 |
An 85-year-old Caucasian female presented with acute vision loss in both eyes. She stated that two days ago she developed pain on the left side of her head with vision loss in the left eye, which shortly spread to the right eye. She reported fatigue, weakness, jaw pain/claudication, scalp tenderness and pains around her head and the back of her neck for the past few months.
Her visual acuity was measured at hand motion in both eyes. Intraocular pressures were 10mm Hg in each eye. Anterior segment exam showed cataracts in both eyes; however, only three months prior she had best-corrected visual acuities of 20/30 OD and 20/40 OS. Posterior segment exam showed bilateral pallid disc edema.
Her retinal exam was otherwise unremarkable.
I (Dr. Trottini) called her internist—whom she had seen recently due to her general complaints of aches, pains and fatigue—and inquired about any recent erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) test results. There was no recent ESR, but a CRP from two weeks prior was 36.1mg/L (the normal range is <3mg/L); however, no additional testing or work up was performed based on this elevated lab study.
Diagnosis and Treatment
I consequently sent her to the emergency department and let the attending physician know that her likely diagnosis was bilateral arteritic ischemic optic neuropathy (AION) from giant cell arteritis (GCA). I recommended an ESR, CRP and temporal artery biopsy as well as rheumatology consultation. I also recommended neuroimaging to rule out any intracranial process, and results were normal.
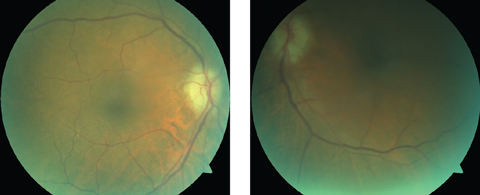 |
| Although our patient’s optic nerve photos were compromised due to her cataracts and imperfect fixation, they show pallid disc edema, which is characteristic of GCA/AION. Click image to enlarge. |
Her ESR was >140mm/hr and CRP was 33mg/L in the emergency department. These lab values, along with the normal neuroimaging, exam findings and other patient symptoms, were all consistent with GCA, and the patient was admitted and started on intravenous Solu-medrol (methylprednisolone sodium succinate, Pfizer) 1g daily for the next three days.
A temporal artery biopsy was performed the next day, which was positive and confirmed GCA. The patient finished the three-day course of Solu-medrol and was started on 80mg of prednisone, which will be tapered accordingly by rheumatology.
One week later on follow-up exam, although she reported almost immediate relief of her aches, pains and fatigue since starting the steroids, her disc edema looked slightly worse compared with the previous visit, and her vision had worsened to no light perception (NLP) in both eyes. She continued her current dose of prednisone and saw rheumatology for GCA management.
On repeat examination two weeks later, she had moderate improvement in her optic nerve appearance. The discs were well perfused again, and the pallid edema was essentially resolved. Unfortunately, she remained NLP in both eyes and has not regained any of her sight over time.
 |
| The large, palpable, firm temporal artery in another patient is a good representation of what the temporal artery can sometimes look like in GCA. Not surprisingly, this patient’s biopsy was positive. Click image to enlarge. |
Discussion
GCA is one of the few serious emergent disorders eye care providers encounter. It is a granulomatous inflammatory vasculopathy affecting medium and large size arteries. The commonly affected vessels include the external carotid branches, ophthalmic, vertebral, distal subclavian and the thoracic aorta.
GCA is a disorder affecting an older population (usually patients >50) and females have a higher incidence compared with males.1
The main concern from an OD’s standpoint with GCA is the development of arteritic ischemic optic neuropathy (AION). As the blood vessels supplying the optic nerve become inflamed, luminal occlusion occurs, which leads to ischemic complications.1 The goal is to recognize and treat GCA before AION occurs.
Typical presenting symptoms of GCA include headache, temple pain, neck pain, scalp tenderness, jaw claudication, weakness and tiredness/fatigue. The temporal artery may be firm and tender on palpation and often nonpulsatile.
With AION, vision loss is usually severe and responds poorly to treatment, as seen in our patient. Presenting vision loss is generally much worse when compared with vision loss from nonarteritic ischemic optic neuropahty (NAION). For example, one study showed initial visual acuity of count fingers to no light perception in 54% of AION patients compared with only 14% of NAION patients.2 Amaurosis fugax will be present in about one-third of patients and is a sign of impending AION.2 Additional ocular findings from GCA can include sixth nerve palsy, cotton wool spots and retinal artery occlusion. The disc edema from GCA/AION generally has a characteristic pale edema or chalky white color.2
This case highlights just how visually devastating GCA can be and the importance of recognizing the symptoms and clinical findings as early as possible.
If steroid therapy is started early in the course of GCA, vision loss typically does not occur. If one eye develops vision loss, the goal is to start treatment to prevent further vision loss in that eye and prevent it in the fellow eye.
When suspected, ESR and CRP should be ordered, as these tests will be elevated due to the presence of inflammation within the body. Further verification of GCA is obtained either by temporal artery biopsy or temporal artery ultrasonography, which has a similar sensitivity to biopsy.
GCA is typically treated with chronic oral steroids under the management of rheumatology; however, if AION does occur, a pulse-dose of 1g intravenous Solu-medrol is given for three days, then switched to oral steroids and generally continued for a lifetime.
Eye care providers should have a fairly low threshold of testing and evaluating for GCA, as ESR and CRP testing is inexpensive and easily obtainable. Temporal artery biopsy is also a routine procedure performed by vascular surgeons or even oculoplastic specialists, while temporal artery ultrasound is a good noninvasive alternative to biopsy.
Early diagnosis and treatment of GCA is imperative, given the severity of the disease and possibility of irreversible vision loss. As frontline eye care providers, ODs can help play a crucial role in identifying GCA as early as possible to mitigate negative outcomes.3
Clinicians should always maintain suspicion when presented with patient complaints of GCA and either initiate a work-up or promptly refer for a work-up.
Even after a patient has suffered vision loss due to GCA/AION, ODs can remain in contact with the rheumatologist, social workers, occupational therapists and other care providers to manage any vision loss affecting an individual’s quality of life.
1. Weyand CM, Goronzy JJ. Giant-cell arteritis and polymyalgia rheumatica. N Engl J Med. 2014;371:50-7. |

