 |
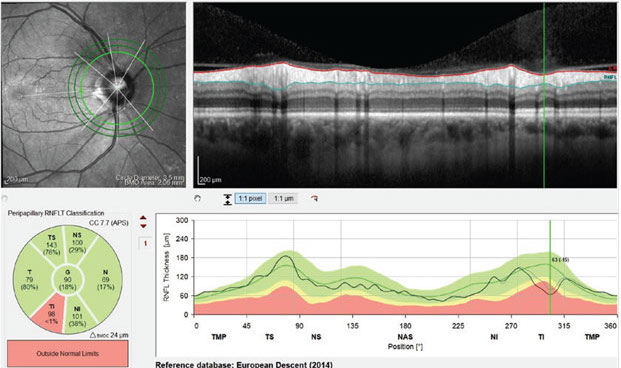
| Clinicians are increasingly aware of the potential for so-called “red disease” artifacts in high myopes. Photo: Jim Fanelli, OD. Click image to enlarge. |
OCT is a useful tool for diagnosing and monitoring glaucoma and optic atrophy, but in patients with refractive errors, the imaging modality can turn up false positives and false negatives due to optics of the eye. Researchers of a recent study noted that for these situations, the terms “red disease” and “green disease” were coined to describe, respectively, the deceptive thinning of the pRNFL in highly myopic eyes (colored red), yielding a false positive, and a seemingly normal pRNFL (colored green) in highly hyperopic eyes, yielding a false negative.
“In most OCT devices, such optical effects are not taken into account,” said the researchers, who examined average pRNFL measurements in healthy eyes to develop a simple method of evaluating average pRNFL in eyes with refractive errors. “The only exceptions are Topcon instruments, which measure pRNFL along a circle whose diameter is adjusted for AL and other parameters of the optical system of the eye. Modern OCT devices by Nidek have a ‘Long AL Normative Database’ for eyes with an AL of 26mm to 29mm. However, this database is not intended for pRNFL adjustment.”
The researchers evaluated the average pRNFL of 183 eyes of 183 healthy white subjects (mean age: 40+; AL: 22.5mm to 24.5 mm, SE: -1.63D to 2.00D) on the Cirrus HD-OCT. From this, they created a database of average pRNFL in mostly emmetropic eyes. The first and fifth percentiles of the distribution of average pRNFL thicknesses for the four age groups were as follows:
41 to 50 years: 81µm and 83µm
51 to 60 years: 79µm and 81µm
61 to 70 years: 78µm and 80µm
71 to 85 years: 76µm and 79µm
The researchers also created a table of first and fifth percentiles for eyes with ALs of 19mm to 30mm in the same age groups using a modified Littmann-Bennett formula (Table 1).
“Various formulas have been proposed to correct the effect of refractive errors on pRNFL,” the researchers explained. “These formulas are used in research but not in practical work due to the need to make calculations, albeit simple ones. Most importantly, the results obtained cannot be compared with the normative databases of OCT devices, since such a comparison is not provided by the manufacturers.”
“The results of the study make it possible to evaluate the average pRNFL data in eyes with refractive errors quickly and easily, without any calculations,” they said. “This is especially valuable in patients with refractive errors of high degree. Table 3 [in the study] is for the Cirrus HD-OCT device only; however, the proposed new formula makes it easy to calculate a similar table for any OCT device using existing databases or after collecting a normal database of eyes with refraction close to emmetropia.”
“In the older age groups, many individuals are pseudophakic, and their refractive errors are corrected by intraocular lens implantation,” they continued. “However, as [another study showed] even a large change in refraction in myopic eyes (mean 8.35D) practically did not change the average pRNFL thickness (mean change 0.2µm). It means that Table 3 [in the study] is also suitable for pseudophakic subjects (and AL—not the refraction—should be considered).”
Importantly, the researchers noted that their proposed table is intended only to estimate average pRNFL, not pRNFL in quadrants or clock hours. “This is due to the different distribution of pRNFL in highly myopic eyes—a shift of the upper and lower pRNFL humps to the temporal side, which doesn’t allow for the use of percentile values that could be calculated for quadrants and clock hours.”
They also used applanation ultrasound biometry measurements of AL since the original formulas they modified were created in the era of ultrasound biometry. “Optical biometry AL measurement should be reduced by 0.14mm or the equivalent used in the specific clinic,” they noted.
They concluded that their proposed table should provide a quick way of assessing the pRNFL results of patients with large refractive errors on the Cirrus HD-OCT.
Table 1. Average pRNFL Thickness by Percentile, Age and AL
AL (mm) | 41-50 years (µm) | 51-60 years (µm) | 61-70 years (µm) | 71-85 years (µm) |
19.0 | 102 (1st), 104 (5th) | 99, 102 | 98, 100 | 97, 99 |
22.5 | 85, 87 | 82, 84 | 81, 83 | 80, 82 |
27.5 | 68, 70 | 66, 68 | 65, 67 | 64, 66 |
30.0 | 62, 63 | 60, 62 | 60, 61 | 59, 60 |
Shpak AA, Korobkova MV. Evaluation of average retinal nerve fiber layer measurements in eyes with refractive errors. Optom Vis Sci. October 20, 2021. [Epub ahead of print]. |

