 |
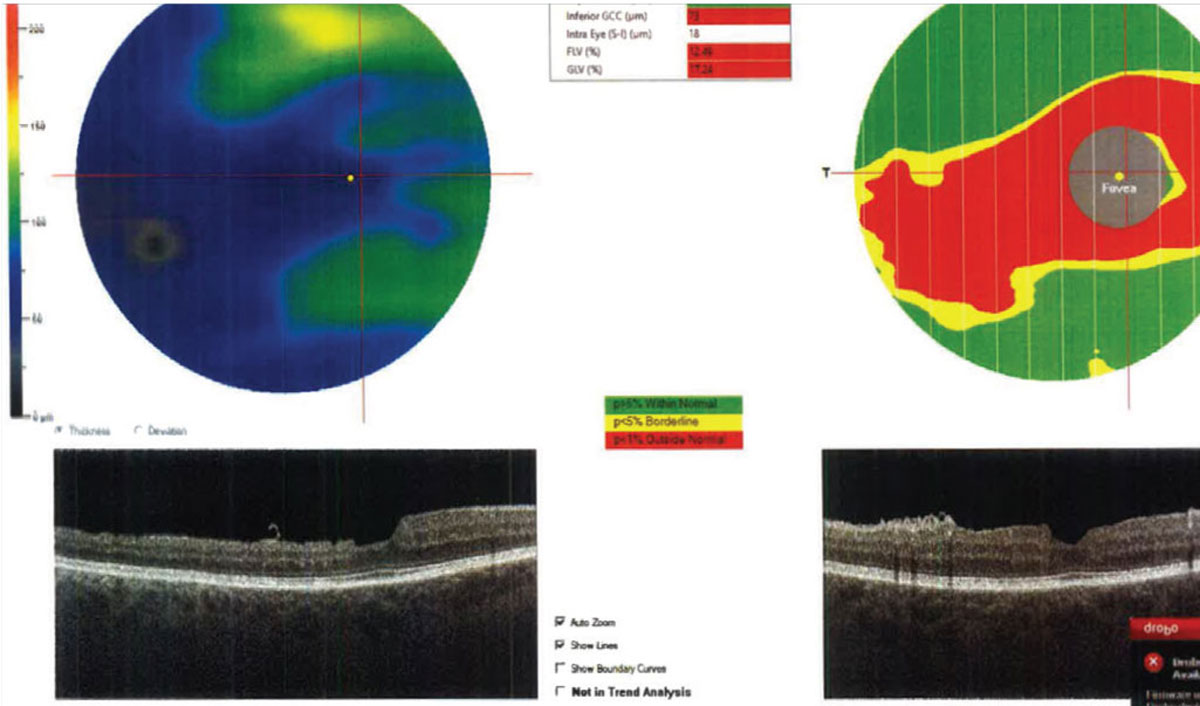
| Macular ganglion cell complex thickness on OCT helps predict glaucoma progression. Photo: Julia Reimold, OD, and Chris Wroten, OD. Click image to enlarge. |
Researchers recently demonstrated that macular ganglion cell complex (GCC) thickness on OCT is a strong measure for detecting structural change in eyes with moderate to severe glaucoma. They compared GCC thickness with other macular measures to see whether it provided a stronger change signal regardless of glaucoma severity, and found it was the optimal measure.
Their prospective cohort study included 112 eyes with moderate to severe glaucoma at baseline. In each 3°x3° macular superpixel, the researchers fit a hierarchical Bayesian random intercept and slope (RIAS) model with random residual variance to longitudinal full macular thickness (FMT), outer retina layers (ORL), GCC, ganglion cell/inner plexiform layer (GCIPL) and ganglion cell layer (GCL) measurements. They estimated individual-level and population-level slopes and intercepts.
“This model [RIAS] more efficiently estimates individual and population rates of change compared with simple linear regression on data from one eye,” the authors explained in their paper. “The RIAS model estimates population means and population standard deviations of the baseline thickness and slopes (i.e., rates of change) and the correlation between superpixel-specific baseline thickness estimates (intercepts) and corresponding slopes. Additionally, the Bayesian paradigm can easily incorporate non-standard features in the data such as differing residual variances between subjects.”
They compared the proportions of significant worsening and improving superpixel slopes between layers, as well as in superpixels with mild or moderate vs. severe damage, where the total deviation of corresponding visual field location was ≥-8dB vs. <-8dB. “This is a topic of significant clinical interest, as various OCT devices use different anatomical outcome measures to determine glaucomatous damage within the macular region,” they pointed out in their study. “While none of the inner macular measures (GCC, GCIPL or GCL) have been demonstrated to be superior in detection of early glaucoma, it’s conceivable that these measures may not perform similarly for detection of glaucoma deterioration across the spectrum of glaucoma severity.”
“A major issue is that with advancing glaucoma damage, the task of segmentation of individual macular layers becomes more challenging; hence, measurements of thicker slabs of tissue such as GCC, the boundaries of which are easier to segment, may be less noisy,” they continued. “Another reason for potentially superior performance of GCC is that small amounts of positively correlated change within macular RNFL, GCL and IPL are added, and changes in the sum could be easier to detect than changes in the components.”
“Most prior studies reported high reproducibility for global and sectoral macular thickness measurements,” they wrote. “Research from our laboratory has demonstrated intra- and inter-session variability to be very low at the superpixel level for all macular outcome measures and mostly uniform across the macular region. This is another potential explanation for superior performance of the GCC in comparison with GCIPL and GCL, as the measurement error compared with the magnitude of change is smaller with GCC.”
The researchers reported that average follow-up time and baseline 10-2 visual field mean deviation were 3.6 years and -8.9dB. Furthermore, FMT (54.9%) had the highest proportion of significant negative slopes. This was followed by GCC (36.5%), ORL (35.6%), GCIPL (30.6%) and GCL (19.8%). They noted less worsening in the severe glaucoma group, detected by inner macular measures, but found that GCC (22.6%) identified the highest proportion (GCIPL 18.6%, GCL 10.8%). They said that the proportion of positive rates was small and comparable among all measures.
“Although for the majority of superpixels FMT had a significantly higher proportion of significantly decreasing slopes compared with other layers, in the clinically important paracentral superpixels, the proportions were not different between FMT and GCC,” they noted. “The signal-to-noise ratio was better for GCC thickness across the macular compared with GCIPL and GCL thickness. Although the signal-to-noise ratio for FMT appeared better than GCC in most superpixels, the FMT thickness measurements include ORL thickness values, which do not reflect damage from glaucoma.”
The researchers said their results confirm that “first, all inner macular measures demonstrate a reduction in the proportion of significant negative slopes detected over time in eyes with worse glaucoma damage (i.e., total deviation <-8dB) compared with those with less severe damage. Second, GCC measurements are best able to identify decreasing slopes compared with GCIPL and GCL, regardless of the level of glaucoma damage. The proportion of positive slopes only slightly increased with worsening glaucoma for all three inner macular measures.”
They wrote that the differences they found among inner retinal layers and detection rates of negative slopes were clinically relevant. “In the group with mild to moderate visual field damage, GCC detected 7% more worsening superpixels compared with GCIPL and about 18% more deteriorating superpixels than GCL,” they explained. “This would translate to about 2.5 to 6.5 more superpixels, on average, being detected as deteriorating by GCC slopes (compared with GCIPL and GCL slopes, respectively); given the large size of superpixels in this study (3°x3° or roughly 1mmx1mm), these would translate to large areas of the macula where additional evidence of change could be identified. The corresponding numbers for the severe glaucoma group were 1.5 and 4.5 more superpixels detected by GCC slopes compared with GCIPL and GCL slopes.”
They recommended that “macular GCC thickness measurements be made available on all OCT devices for optimizing detection of glaucoma progression,” especially in moderate to severe cases. They noted that their future work will examine how best to summarize regional and global rates of change, explore predicting functional change with longer follow-up times and work toward providing better data visualization for detecting progression in real-time.
Mohammadzadeh V, Su E, Rabiolo A, et al. Ganglion cell complex: the optimal measure for detection of structural progression in the macula. Am J Ophthalmol. December 20, 2021. [Epub ahead of print]. |

