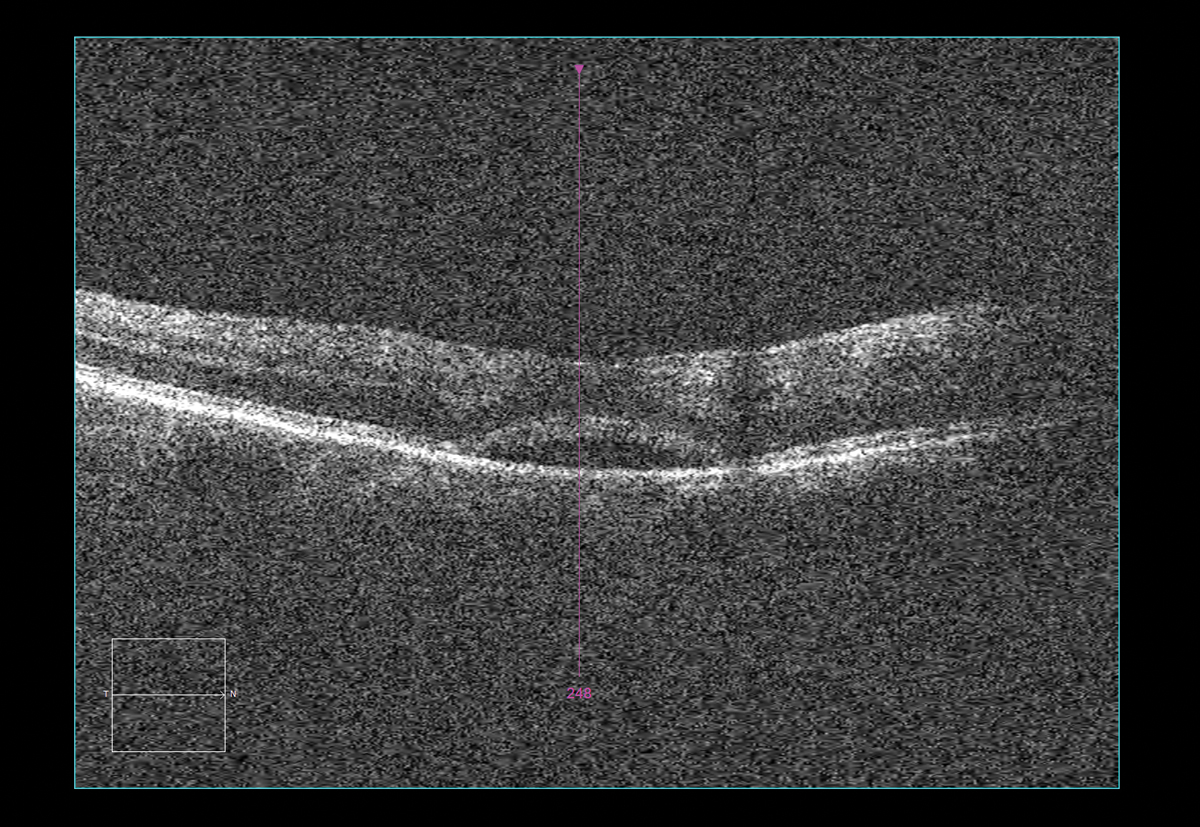 |
| Interpretation and report of OCT performed in office two weeks after anti-VEGF injection: Clinical findings/diagnosis: H34.8310 tributary (branch)retinal vein occlusion, right eye, with macular edema. |
Be Strict with Modifiers
If you perform a bilateral test on one eye only, you must use the -52 modifier and the RT or LT modifier, and payment will be reduced by 50%. The following are commonly performed bilateral tests:
- External photos (92285)
- Topography (92025)
- Gonioscopy (92020)
- Pachymetry (76514)
- Fundus photos (92250)
- OCT, optic nerve (92133)
- OCT, retina (92134)
- Visual fields (92083)
If a unilateral test is performed on both eyes, use the -50 modifier. In this case, you will receive 150% of the unilateral reimbursement.
Structure Same-day Testing
If you are performing multiple diagnostics tests on the same day, you should bill the most expensive test first, since each subsequent test will have a decreased reimbursement.
Remember, certain CPT codes can’t be billed together when performed by the same physician during the same visit on the same day; these are called mutually exclusive. For example, external ocular photography (92285), fundus photography (92250), retina OCT (92134) and optic nerve OCT (92133) will not be reimbursed if they are performed on the same day because they are mutually exclusive. If you want to be reimbursed for mutually exclusive tests, you must perform these tests on different days. In addition, some tests are components of another test, and they cannot be billed separately.
When to use ABN/Waivers
If you have a specific reason you believe a test may be denied, you must use a waiver of liability that states that if the claim is denied, the patient will be fully and personally liable to pay you for the test.
Note: clinicians should never use an advance beneficiary notice (ABN)/waiver to get paid for two or more mutually exclusive tests on the same day.
A waiver of liability will not influence determination of coverage. Some insurance companies have their own waivers. For example, Medicare uses the ABN, while Tricare has its own waiver and will not honor any others.
When in doubt, have the patient sign a waiver.
Dr. Scott Moscow is the clinical director of Roswell Eye Clinic in Roswell, GA, where he focuses on fitting specialty contact lenses and treating eye disease. In addition to lecturing, he consults on billing and coding, including for specialty contact lenses and vision therapy.

