 |
Q: I recently saw a patient with a significant Pseudomonas ulcer in which the edge had reached the limbus. The ulcer is 3.5mm by 4mm with at least 50% thinning. The corneal specialist added an oral antibiotic. Is this necessary, and what might the best option be drug-wise?
A: “There is no data that specifically supports how much of an oral antibiotic reaches the ocular surface,” Paul Karpecki, OD, of Koffler Vision Group, says. “That being said, there is also no data to say that it won’t help the ocular surface.” In the case of an aggressive Pseudomonas ulcer, oral antibiotics are worth considering despite their unknown distinct impact on the cornea. Besides providing added antibiotic coverage, many oral antibiotics also carry anti-inflammatory properties and, since a topical steroid would be contraindicated in this case, the oral medication could be used to help manage inflammation.
Certain corneal ulcer situations—such as ones carrying the potential for endophthalmitis, in the case of concurrent treatment for systemic diseases like gonorrhea, or if the infection spreads to the sclera—necessitate the use of oral antibiotics, Eric Donnenfeld, MD, of Ophthalmic Consultants of Long Island and Connecticut, says.
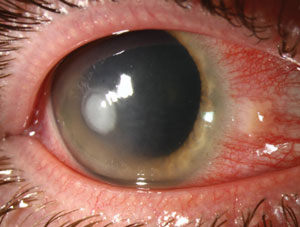 | |
| Pseudomonas ulcers, like the one pictured here, must be aggressively treated to prevent permanent corneal damage. Photo: Christine W. Sindt, OD. |
In this particular instance, “the progression of isolated infectious keratitis toward the limbus suggests that the infection has been undertreated or incorrectly treated and is associated with a poor prognosis,” says James P. Dunn, MD, director of the uveitis unit at Wills Eye Hospital. Patients with this presentation often require enucleation or evisceration.1 Thus, Dr. Dunn explains, it is critical to treat such infections aggressively using culture and sensitivity results as a guide; however, he suggests keeping in mind that P. aeruginosa in particular is extremely difficult to remove once it invades the avascular scleral lamellae. Debridement, scleral wall resection and patch grafting can be used in severe cases.2 He adds that residual scleromalacia is typical.
James Aquavella, MD, of the University of Rochester Medical Center, recommends the use of fortified topical antibiotics—specifically tobramycin 15mg/ml every hour around the clock alternating with cefazolin 50mg/ml. “If there is threatened perforation, systemic drugs may have a place, but even here I prefer a surgical approach with intracameral antibiotics,” he adds.
In agreement, Dr. Dunn notes the use of combination intravenous ceftazidime and gentamicin in addition to topical antibiotics may be more effective than treatment with a single intravenous agent.3 Subconjunctival aminoglycosides may also be beneficial.4 Regarding oral antibiotics, he says, fluoroquinolones and imipenem do seem to achieve good intraocular penetration and may be as effective as intravenous antibiotics, though controlled studies are not forthcoming.
1. Reynolds MG, Alfonso E. Treatment of infectious scleritis and keratoscleritis. Am J Ophthalml. 1991 Nov 15;112(5):543-7.2. Cunningham MD, Alexander JK, Matoba AY, et al. Management and outcome of microbial anterior scleritis. Cornea. 2011 Sep;30(9):1020-3.
3. Helm CJ, Holland GN, Webster RG Jr., et al. Combination intravenous ceftazidime and aminoglycosides in the treatment of pesudomonal scleritis. OphthalmologY. 1997 May;104(5):838-43.
4. Smith TC, Lee GA. Conservative management of pseudomonal infectious sclerokeratitis. Clin Exp Optom. 2008 May;91(3):319-21.

