 |
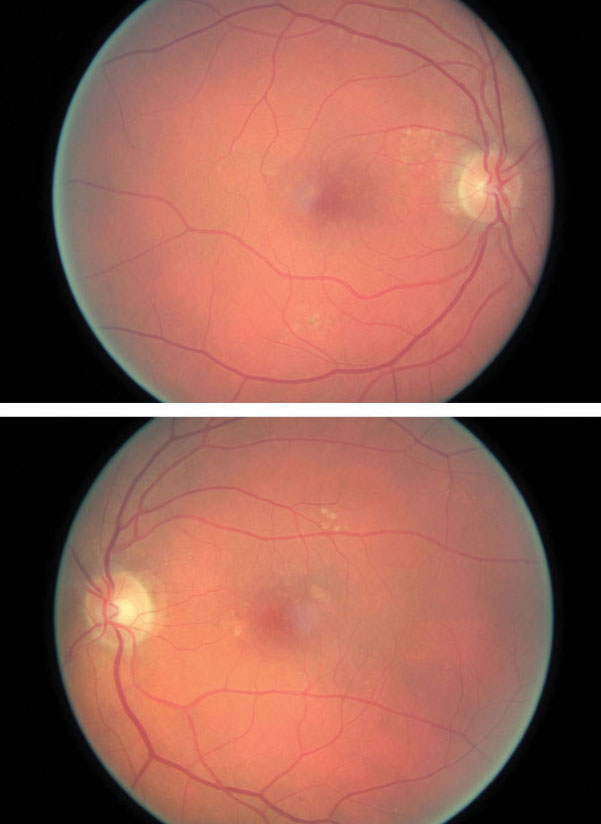
| AMD patients are at an increased risk of submacular hemorrhages. Photo: Amanda Legge, OD. Click image to enlarge. |
A common secondary finding in patients with neovascular age-related macular degeneration (nAMD) is submacular hemorrhage (SMH), typically located subretinally. It has a reported prevalence of 19% to 62% in patients who present with new nAMD. A group of researchers recently compared the demographics, visual acuity and retinal morphology of untreated nAMD patients from the IVAN study with and without SMH and found several similarities among those who develop the condition.
The IVAN study involved a total of 605 trial participants from 23 UK hospitals, 535 of which were included in the results of this analysis (average age: 78). Each participant completed 12 to 24 months of follow-up and underwent comprehensive imaging, including at baseline to determine type, position and extent of SMH. Through random assignment, participants each received one of the following treatments: monthly ranibizumab, as-needed ranibizumab, monthly bevacizumab or as-needed bevacizumab.
At baseline, more than half (53%) of the total participants had SMH present, and 68% of hemorrhages were subretinal. Of all baseline SMH, 89% were smaller than 2.5mm, and those that were intraretinal (14% of 535) tended to be the smallest.
Further observations based on patients with SMH include the following:
About 78% of SMH were within a 1mm radius of the fovea, and 39% involved the foveal center.
Only 8% of baseline SMH occupied more than half of the nAMD lesion area.
Most cases of SMH (70%) resolved within three months.
Patients with SMH were more likely to be older, have intraretinal fluid present and have a worse baseline best-corrected visual acuity (BCVA) with an estimated difference of six letters. However, by month 12, BCVA had improved for patients with and without SMH and was no longer associated with hemorrhage presence.
“Some degree of SMH is a common finding in patients with nAMD and is associated with worse baseline visual acuity,” the authors of the study wrote. “The occurrence of SMH at baseline is associated with older age and the presence of intraretinal fluid, which are both non-modifiable risk factors.”
The important takeaway from the analysis of this dataset is that although these submacular hemorrhages affect a large portion of patients with nAMD, the treatments available today prove to be successful. “Patients with the level of SMH included in this analysis can respond well to anti-VEGF treatments, and after 12 to 24 months of treatment, the negative effect of baseline SMH on BCVA was no longer significant,” the authors concluded.
Mehta A, Steel DH, Muldrew A, et al. Associations and outcomes of patients with submacular haemorrhage secondary to age-related macular degeneration in the IVAN trial. Am J Ophthalmol. September 27, 2021. [Epub ahead of print]. |

