A 51-year-old white female had sudden vision loss in her left eye. She came into our clinic the next day.
Her best-corrected visual acuity was 20/200 with a grade 4+ vitreous hemorrhage in the left eye. Ultrasonography confirmed a retinal break. We referred her to a retinal specialist who performed a pars plana vitrectomy with laser photocoagulation encircling the flap tear.
We diagnosed this 51-year-old white female with a retinal break. A retinal specialist performed a pars plana vitrectomy with laser photocoagulation encircling the flap tear.
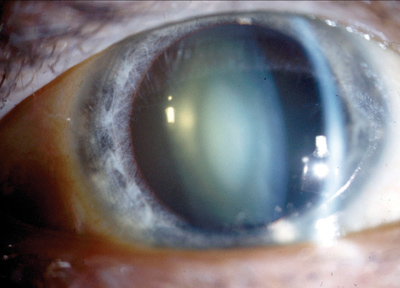
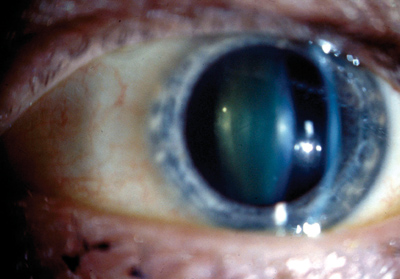
Three months later, the patient presented with this appearance.
Diagnostic Data
An examination with refraction demonstrated a 3.25D increase in myopia O.S. The ocular findings in the left eye are demonstrated in the photograph.
The patients external examination was normal, and there was no evidence of afferent pupillary defect. Anterior segment structures were normal. Applanation intraocular pressures measured 15mm Hg in both eyes.
Your Diagnosis
How would you approach this case? Does this patient require additional tests? What is your diagnosis? How would you manage this patient? What is the likely prognosis?
Discussion
The diagnosis in this case is increased myopia induced by retinal repair and pars plana vitrectomy along with the formation of a post-vitrectomy cataract.
Several studies have demonstrated that nuclear cataracts are associated with increased oxidative damage to the proteins and lipids of the oldest cells in the lens.15 Up to 80% of older patients who undergo vitrectomy exhibit changes in the lens that cause a myopic shift and nuclear cataracts within two years.
Until recently, the mechanisms for this have been poorly understood. Recent research points to a plausible explanation.1 Investigators note that the back surface of the lens normally exists in a low-level oxygen environment because the intact vitreous blocks oxygen from reaching this area, which minimizes oxidative damage. But when the vitreous is removed (partially or totally) and replaced (albeit temporarily) with a saline solution (which is comparatively high in oxygen content), the lens becomes opacified as a reaction to its exposure to increased oxygen levels.1
As vitrectomy surgery naturally induces an enhanced and rapid oxidative change, this mechanism makes sense. Indeed, patients older than 50 and those who receive intravitreal gas bubbles are more likely to form nuclear cataracts within one to two years.6
For the patient in this case, the cataract was removed to provide a final good visual outcome. The retinal detachment repair has remained intact without complications.
Thanks to Matthew J. Garston, O.D., of Cambridge, Mass., who contributed this case.
1. Harocopos GJ, Shui YB, McKinnon M, et al. Importance of vitreous liquefaction in age-related cataract. Invest Ophthalmol Vis Sci 2004 Jan;45(1):77-85.
2. Sawa M, Saito Y, Hayashi A, et al. Assessment of nuclear sclerosis after nonvitrectomizing vitreous surgery. Am J Ophthalmol 2001 Sep;132(3):356-62.
3. Saito Y, Lewis JM, Park I, et al. Nonvitrectomizing vitreous surgery: a strategy to prevent postoperative nuclear sclerosis. Ophthalmology 1999 Aug;106(8):1541-5.
4. Melberg NS, Thomas MA. Nuclear sclerotic cataract after vitrectomy in patients younger than 50 years of age. Ophthalmology 1995 Oct;102(10):1466-71.
5. Palmquist BM, Philipson B, Barr PO. Nuclear cataract and myopia during hyperbaric oxygen therapy. Br J Ophthalmol 1984 Feb;68(2):113-7.
6. Thompson JT. The role of patient age and intraocular gases in cataract progression following vitrectomy for macular holes and epiretinal membranes. Trans Am Ophthalmol Soc 2003;101:485-98.

