
A 53-year-old white female presented to her optometrist one week earlier for her first-ever eye exam. The O.D. noted atypical fundus changes and referred her to us for evaluation. This was her first dilated eye exam. Medical and ocular history were unremarkable.
At this visit, the patients uncorrected visual acuity was 20/25 O.D. and 20/50 O.S. Pinhole improved her acuity to 20/20 O.U. Pupils were equally round and reactive, with no afferent pupillary defect. IOP was normal O.U. There was mild nuclear sclerosis O.U.
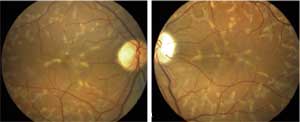 | |
| 1, 2. Color fundus photos (O.D. left, O.S. right) revealed healthy optic nerves and atypical fundus lesions throughout the posterior pole and periphery. | |
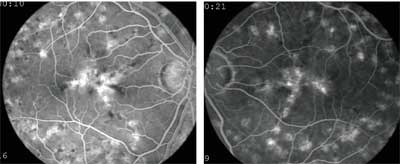 | |
| 3, 4. Fluorescein angiography (O.D. left, O.S. right) showed diffuse staining of the lesions.The patient does not have a quiet choroid, and the background choroidal fluorescence is considered normal. |
Take the Retina Quiz
1. What is the most likely diagnosis for this patient based on the fundus appearance and fluorescein angiogram?
a. Stargardts disease.
b. Pattern dystrophy.
c. Dominantly inherited drusen.
d. Cone-rod dystrophy.
2. How would you best describe the fluorescein appearance?
a. Normal.
b. Normal background staining appearance with diffuse staining of the lesions.
c. Quiet choroid with diffuse staining of the lesions.
d. Atrophic macular changes with associated choroidal neovascularization (CNV).
3. This patient can expect her vision to:
a. Rapidly decrease during the next few months.
b. Rapidly decrease during the next few years.
c. Rapidly decrease to less than 20/400.
d. Slowly decrease or remain unchanged.
4. The best treatment for this patient is:]
a. Photodynamic therapy for the fundus lesions.
b. Intravitreal Lucentis (ranibizumab, Genentech).
c. Cataract surgery.
d. Observation and education.
5. Other testing for this condition can include:
a. Color vision testing.
b. Visual field testing.
c. Electro-oculogram.
d. All of the above.
For answers, see below.
Discussion
Based on the patients fundus appearance, we initially suspected an atypical form of Stargardts macular disease (SMD), also known as fundus flavimaculatus. Stargardts disease is the most common hereditary dystrophy and is commonly inherited as an autosomal recessive disorder. Patients who have this condition commonly experience vision loss in childhood, with vision deteriorating to 20/80 to 20/200 by the third decade.1
Patients who have SMD may have yellow fishtail, or pisciform, flecks in the posterior pole that may extend into the periphery. Patients may also exhibit changes within the macula that result in a beaten bronze appearance.
SMD is considered a lipofuscin storage disease, meaning that patients have an increased deposition of lipofuscin at the level of the retinal pigment epithelium (RPE). This can result in a vermillion, or deep red, fundus appearance.
Fluorescein angiography is usually diagnostic for SMD, as it will show blockage of the choroidal fluorescence due to the lipofuscin. This is referred to as a quiet choroid.
Interestingly, our patient does not have a quiet choroid. In fact, the background choroidal fluorescence in our patient would be considered quite normal. So what else could this be?
Our patient is in her fifth decade with best-corrected vision of 20/20. She has no complaints of decreased vision, and there is no family history of blindness or eye disease.
Based on the patients history, clinical findings and fluorescein staining pattern, we diagnosed multifocal pattern dystrophy simulating Stargardts disease.
Multifocal pattern dystrophy is considered to be one of the five forms of dominant pattern dystrophies. The five forms that have been identified are labeled based on their peculiar shape or clinical appearance. These include:1
Adult-onset foveomacular vitelliform dystrophy (group 1). Lesions in this group can simulate the lesions that are commonly seen in juvenile Bests disease.
Butterfly-shaped pigment dystrophy (group 2). This form is characterized by yellowish flecks that concentrate in the macula and may spread throughout the posterior pole. As the name suggests, they can simulate the appearance of a butterfly.
Reticular dystrophy of the RPE (group 3). This form of the disease can have more of a reticulated fishnet appearance in which the RPE changes are more contiguous with one another.
Multifocal pattern dystrophy simulating fundus flavimaculatus (group 4). These patients show the pisciform changes that are commonly seen in SMD, but they do not show angiographic evidence of a dark choroid.1,2
Fundus pulverulentus (group 5). Patients with this form show prominent, coarse, punctiform mottling of the RPE in the macular area.1
With all the forms of pattern dystrophy, patients have mild to minimal visual changes with onset between 20 and 50 years of age. CNV may develop.
Additional testing may include color vision testing, which is normal; Amsler grid testing, which may reveal a central scotoma; and an electro-oculogram, which may be subnormal. On subsequent visits, our patients color vision and Amsler grid testing were normal.
We educated the patient about her condition but did not recommend any treatment. Her vision has remained unchanged during the past four years.
Other family members have since received dilated fundus exams with her referring optometrist. The findings were normal. Our patient now has regular exams with her referring optometrist and returns to our office as needed.
This case was co-written by George Meers, O.D., who is in private practice in Tacoma, Wash.
Retina Quiz Answers: 1) b; 2) b; 3) d; 4) d; 5) d.
1. Gass JDM. Autosomal Dominant Pattern Dystrophies of the RPE. Stereoscopic Atlas of Macular Disease. 4th ed. St. Louis: CV Mosby Co.,1998:322-32.
2. Lopez PF, Aaberg TM. Phenotypic similarities between Stargardts flavimaculatus and pattern dystrophies. Aust N Z J Ophthalmol 1992 Aug;20(3):163-71.

