 |
 |
The role of the OD is pivotal in achieving the best possible outcomes through careful pre-op care.
Ocular Surface Quality
The first and most important rule is to remember that the results of any refractive surgical procedure will depend heavily on the quality of the ocular surface. Surgery should not be considered until the ocular surface is in good shape or stabilized with treatment. A compromised ocular surface will limit patients’ intraocular lens options. Ocular surface disease will increase the risk of surgical complications, affect IOL measurements (e.g., biometry, keratometry) and impact patient comfort and quality of vision.
|
|
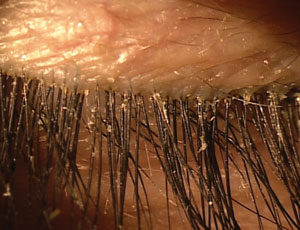
| Untreated blepharitis could diminish the outcome of an otherwise routine cataract surgery. Be sure to treat it preoperatively. |
|
Accurate keratometry readings are critical for refractive success—these measurements become highly variable in a patient with a poor ocular surface. Preoperative ocular surface issues that could affect surgery include the following:
• Blepharitis. For a condition that is among the most significant causes of postoperative symptoms, blepharitis is still routinely overlooked.1 Explain to these patients that they have a chronic condition that will need to be treated before surgery.
Treat any amount of lid margin inflammation or gland secretion turbidity. Preoperative treatments may include combination antibiotic/steroid drops, topical azithromycin and oral tetracycline analogs along with lipid-based tear supplements. Long-term management includes pulse-dosing steroids, warm compresses and lid scrubs, low-dose tetracycline analogs and oral omega-3 supplementation.
• Dry eye. There’s no question that moderate to severe dry eye is a contraindication to refractive surgery, but for many patients even mild dry eye warrants attention, as it is often unavoidable. For at-risk patients such as women and those of advanced age, begin prophylactic pharmacological treatment (such as topical anti-inflammatories) in addition to omega-3 and artificial tears. This will also hold true for asymptomatic patients with low tear prism height and anyone with mild superficial punctate corneal staining. Topical steroids can speed healing preoperatively, but are typically not used long term after surgery. For chronic dry eye, cyclosporine, nutraceuticals and punctal occlusion may be necessary.
• Allergy. Although allergic conjunctivitis patients typically control symptoms with an antihistamine/mast cell stabilizer eye drop, treating ocular allergy with topical corticosteroids in the perioperative period should be considered. Steroids will shut down the entire inflammatory cascade, creating a better environment for surgery and ensuring good control of moderate allergy. In the immediate postoperative period, antihistamine drops are then initiated based on need.
Treat Early, Treat Often
A poor tear film will decrease contrast sensitivity and lead to inconsistent vision.2
Attempting to only begin treatment postoperatively can be a fruitless task because of neuropathy-related decreased tear production.
Running into just a couple of these problem patients after surgery will forever change your attitude about treating any amount of pre-existing ocular surface disease.
1. Levinson BA, Rapuano CJ, Cohen EJ, et al. Referrals to the Wills Eye Institute Cornea Service after laser in situ keratomileusis: reasons for patient dissatisfaction. J Cataract Refract Surg. 2008 Jan;34(1):32-9. 2. Huang FC, Tseng SH, Shih, MH, Chen FK. Effect of artificial tears on corneal surface regularity, contrast sensitivity, and glare disability in dry eyes. Ophthalmology. 2002 Oct;109(10):1934-40.
