Femto Fans Fight Back
We take some flak over recent coverage of FLACS.
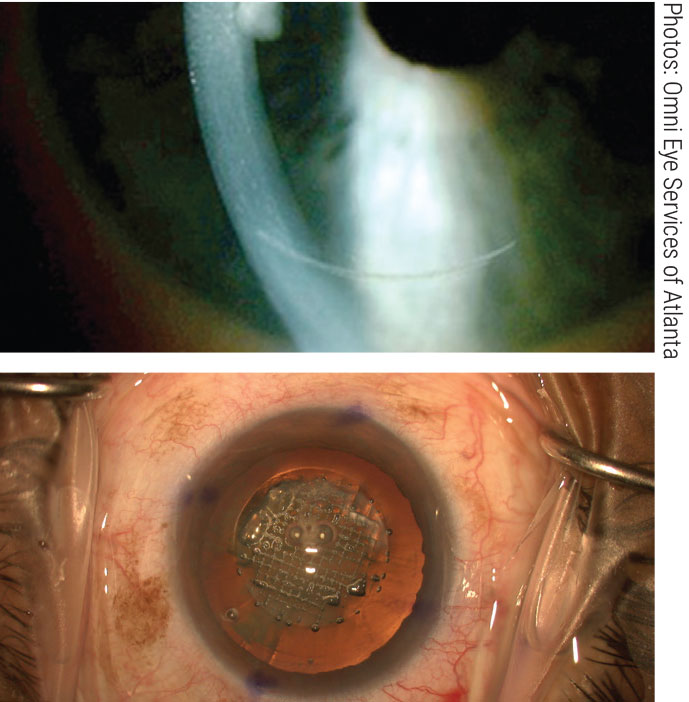 |
| The femtosecond laser makes precise arcuate incisions (top), fragments the nucleus (bottom) and automates capsulorhexis formation. Click image to enlarge. |
We read with interest your news story, “No Clinical Advantage to Femto Cataract Surgery” in the May edition. From our perspective, as a practice that had the first femto laser for cataract surgery (FLACS) in Atlanta in 2013, there are several problems with the journal article summary presented. We wish Review had not used such a “sensational” headline; it is oversimplification to state there is no clinical advantage to FLACS over standard phaco.
The article quoted is based on the results of one study in the British Journal of Ophthalmology, looking at one narrow aspect of FLACS. Most readers won’t take the time to read the manuscript, but if they did they would discover what we did, as one of many leading high-volume cataract practices that embrace FLACS and has clearly seen the advantages for the appropriate patient population:
1. In the study, intrastromal arcuate FLACS incisions were used instead of transepithelial ones, which are more effective and much more widely used. Limbal relaxing incisions (LRIs) are obviously transepithelial, so it demonstrates poor study design to use intrastromal FLACS incisions.
2. The study criteria required patients to have astigmatism >0.9D. Astigmatism correction by corneal incisions is quite unpredictable for that amount of astigmatism, whether by FLACS or LRIs. That is why it is generally accepted that toric intraocular lenses be used instead of corneal incisions for >0.8D of astigmatism. Inclusion criteria for the study should have been eyes under 0.9D, not over 0.9D. Despite this flaw, the study did show significantly less difference vector in the FLACS group vs. LRIs, indicating that laser arcuate incisions were more effective in reducing astigmatism. However, this was not mentioned in Review’s summary, a glaring omission.
3. The study did not report the percentage of eyes within 0.25D residual refractive error, only that within 0.5D and 1.00D. Numerous studies have documented benefit for FLACS vs. standard within 0.25D—some showing as much as 40% improvement among eyes within 0.25D. Most eyes will be within 0.5D with either procedure because modern IOL calculation formulas and new technology (optical biometers and swept-source OCT biometers) are quite accurate with IOL power selection. However, FLACS has been shown to increase the percent of eyes within 0.25D presumably due to the benefits of added precision of capsulotomy circularity and centration, which may decrease lens tilt and residual refractive error.
4. Post-op endothelial cell counts and central corneal thickness have been shown to be statistically significantly improved in FLACS cases. The BJO study’s finding that those were not better with FLACS should be further analyzed for possible explanations, because this goes against what almost all other studies have shown when evaluating those outcomes.
5. Phaco energy was also not reported in this study. It has been shown in many studies to be statistically significantly less in FLACS cases. Reduced ultrasound energy means less corneal endothelial cell damage and loss over time. Not reporting phaco energy used is a major flaw in this study design.
We would respectfully request that Review publish results from studies which evaluate the issues that we have raised here. Cited at the end of this letter are some studies that support our stance that there are many clinical benefits to FLACS.
A headline that states there is no clinical benefit based on a flawed British study leaves readers with misinformation which can quickly turn to misconceptions as they talk to patients each and every day. Unfortunately, we see in our referral-only practice that there is enough hesitation already by optometrists to get involved in pre-op counseling. Headlines like this will give optometrists the excuse they need to cut off discussions of new technology and premium services, thus depriving patients of factual information based on current studies so that they can make informed decisions about their upcoming surgery.
All studies we cite below, except one, are from The Journal of Cataract and Refractive Surgery, the premier US journal dedicated to such topics. Studies conducted in the US are much more rigorous than in other countries and are considered the gold standard. Each of these studies refutes individual pieces of the BJO “broad brush” study and shows a particular benefit of FLACS compared to conventional surgery. These studies reflect a small percentage of those available in the literature showing clinical benefits to FLACS.
We look forward to Review presenting the other side of the story so that readers are clearly aware this is a state-of-the-art technology that benefits patients and is very much here to stay.
—Lawrence Woodard, MD, and Paul C. Ajamian, OD
Omni Eye Services of Atlanta
1. Filkorn T, Kovacs I, Takacs A, et al. Comparison of IOL power calculation and refractive outcome after laser refractive cataract surgery with a femtosecond laser versus conventional phacoemulsification. J Refract Surg. 2012;28(8):540-4.
2. Chen X, Yu Y, Song X, Zhu Y, Wang W, Yao K. Clinical outcomes of femtosecond laser–assisted cataract surgery versus conventional phacoemulsification surgery for hard nuclear cataracts. J Cataract Refract Surg. 2017; 43:486–491.
3. Vasavada VA, Vasavada S, Vasavada AR, et al. Comparative evaluation of femtosecond laser–assisted cataract surgery and conventional phacoemulsification in eyes with a shallow anterior chamber. J Cataract Refract Surg. 2019; 45:547–552.
4. Ganesh S, Brar S, Arra RR. Comparison of astigmatism correction between anterior penetrating and intrastromal arcuate incisions in eyes undergoing femtosecond laser–assisted cataract surgery. J Cataract Refract Surg. 2020; 46:394–402.
5. Kolb CM, Shajari M, Mathys L, Herrmann E, Petermann K, et al. Comparison of femtosecond laser–assisted cataract surgery and conventional cataract surgery: a meta-analysis and systematic review, J Cataract Refract Surg. 2020; 46:1075–85.
6. Enz TJ, Faes L, Bachmann LM, Thiel MA, et al. Comparison of macular parameters after femtosecond laser–assisted and conventional cataract surgery in age-related macular degeneration. J Cataract Refract Surg. 2018; 44:23–27.
7. Mencucci R, De Vitto C, Cennamo M, Vignapiano R, Buzzi M, Favuzza E. Femtosecond laser–assisted cataract surgery in eyes with shallow anterior chamber depth: comparison with conventional phacoemulsification. J Cataract Refract Surg. 2020; 46:1604–10.
8. Fan W, Yan H, Zhang G. Femtosecond laser–assisted cataract surgery in Fuchs endothelial corneal dystrophy: Long-term outcomes. J Cataract Refract Surg. 2018; 44:864–70.
9. Lee JA, Song WK, Kim JY, et al. Femtosecond laser–assisted cataract surgery versus conventional phacoemulsification: Refractive and aberrometric outcomes with a diffractive multifocal intraocular lens. J Cataract Refract Surg. 2019; 45:21–27.
10. Cinar E, Yuce B, Aslan F, Erbakan G, Kucukerdonmez C. Intraocular lens tilt and decentration after Nd:YAG laser posterior capsulotomy: Femtosecond laser capsulorhexis versus manual capsulorhexis. J Cataract Refract Surg. 2019; 45:1637–44.
11. Roberts HW, Wagh VK, Sullivan, DL, Archer TJ, O’Brart DPS. Refractive outcomes after limbal relaxing incisions or femtosecond laser arcuate keratotomy to manage corneal astigmatism at the time of cataract surgery. J Cataract Refract Surg. 2018; 44:955-963.
12. Conrad-Hengerer I, Al-Sheikh M, Hengerer FH, Schultz T, Burkhard Dick HB. Comparison of visual recovery and refractive stability between femtosecond laser–assisted cataract surgery and standard phacoemulsification: six-month follow-up. J Cataract Refract Surg. 2015; 41:1356-64.
Femto ‘Facts’—or Fake News?
The June 2021 supplement Clinical Perspectives on Patient Care included numerous clinical questions and answers. Among the topics was a section titled “Facts on Femto.” The writers stated that “knowledge gleaned from the literature is so enlightening.” Their conclusion: “While there is a lot of hype and discussion regarding the ‘benefits’ (and increased revenue) from femtosecond-assisted cataract surgery, the consensus of the literature opines that such extra expense to the patient does not meet the clinical return on investment.”
I congratulate the writers on their exhaustive review of the literature on this topic, which included a total of four references. Moreover, two of these references were published in 2016, one in 2018 and one in January 2020. Each will be addressed below.
I am surprised the writers did not also find a more recent article, “Outcomes of Femtosecond Laser Arcuate Incisions in the Treatment of Low Corneal Astigmatism,”published in May 2020.1 Briefly, this peer-reviewed study shows that in fact use of the femtosecond laser in cataract surgery, including treatment of low amounts of corneal astigmatism, yields a 1.8x greater chance of uncorrected 20/20 distance vision over standard surgery.
1. The first reference noted by the writers, “Femtosecond Laser-Assisted Cataract Surgery Versus Phacoemulsification Cataract Surgery (FACT),” was a study of surgeries between May 2015 and September 2017 in the UK.2 In this article, we were treated to the knowledge that “based on a hypothetical cohort”(emphasis mine) an economic modeling evaluation showed FLACS was not cost-effective (using 2014 data). Also, the surgeons in this study had performed at least 10 supervised FLACS and been certified by laser manufacturers. The article later points out “correspondence suggests the learning curve may include the first 100 cases.” Surgeons could treat astigmatism with the laser or not based upon their discretion.
The patients’ subjective assessment part of the study included this choice of statements for agreement: “I have no problems seeing; I have some problems seeing; I have extreme problems seeing.”
Impressive scientific rigor and worthy of review this article was!
2. The second article referenced by the writers, “Efficacy and Safety of Femtosecond Laser-Assisted Cataract Surgery Compared with Manual Cataract Surgery” (MCS), was a literature search from 2007 to March 2016.3 Even back then, this review of articles showed a statistically significant lesser phaco time, greater capsular circularity, improved postoperative central corneal thickness and lessened corneal endothelial cell reduction with FLACS. “There was a significantly greater incidence of posterior capsular tears after FLACS relative to MCS,” the study notes. “Given that many of the included studies were published early after the introduction of FLACS, the surgeon learning curve may have influenced these results.”
In spite of these observations, and the fact that FLACS was approved by the FDA in 2010, those authors suggested “evidence of safety and efficacy of this technology is urgently needed.”
3. The third article referenced, “Femtosecond Laser-assisted Cataract Surgery versus Standard Phacoemulsification Cataract Surgery: Study from the European Registry of Quality Outcomes for Cataract and Refractive Surgery,” included femto cases performed between December 2013 and May 2015 by surgeons who had done at least 50 femto cases (see above on learning curve) and most of the complications occurred in the first few cases.4 Of the 2,814 FLACS cases that met the criteria for inclusion, only “127 cases had corneal astigmatism treated by the laser at the time of femtosecond-assisted surgery.” Also, a “higher rate of previous corneal refractive surgery in the femtosecond group is, clinically, very significant.”
Confirming that FLACS showed better reproducibility in capsular diameter and centration, better reproducibility of corneal wound construction and less ultrasound energy, the authors somehow reached the conclusion that “this study found no evidence to support claims that femtosecond laser-assisted cataract surgery is a major advance and better than the conventional method.”
4. The final article, “Visual and Refractive Outcomes in Manual versus Femtosecond Laser-Assisted Cataract Surgery,” reviewed eyes receiving FLACS and MCS from July 2012 to July 2015.5 Again, in this study astigmatism was only corrected with a toric IOL. To reduce outliers, anyone with greater than 1.5D of corneal astigmatism who elected to have a non-toric IOL was excluded. This does not address those with up to 1.5D.
The study concludes that “no statistically significant difference was found between eyes undergoing FLACS and eyes undergoing MCS with respect to refractive and visual outcomes” but allows that “surgeon learning curves and ongoing FLACS technological improvements may have altered its risk profile in the present day.”
With 35 years working in an optometric referral center specializing in cataract and laser surgery, I would like to share the way I see it.
When first introduced, FLACS was supposed to make a poor surgeon good and a good surgeon great. It hasn’t turned out that way. Due to the cost of equipment and steep learning curve, those who do not want to make the financial and time commitment just find fault with FLACS. But the surgeons who do commit to the technology demonstrate its superiority.
As an example, one of our surgeons—one author of the study mentioned above—is on record as saying there was no advantage to FLACS. His experience prior to joining our practice led him to this conclusion. However, after joining our group and committing to the technology, he sees it much differently. To prove the point, he (and others) did the research and proved better outcomes with FLACS.
Both surgeons in our practice will readily admit the femtosecond laser makes a more consistently round and properly positioned capsulorhexis than they can do by hand. These are two outstanding cataract surgeons with excellent hands. They would further say that when their turn comes, they want FLACS for their eyes.
I challenge any OD or MD to observe FLACS and MCS performed by suitably experienced surgeons and not conclude FLACS is better. Some faults in studies used to belittle FLACS include the age of the studies (including the infancy of FLACS at that time), the relative inexperience of the surgeons using the FLACS method at the time of the study, the omission of correction for lower amounts of astigmatism—what OD would Rx a pair of glasses that didn’t correct low astigmatism?—and perhaps some personal bias.
The innuendo that FLACS is only encouraged to generate higher surgical fees is insulting. What doctor would not offer the newest technology in contact lenses and spectacles because they cost more? Should patients be denied the option for better technology because it costs more? Of course not.
Want a historical analogy? Around 1990, when sutureless cataract surgery came on the scene, there were plenty of haters. I was included in that group. Nowadays, who does not agree that sutureless is superior (given a well-constructed wound) and is surprised to see any of their post-op patients with sutures?
“Facts on femto?” Hardly. Let’s keep fake news out of our journals.
—Howell M. Findley, OD
Lexington, KY
1. Wortz G, Gupta PK, Goernert P, Hartley C, Worthz B, Chiu J, Jaber N. Outcomes of femtosecond laser arcuate incisions in the treatment of low corneal astigmatism. Clinical Ophthalmology. 2020; 14: 2229-36.
2. Day AC, Burr JM, Bennett K, et al; FACT group. Femtosecond laser-assisted cataract surgery versus phacoemulsification cataract surgery (FACT): A randomized noninferiority Trial. Ophthalmology. 2020; 127(8):1012-9.
3. Popovic M, Campos-Möller X, Schlenker MB, et al. Efficacy and safety of femtosecond laser-assisted cataract surgery compared with manual cataract surgery: a meta-analysis of 14,567 eyes. Ophthalmology. 2016; 23(10):2113-26.
4. Manning S, Barry P, Henry Y, et al. Femtosecond laser-assisted cataract surgery versus standard phacoemulsification cataract surgery. J Cataract Refract Surg. 2016; 42(12):1779-90.
5. Berk TA, Schlenker MB, Campos-Möller X, et al. Visual and refractive outcomes in manual versus femtosecond laser-assisted cataract surgery: a single-center retrospective cohort analysis of 1838 eyes. Ophthalmology. 2018; 125(8):1172-80.
From the Editor: The above letters raise many valid points—and a few spurious ones. None of the 12 studies cited in the first letter were conducted in the US, undermining that letter’s critique of the BJO study for having been conducted outside the US. The second letter takes the authors of the Clinical Perspectives supplement to task for citing only four studies but overlooks the decades of hands-on expertise that also informed their views—an ethos built into the very title of that publication. When summarizing a journal article for a news story, we take care to note that we are describing the results of a single study. Implicit in this framing is a reliance on readers’ knowledge that rarely is any one study the definitive word on a topic. The current issue of this publication includes a news story on positive attributes of FLACS in diabetic patients; we similarly do not expect readers to take that brief summary as the final word on the matter either. Clinicians stitch these and other glimpses of knowledge together into a mosaic. Still, we acknowledge that the headlines used may not always reflect such nuance; we’ll aim to do better. Femto cataract surgery achieves impressive results, but its considerable expense and logistical challenges put greater burdens on surgery centers and patients alike. It’s fair to ask for an accounting of value in return. The studies and insights shared in these letters help advance that discussion, and we’re grateful for the opportunity to enable a deeper understanding of complex clinical issues. |
Back to the Future
I feel we have reached a critical juncture in our profession’s history. I view a number of issues with a mixture of anxiety, concern and disappointment. I believe this to be more than the usual problems we face—it’s worrisome because it involves a confluence of multiple strategic threats.
Over 50 years ago, optometry faced a similar crossroads: either the profession needed to move forward by adopting a medical model or face extinction. A group of visionaries met in a hotel room at LaGuardia airport and changed the course of the profession. At the meeting, they decided to advocate for optometrists to play a role in diagnosis and treatment of eye diseases. Three years later, the first DPA bill was passed in Rhode Island and the profession as we now know it was born.
 |
| In 1968, Alden Haffner, Irv Borish, Norman Wallis and other luminaries met at LaGuardia airport and decided to push for a new era in optometric care. Is it time for another? Click image to enlarge. |
Where we would we be today without the foresight of those individuals?
I think we are at a similar crossroads now. The inevitable changes that are going to occur in our current health delivery system will not spare optometry. The current model is unsustainable. But I believe it’s always preferable to be prepared and proactive as opposed to waiting and being forced to react.
Currently, these are the main challenges as I see them:
1. Quality/quantity. At the Academy 2019 meeting in Orlando, I had the opportunity to talk with a number of young ODs involved with residency programs throughout the country. They have serious concerns about the quality of the recent crop of graduates from optometry schools. Apparently, the explosion in new optometry schools has resulted in a decrease in selectivity when accepting students. The ratio of applicants to acceptees is approaching 1:1. When I applied to PCO, there were 14 optometry schools and now there are 23. When I graduated, there were about 27,000 optometrists in the US. Today there are over 41,000.
2. Residencies. This has always been an issue for me. I still maintain that the only difference between OD and MD training is a residency. I appreciate the argument concerning the difficulties facing mandatory residency. I maintain that a solution can be found once a decision is made to move ahead.
3. Reciprocity. This is an embarrassment. It is also anti-competitive. Someday somebody is going to go ahead and also make this an anti-trust issue. Once everything else is addressed, there will be no excuses for this to continue and those states that do will be leaving themselves open to litigation.
4. Multiple certifying boards. Another embarrassment. I see this ultimately as a leadership issue. The leaders of the profession (not necessarily elected) need to come together to resolve this.
5. Artificial intelligence. I see two separate issues here:
First, online autorefraction is an existential issue. This isn’t something that’s just coming—it’s already here. The bottom line is that if your business model is only based on refraction, you’re in trouble.
Second, we risk exclusion from diabetic and glaucoma screenings. Diabetic telemedicine is already here. Last time I saw my PCP, there was a big sign in the office offering tele-eye exams for diabetes patients. My concern is not the technology—it’s already up and running. My concern is OD access to be providers of this service. It is likely that these types of screening programs (soon to include glaucoma) will only allow MDs and exclude ODs.
6. Vision exams. This is a fundamental issue for the profession that goes back to the time of Prentice. At some point, we are going to have to decide whether we are refractionists or health care providers.
7. As-taught legislation. Eventually, this principle of licensure will need to be addressed or optometry will eventually find itself irrelevant. Going back to the legislature for every new medication or technique is impractical and hinders the advancement of care that scope expansion laws aim to achieve in the first place.
I’m old enough to have personally known several attendees of the LaGuardia meeting. To the best of my knowledge, all were Academy members and many were from academia. I believe that this is where leadership needs to come from again.
We need people to stand up. We need another LaGuardia.
—John J. O’Donnell, Jr., OD, FAAO, Dipl. (Glaucoma)
Harrisburg, PA
Fanelli and Sowka: Greek Gods
I read with interest two articles in the June issue, “Don’t Feed the Hand that Bites You” by James Fanelli, OD, and “Not a Brite Idea” by Joseph Sowka, OD, both about surgical misadventures in procedures of dubious medical necessity. I was heartened by the pronouncement of each author and commend their fortitude in reaffirming our duty to abide by the Hippocratic Oath: First, do no harm.
“If there is one act alien to civilized behavior yet applauded by society, it is surgery,” opined Richard Selzer, MD, a brilliant surgeon and author, in a 2004 US News & World Report article.
In other words, surgery is a necessary evil conferring a big burden on all concerned. Medical necessity should be the omnipresent preoccupation on the mind of caring professionals, as exemplified by the likes of Drs. Fanelli and Sowka.
Kudos to both. I’ll frame their inspiring and caring conclusions and will keep honoring my own oath to “do no harm.”
—Joseph Hallak, PhD, OD, FAAO
Syosset, NY
To comment on these discussions, or start your own, write to editor@reviewofoptometry.com.

