 |  |
How often had you had a patient tell you about their vitreous opacities (VO)—a.k.a. floaters—and ask if there are any treatments available? We get this from patients daily. To ease their concern, we perform a thorough dilated examination and educate them about their condition and why they have VOs. Whether acute or chronic, our role is to explain the reason for floaters and to check for any retinal pathology like retinal breaks or detachment.
In the past, our discussions focused mainly on patient reassurance that their symptoms will resolve over time and the brain will adapt and ignore them (neuroadaptation) over the next several weeks to months. Unfortunately for some patients, VOs can be incredibly debilitating and have a significant impact on their quality of life. Because patients are willing to try anything to get rid of their floaters, they will search the internet high and low for various treatment options, from homeopathic remedies to in-office laser vitreolysis.
Although there are reports that laser vitreolysis is successful, clinical research and experience remain limited. The retina specialists we work with have not adopted the procedure and instead perform pars plana vitrectomy—a safe and viable option for patients with VOs.
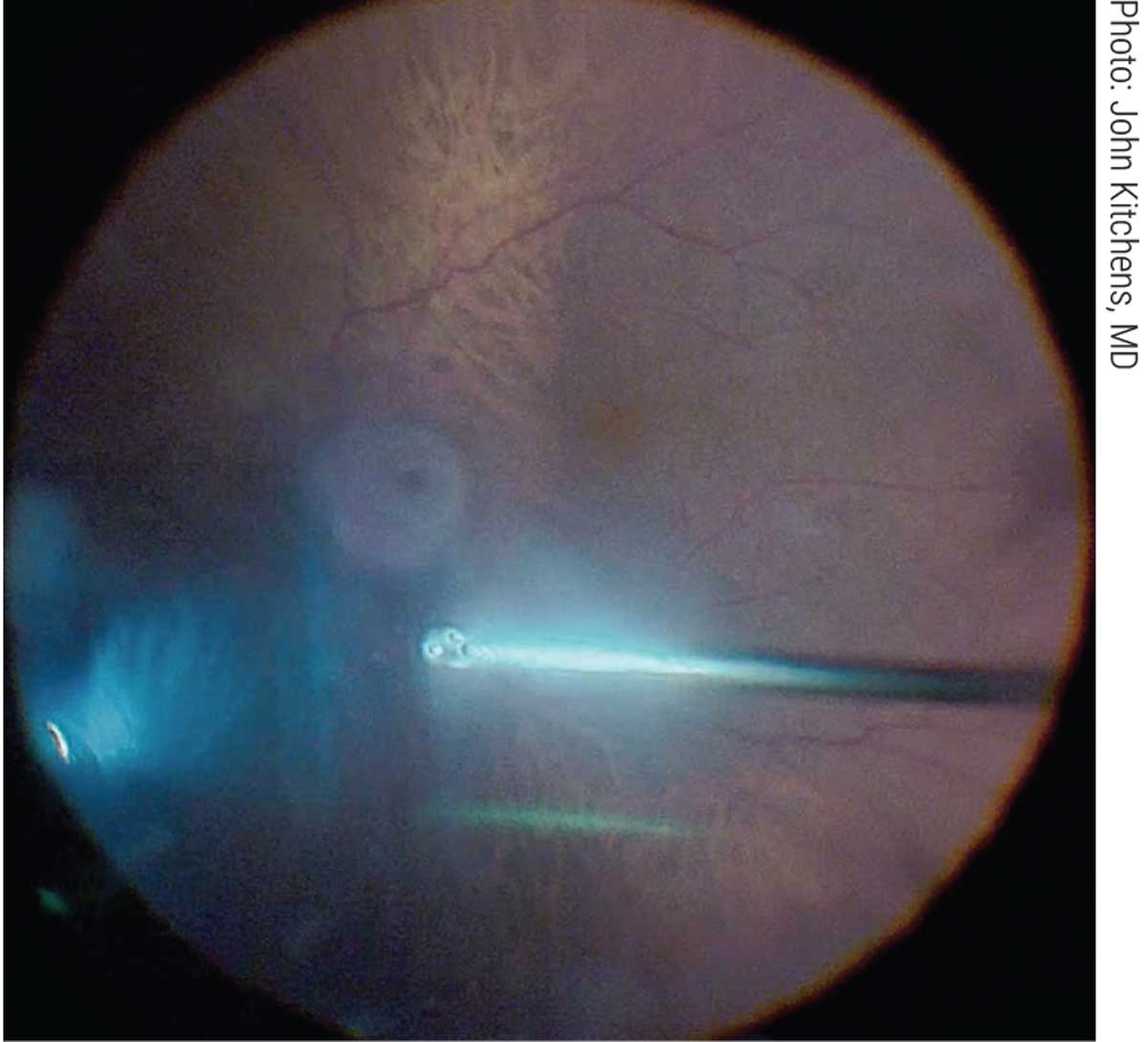 |
| When surgical intervention is needed, pars plana vitrectomy is the best option. Click image to enlarge. |
What Are VOs?
Familiar to all eye doctors, vitreous opacities are small dark shapes that float across your vision. Vitreous hemorrhages, pigmented cells and inflammatory cells are also VOs. Risk factors include age, nearsightedness, trauma, complications from cataract surgery, diabetic retinopathy and eye inflammation.
Although most patients do not require surgical intervention, the main indications for surgery include symptomatic decrease in quality of vision and life (e.g., can’t read, drive) and/or symptomatic VO is greater than six months. Patients who are pseudophakic are optimal candidates compared to phakic candidates due to the development of cataracts post-vitrectomy. Anecdotally, patients with multifocal intraocular lenses seem more bothered by VOs.
As with any ocular surgery, communication is key. Discuss with your surgeon their thoughts on when it is appropriate to perform a vitrectomy, which will help prepare patients for the referral to the retina provider.
Pars Plana Vitrectomy
Prior to surgery, patients receive a local retrobulbar injection to ensure good anesthesia is obtained. Next, the eye is prepped and draped in the usual sterile fashion. A 27-gauge 4mm infusion cannula is placed 3.5mm from the limbus inferotemporally. After confirming the position of the cannula, two superior 27-gauge sclerostomies are placed. Then, the vitrectomy device and light pipe are inserted. The surgeon identifies the VOs and begins a standard three-port pars plana vitrectomy to clear the opacities. Once complete, a 360° scleral depression is performed at the end of the case to ensure no breaks were noted. The last step is to remove the trocars and cannulas and ensure the eye is watertight. A subconjunctival injection of steroids and antibiotics is administered followed by patching/shielding the eye.
As with any ocular surgery, risks include cataract formation, retinal tear and detachment, macular pucker, macular edema and endophthalmitis. Typical postoperative visits are one day, one week and one month after the procedure.
So, next time you have a symptomatic patient complaining about floaters, consider a referral for a vitrectomy. With significant advances in technology, we are able to help improve our patients’ vision and tackle those pesky floaters.
Drs. Cunningham and Whitley wish to thank Rohit Adyanthaya, MD, for his contributions to this month’s discussion.
Dr. Cunningham is the director of optometry at Dell Laser Consultants in Austin, TX. He has no financial interests to disclose.
Dr. Whitley is the director of professional relations and residency program supervisor at Virginia Eye Consultants in Norfolk, VA. He is a consultant for Alcon.

