 |
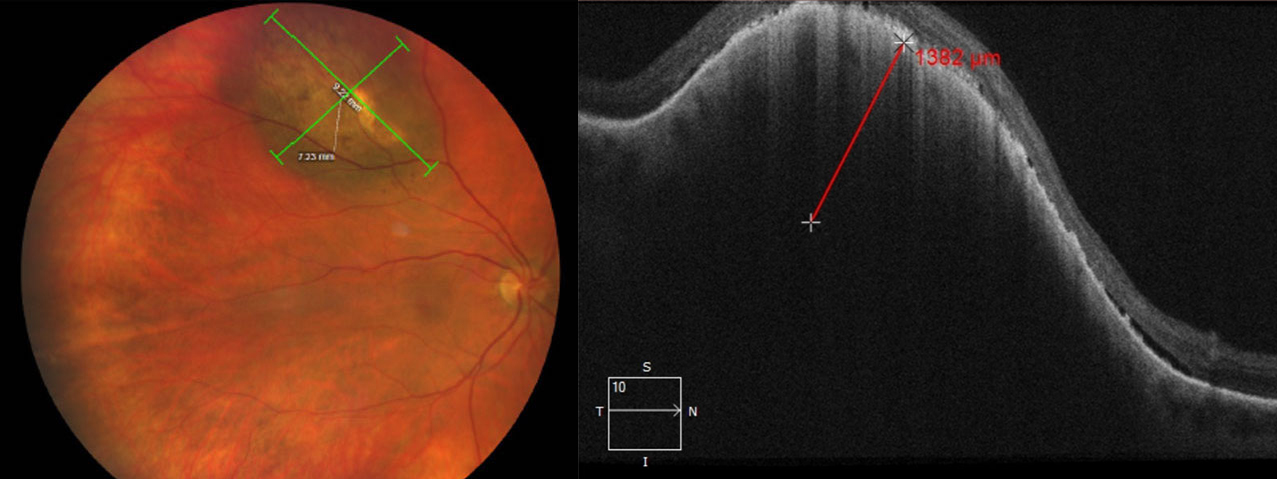
| fSRT may effectively treat small, medium and large tumors, this study concluded. Photo: Amy Bade, OD. Click image to enlarge. |
Uveal melanoma are rare ocular tumors associated with significant morbidity and mortality. Fortunately for patients, there are several effective treatment options, one of which is fractionated stereotactic radiotherapy (fSRT). fSRT is used mainly for small- and medium-sized uveal melanoma. It may also be used in larger tumors up to 12mm in thickness and 16mm in diameter. A benefit of fSRT is that it does not require any surgical procedures to determine tumor localization and dimension. Reported radiogenic side effects include cataract, retinopathy, maculopathy, neovascular glaucoma, vitreous hemorrhage and optic neuropathy. Visual impairment and secondary enucleation rates (3% to 16%) are similar to those associated with other treatments like proton beam radiotherapy and brachytherapy.
Researchers recently evaluated the value of fSRT for uveal melanoma in a study published in Acta Ophthalmologica. “Since there are overlapping treatment options depending on the tumor size and location, it’s important to know the potential radiogenic side effects and how to treat them,” the researchers explained. “Awareness of the risk of side effects can influence the choice of treatment. Since some side effects develop over the years, we only analyzed our treated patients with a follow-up of at least five years.” The researchers reported on local tumor control rate, late radiogenic side effects, visual preservation and disease-free survival.
A total of 189 patients were treated with fSRT for uveal melanoma by the Rotterdam Ocular Melanoma Study group between 1999 and 2014. The research group reported the following findings:
- Local tumor control rates at one, three, five, 10 and 15 years were 99.4%, 92.8%, 92.2%, 89.3% and 89.3%, respectively.
The most common side effect was cataract (67%), followed by retinopathy (35.1%), maculopathy (23.8%), vitreous hemorrhage (20.1%), neovascular glaucoma (20%) and optic neuropathy (12.4%).
Anterior-located uveal melanoma developed cataracts more frequently.
Tumor recurrence and neovascular glaucoma were significant factors for secondary enucleation.
At five years, 77% of patients experienced disease-free survival. Risk factors for worse disease-free survival included larger uveal melanoma and tumors with subretinal fluid at baseline.
The researchers reported an overall decrease in visual acuity in the patient cohort. A total of 22% of patients after five years and 17.6% of patients after 10 years had a visual acuity less than or equal to 0.3logMAR. Visual acuity worsening was mainly due to cataract, maculopathy, retinopathy, optic neuropathy, vitreous hemorrhages or neovascular glaucoma. “Visual acuity is most effectively preserved in eyes with small tumors outside a radius of 5mm from the optic disc and fovea,” the researchers explained.
“Local tumor control was excellent,” they noted. Their findings fell in between a few other studies, which they say may be due to differing definitions in tumor recurrence. In the present study, tumor recurrence was classified as tumor growth after initial regression post-treatment.
“Overall, the three-year tumor control rate was 92.8% and therefore comparable with other SRT studies with a tumor control rate of 94% at approximately three years after SRT and 93.3% after gamma knife radiosurgery with a median time of 29.4 months,” they said.
“In our cohort, patients with large tumors and uveal melanoma with subretinal fluid at baseline had a worse disease-free survival,” the researchers noted. “The risk for metastasis and death increased twofold with each increasing tumor category, and the 10-year metastatic rate was 15% for T1, 25% for T2, 49% for T3 and 63% for T4 tumors.”
They concluded that fSRT is a good treatment option for patients with small, medium and large tumors.
van Beek JGM, van Rij CM, Baart SJ, et al. Fractionated stereotactic radiotherapy for uveal melanoma: Long-term outcome and control rates. Acta Ophthalmologica. September 16, 2021. [Epub ahead of print]. |

