 |
A 57-year-old female presented for evaluation of possible diabetic retinopathy. She has had poorly controlled diabetes for 12 years and currently is on Januvia (sitagliptin, Merck) and insulin. Her hemoglobin A1c was 9.0 a month earlier. She reported that the vision in her right eye has been poor for more than 10 years, but sees well out of her left eye.
On examination, her best-corrected visual acuities measured 20/40 OD and 20/20 OS. Confrontation visual fields were full-to-careful finger counting in both eyes. Her ocular motility testing was normal and her pupils were equally round and reactive without an afferent pupillary defect. Her anterior segment was unremarkable. Tensions by applanation measured 17mm Hg OU.
On dilated fundus exam, her optic nerves appeared healthy with a small cup and good rim coloration and perfusion in both eyes. Examination of the macula in the right eye showed obvious changes (Figure 1). Close inspection of the left eye also shows subtle findings (Figure 2). Spectral-domain optical coherence tomography (SD-OCT) was also performed (Figures 3 and 4) and OCT angiography (OCT-A) of the right eye is also available for review (Figure 5).
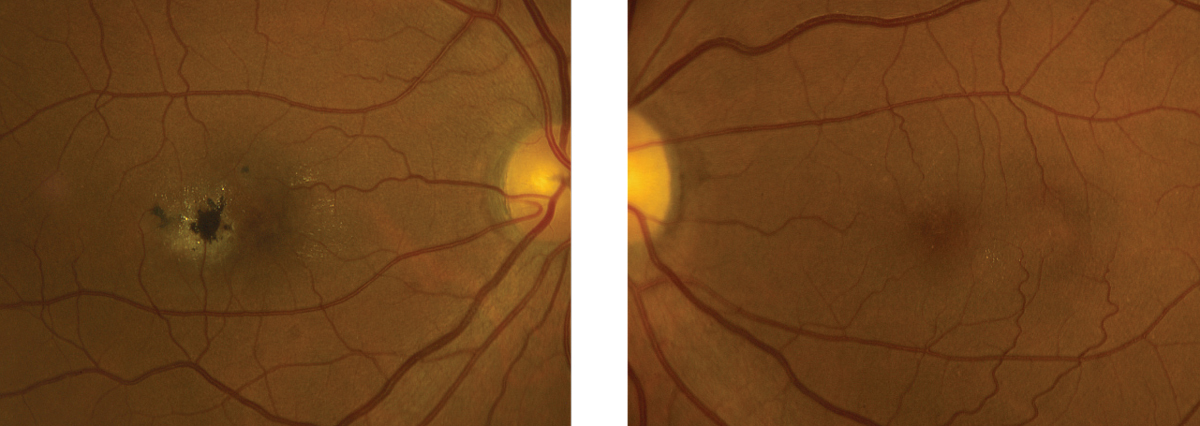 |
| Figs. 1 and 2. This is the right and left eye of our patient. Note the pigment changes seen in the right eye. But don’t ignore the left eye—what do you see? Click images to enlarge. |
Take the Retina Quiz
1. What do the small white spots that are visible in the right eye represent?
a. Drusen.
b. Exudate.
c. Retinal crystals.
d. Talc.
2. What is the essential finding on the SD-OCT in the right eye?
a. Choroidal neovascularization.
b. Center-involved diabetic macular edema.
c. Cystoid macular edema.
d. Scaring and parafoveal loss of the IS/OS Junction.
3. What is the essential finding on the SD-OCT of the left eye?
a. The OCT is normal.
b. Cystoid macular edema.
c. Internal limiting membrane drape.
d. Subretinal fluid.
4. What is the correct diagnosis?
a. Macular telangiectasia.
b. Mild nonproliferative diabetic retinopathy.
c. Chorioretinal scar from toxoplasmosis.
d. Retinal detachment.
5. How should this patient be managed?
a. Observation.
b. Observation right eye, anti-VEGF treatment left eye.
c. Anti-VEGF therapy both eyes.
d. Pars plana vitrectomy, membrane peel.
For answers, see below.
Diagnosis
We observed an obvious large plaque of retinal pigment hyperplasia adjacent to the macula in the right eye with parafoveal loss of the inner segment/outer segment (IS/OS) junction. We observed no subretinal fluid, nor a choroidal neovascular membrane. With direct comparison of the SD-OCT, the bright intraretinal hyperreflective spot on the OCT represents the retinal pigment epithelial (RPE) hyperplasia, which is blocking the transmission signal posterior to the plaque. Remarkably, our patient is still able to see 20/40 OD. That should not be a big surprise because, on close evaluation of the OCT, the IS/OS junction at the fovea is intact.
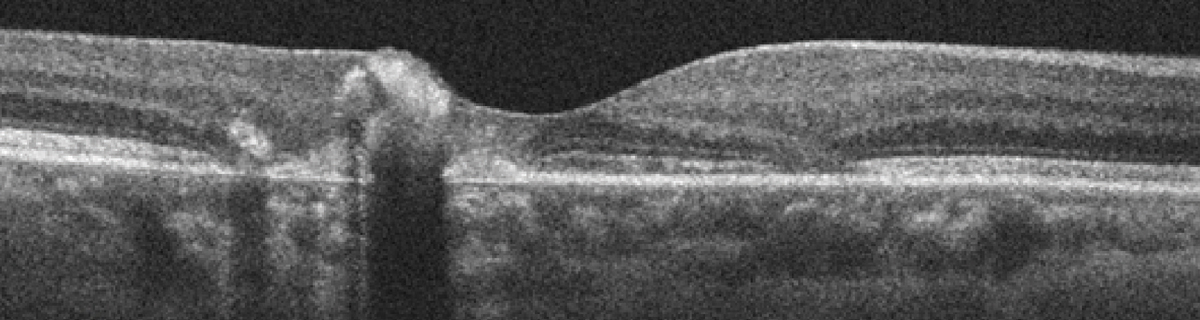 |
| Figs. 3 and 4. This represents the SD-OCT of the right and left eye. Note the changes within each macula. Click images to enlarge. |
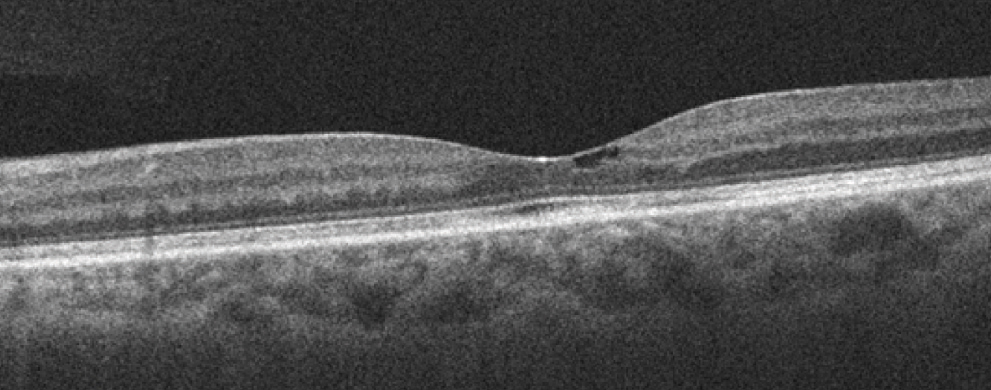 |
The other interesting findings in the right eye were small refractile white deposits scattered throughout the macula. They appeared to be intraretinal and represent small crystalline deposits. Of particular interest were intraretinal crystals in the left eye. What’s more, the SD-OCT in the left eye is also quite revealing. Slightly temporal to the macula is what appeared to be a small pocket of fluid or perhaps a small retinal cyst. What this represents is an internal limiting membrane drape.
All these findings are typical for macular telangiectasia (MacTel).
Discussion
MacTel can be autosomal dominant but with reduced penetrance.1 MacTel is divided into two main types. Type 1 is categorized as macular aneurismal telangiectasia and type 2 as macular perifoveal telangiectasia.1-2 Our patient has type 2. In type 1, patients are more likely to have obvious vascular changes with more pronounced aneurismal dilations and cystoid macular edema. Type 2 patients will have minimal exudation and a central lamellar cyst with a “draping” of the retina over the central cystic, which is seen in the left eye of our patient on the OCT. In addition, type 2 patients will have loss of the retinal transparency and more subtle telangiectatic changes within the capillaries. This can be seen on the OCT-A in the right eye of our patient temporal to the macula. These subtle telangiectatic vascular changes were not as obvious on the OCT-A in the left eye but they were present.
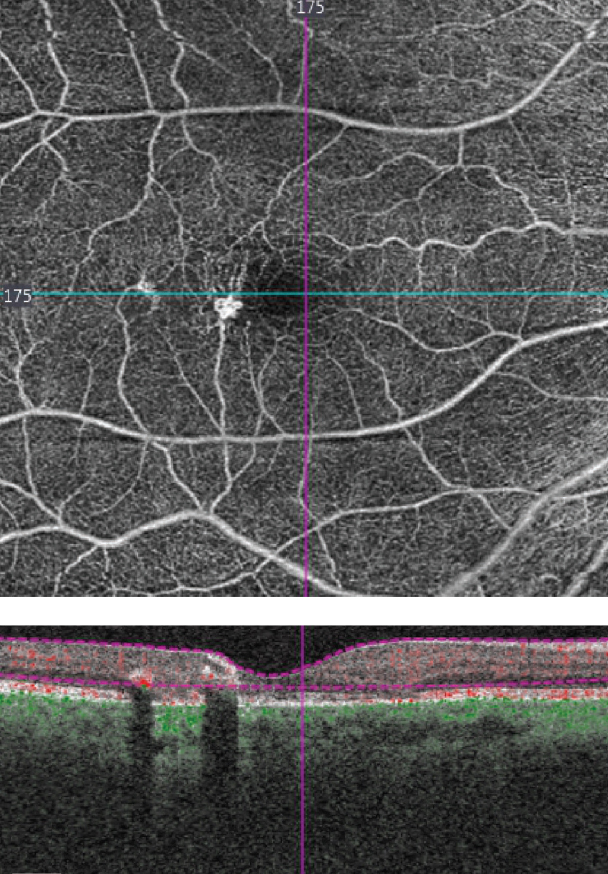 |
| Fig. 5. This OCT-A shows our patient’s right eye. |
Another subtle finding in the left eye is how the retinal veins temporal to the macula appear to be blunted or come to an abrupt stop. What’s happening is that the veins are making a right angle turn and “diving” posterior into the macula. We can’t see this in the right eye because of the plaque of pigment, which is also characteristic for the late stages of MacTel.
Most patients will develop these plaques of intraretinal pigment over time. It’s usually not as extreme as what is seen in our patient. This may be in response to a chronic incompetence of the retinal capillaries, which results in slow leakage and atrophic changes in the photoreceptor layer.1 This stimulates the pigment to migrate from the RPE and extend into the sensory retina. The pathophysiology may be similar to bone spicule-like pigmentation that is in retinitis pigmentosa.1
Patients can also develop choroidal neovascularization, which can also result in scaring and RPE hyperplasia. We were not sure why the pigment was so dense in the right eye of our patient and was not present at all in the left eye. Perhaps she had a CNV at one point in time. Remember, our patient said the vision in the right eye had been reduced for more than 10 years.
In this case, our patient’s MacTel was stable and required no treatment. Of concern was a history of concurrent poorly controlled diabetes. Even though she did not have diabetic retinopathy, she is at risk because of her elevated blood sugar levels. She was counseled on the importance of tighter control of her blood sugar and asked to return for follow-up in six months.
1. Hayreh SS, Zimmerman MB. Amaurosis fugax in ocular vascular occlusive disorders: prevalence and pathogeneses. Retina. 2014;34(1):115-22. |

