 |
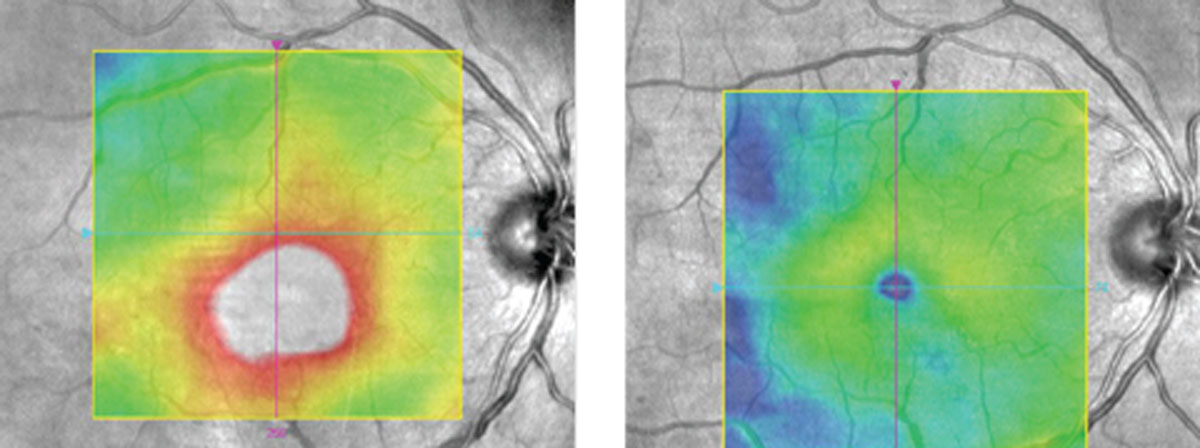
| Retinal fluid volume may help guide DME management. Photo: Diana Shechtman, OD, and Jay M. Haynie, OD. Click image to enlarge. |
Retinal thickness, the sum of retinal tissue, cystic spaces and subretinal fluid, is a key biomarker in the management of diabetic macular edema (DME). Currently, the correlation between visual acuity (VA) and central subfield thickness (CST) is weak. Having a biomarker that correlates more closely with VA may help clinicians make more meaningful treatment decisions. Researchers at the Casey Eye Institute in Portland, OR, believe retinal fluid volume may be a more specific indicator of exudative changes in DME.
The study enrolled 125 patients with DME between the ages of 18 and 85 (60 women, mean age: 61). A deep learning-based algorithm was able to provide accurate segmentation and quantification of 3D fluid volume in the retina from dense OCT-A 3mmx3mm scans. The detected fluid was subdivided into inner fluid volume, bounded by the inner nuclear layer (INL), and outer fluid volume, the fluid between the outer border of the INL to the ellipsoid zone.
The mean detected inner fluid volume was 0.013mm3 in 109 eyes (87%). The mean detected outer fluid volume was 0.042mm3 in 124 eyes (99%). Univariate analysis demonstrated that the VA significantly correlated with the inner fluid volume, whole macular fluid volume and CST; however, multivariate analysis demonstrated that the inner fluid was the only significant factor. These correlations were consistent when the study analyzed the treatment-naïve group (n=33) and the eyes without previous laser treatments (n=93) separately. The area under the receiver operating characteristic curve (AUC) of inner fluid for a VA of 20/32 or worse was significantly higher than the AUC of CST (0.66 vs. 0.54, respectively).
The INL comprises numerous packed cells, including bipolar, amacrine and horizontal cells. The researchers suggested the presence of fluid in the INL may disrupt pathways that transmit visual information from the photoreceptors to the ganglion cells. Intracellular swelling may lead to increased tissue volume, causing more swelling damage to the INL and negatively impacting VA.
“Our group has demonstrated that an automated central macular fluid volume may be more sensitive and specific in detecting DME than CST, especially in eyes with retinal atrophy,” the researchers wrote in their paper. Nevertheless, they also noted that a longitudinal study is needed to validate the clinical utility of inner fluid volume.
Tsuboi K, You QS, Guo Y, et al. Association between fluid volume in inner nuclear layer and visual acuity in diabetic macular edema. Am J Ophthalmol. December 20, 2021. [Epub ahead of print]. |

