Cataract surgery is one of the most common procedures across the globe and the number one surgery (of any stripe) performed in the United States. But with an expanding pool of potential postoperative outcomes, patients have a higher demand than ever for precision. Today’s intraocular lens (IOL) technology, while imperfect, benefits from an array of recent innovations. While none replicate the eye’s natural ability to accommodate and refocus at varying distances as in a pre-presbyopic eye, the newest slate of IOLs can give patients more independence from glasses than ever before.
The optometrist’s role in preparing patients for cataract surgery includes a robust understanding of these available IOL options and how to best match a patient to the technology that fits their priorities. As good as the newest lenses may be, they still impose trade-offs among near, intermediate and distance vision. All patients are likely to experience improved vision after the procedure, and many can achieve excellent postoperative acuity at multiple focal lengths—if we do our jobs well in patient selection and pre-op education. This article will give an overview of the process.
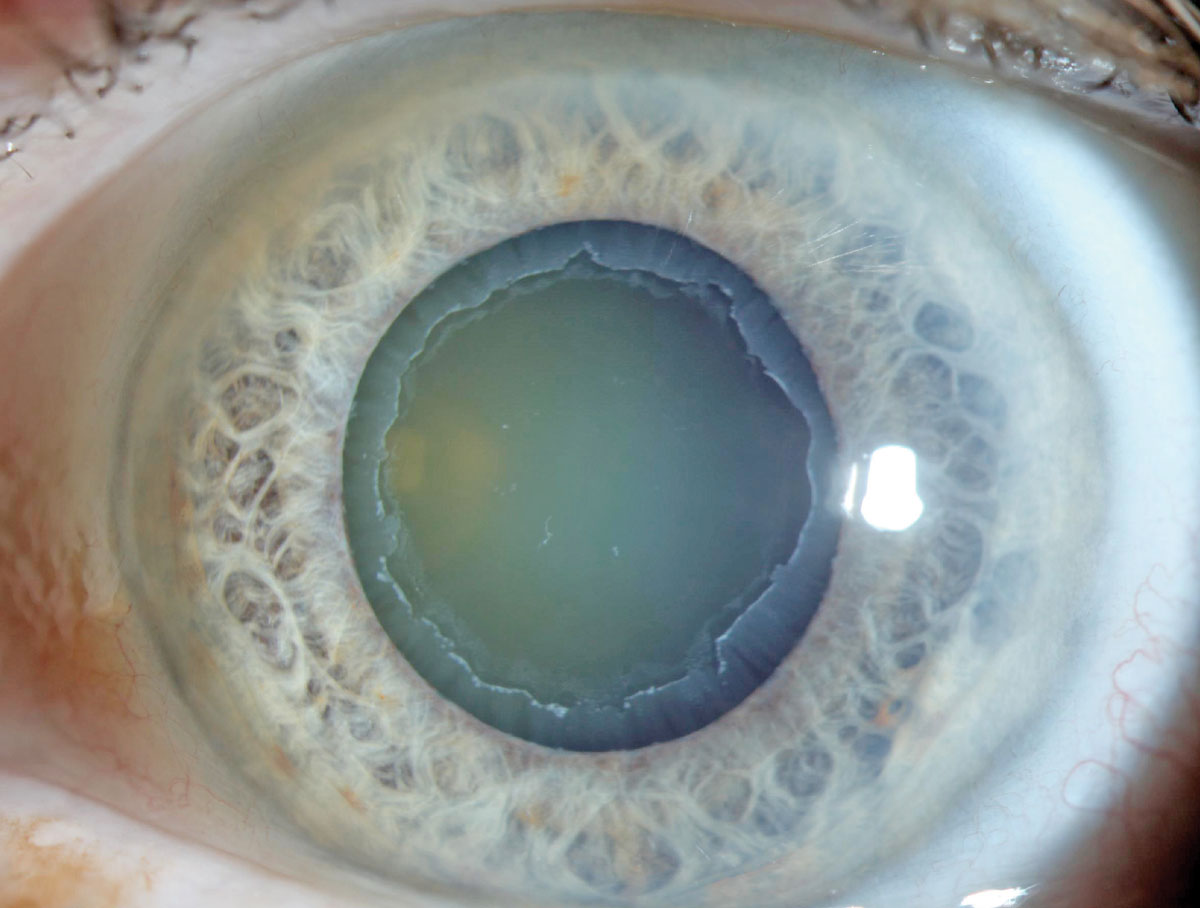 |
| Pseudoexfoliation can cause difficulty in IOL placement. Due to association with weak zonules, specialty lenses are contraindicated in these patients. Photo: Aaron Bronner, OD. Click image to enlarge. |
First Things First
Initial consultation for cataract surgery should include best-corrected acuity, glare testing and a history that details the patient’s lifestyle. To get an understanding of their expectations, start by discussing how reduced acuity affects their day-to-day functioning. No “absolute” acuity will qualify a patient for insurance reimbursement, but a good rule of thumb is to begin discussing the future need for cataract surgery when the patient is beginning to struggle with those daily activities with no improvement despite glasses or contact lenses.
Recent research shows that when patients recognize postoperative visual improvements, they are more satisfied with the surgery—especially when they regain unaided near vision for reading after the cataract is removed.1 Younger patients, who still have some remaining accommodative ability left before the surgery, tend to rank their satisfaction lower postoperatively compared with those in their 70s or older.1,2
If the patient does not present with any glare issues from the cataract, the potential for “trading symptoms” is also a concern.2 As initial dysphotopsia following surgery is not uncommon, patients also must be educated preoperatively about the potential for glare, arcs, streaks and halos initially after surgery.
In addition, proper reassurance during the healing period that neuroadaptation improves with time will help minimize patient stress during the recovery process.
Toric IOLs
Of the two broad categories of premium IOLs—toric and presbyopic—the former is more likely to succeed. However, while 52% of patients can be treated with a toric IOL, only 7% of patients receive one.3 Of course, the first step is figuring out which patients are in that 52% who qualify.3
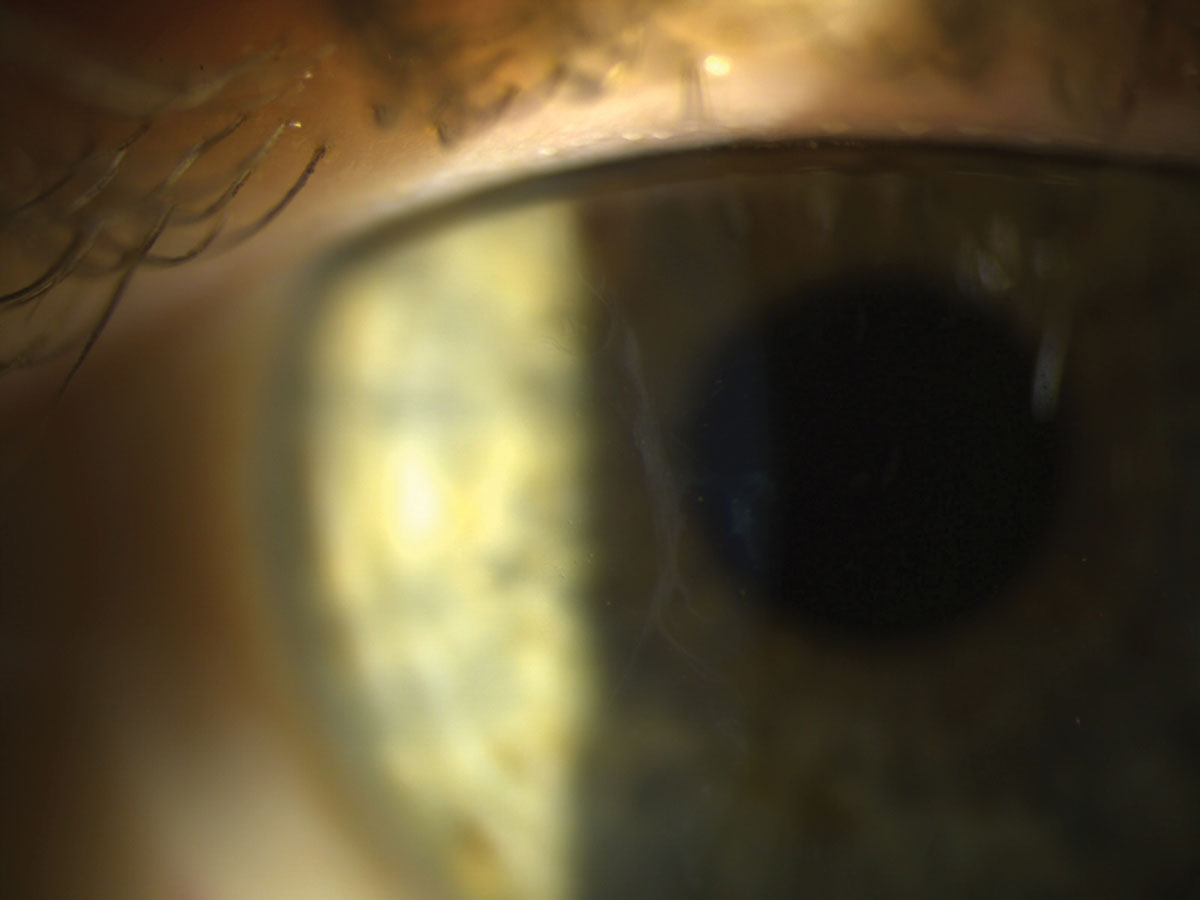 |
| Even subtle EBMD may disrupt aberrometry measurements and ultimately patient’s visual outcome with a toric or premium IOL. Click image to enlarge. |
Whether incompatibility is due to personality quirks that make adaptation difficult or preexisting ocular conditions that limit best-corrected visual acuity (BCVA), setting reasonable vision goals is the first step.4-6
Recent research shows ‘Type A’ patients are more likely to fare poorly with a premium lens.4 A patient who has a long history of maladaptation to progressive lenses and updated prescriptions yearly may not be able to appreciate the gain of less dependence on glasses. Instead, these patients will more likely nitpick at the small aberrations and dysphotopsias associated with these lenses. Conversely, those with more agreeable or open personalities (Type B) tend to adapt better to the new lenses, whether standard or premium.4
Obvious ocular morbidities (e.g., macular degeneration, ocular surface disease, diabetic retinopathy, glaucoma) are contraindicated and easily explained to patients.5 More subtle findings tend to require more explanation as to why a premium lens would not be a proper match. These can include forme fruste keratoconus, mild epiretinal membrane and epithelial basement membrane dystrophy (EBMD), for which the patient has no symptoms.
One study earlier this year found that EBMD can result in inaccurate biometric keratometry measurements used for IOL selection, leading to post-op refractive inaccuracies and patient dissatisfaction.4,7 Instead, the patient should be educated on the diagnosis and potentially offered phototherapeutic keratectomy to smooth out the corneal surface. However, if corneal opacity persists, many of these patients will be poor premium lens candidates.
Before cataract surgery, be sure to evaluate all patients with corneal topography. Instead of educating your patient on toric IOL candidacy based on refractive cylinder, using corneal topography offers more accurate information when calculating IOLs. You can compare your corneal topography findings to your autorefractor Ks to see if the patient would likely be a candidate for an astigmatism-correcting lens at the time of surgery. If the two measurements are not within half a diopter, the typical IOL increment, careful evaluation of the cornea may be warranted. As mentioned above, subtle changes like EBMD or dry eye can distort keratometric readings and, ultimately, post-op results.7 Management of such treatable corneal findings should be addressed before proceeding with cataract surgery measurements.
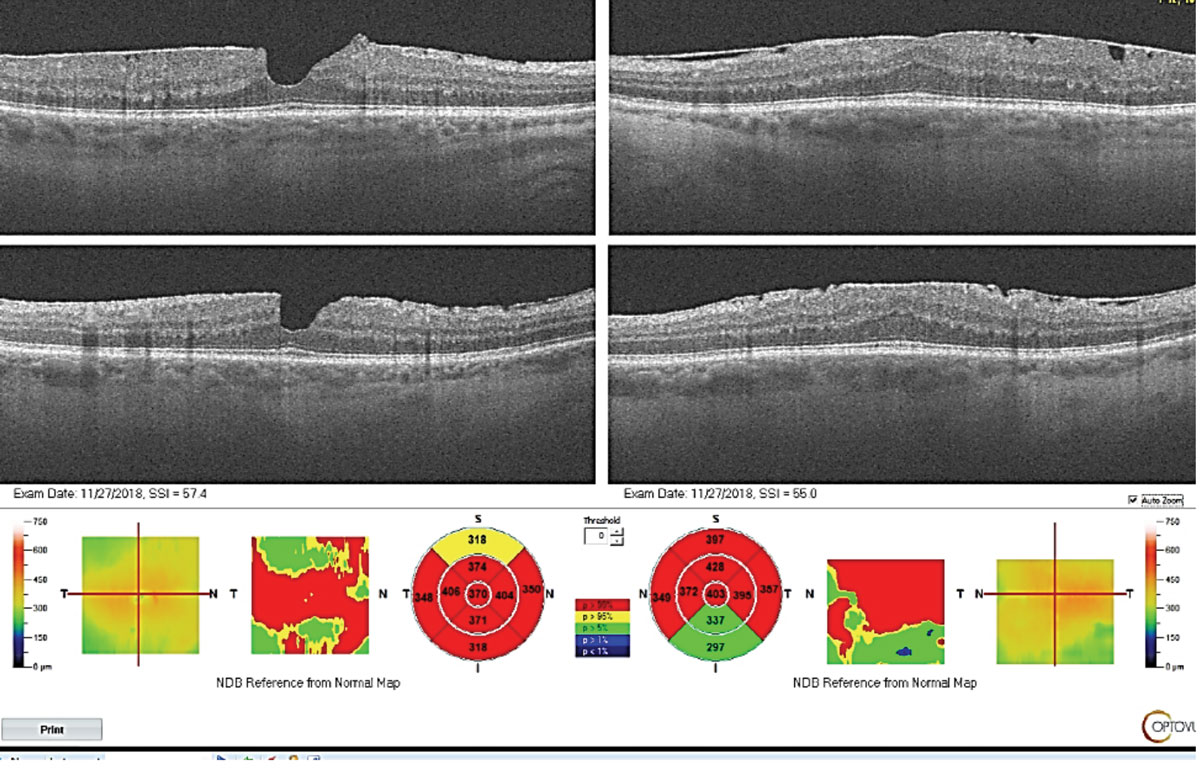 |
| Epiretinal membrane is a contraindication for proceeding with premium IOLs as the patient’s acuity post-operatively is likely limited. In addition, patients are at elevated risk for post-operative cystoid macular edema. Click image to enlarge. |
Furthermore, it is prudent to notify patients if they are at higher risk for zonular dehiscence at the time of surgery due to history of trauma, history of retinal detachment repair with silicone oil or presence of pseudoexfoliation. With weakened zonular integrity, orienting the axis accurately or centering the lens in a poorly secured bag will be difficult. Luckily, a capsular tension ring is typically placed into the capsular bag to help stabilize the structures enough to accommodate a toric IOL.8
After evaluating for these contraindications and establishing need for astigmatism correction, it’s time to guide the toric-candidate through their options. Depending on the patient’s preferred endpoint or chosen residual prescription, the benefits of electing a toric IOL may vary. If sharp distance vision without correction is their priority, then proceeding with a toric IOL is important in achieving their lifestyle goals. But careful discussion is needed to emphasize loss of intermediate and near function in the single-focus lens. In addition, individuals with career environments that may enhance sensitivity to glare, arcs, and other aberrations may benefit to neutralize their astigmatism to minimize ghosting and streaks with focal lights.6
What may also be a crucial factor in a patient’s decision making is the financial burden of opting for a non–insurance-covered lens. Careful consideration of the cost/benefit tradeoffs of toric IOLs in patients hoping to retain near function will depend on the patient’s blur tolerance. Astigmatism below 1.50D may not negatively affect their near acuity and a spectacle Rx at distance will be required to achieve the best results anyway. If proceeding with a specialty lens comes at too high of a financial burden for the patient, the preoperative evaluation serves as an opportunity to create an alternative plan to achieve their goals once they are stable from cataract surgery.6 After evaluating for these contraindications, it’s time to guide the toric candidate through their options.
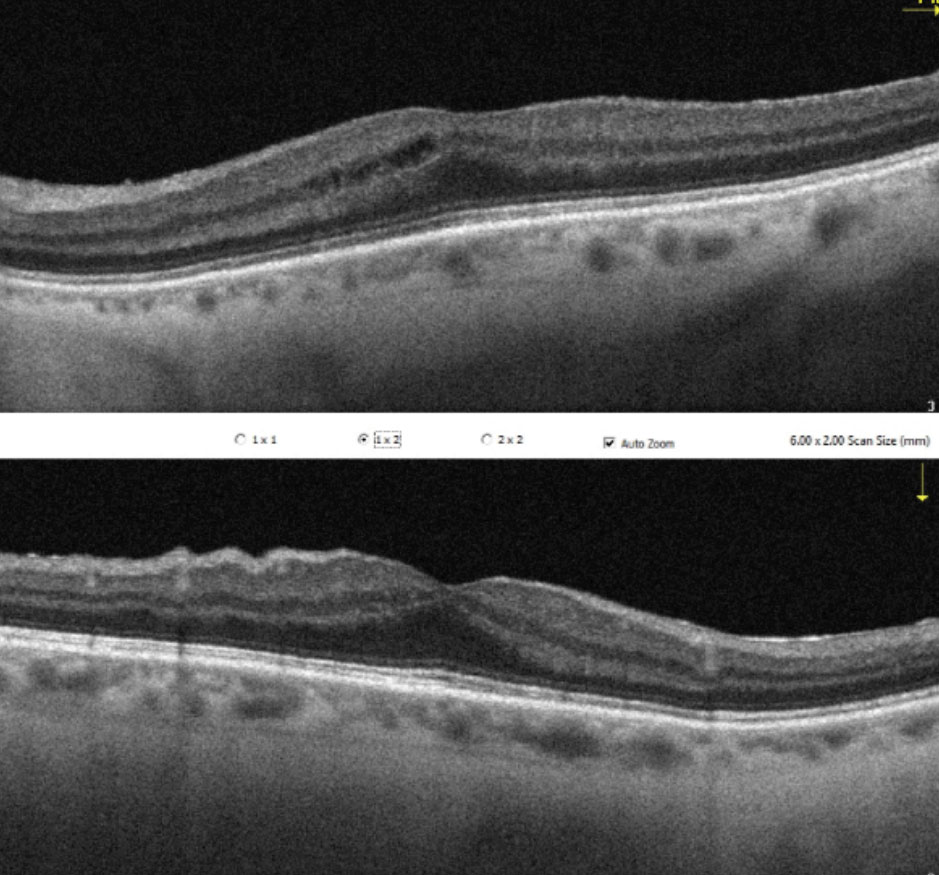 |
| Irvine-Gass syndrome 1.5 months following cataract surgery. Prompt treatment with an NSAID and steroid typically results in a good prognosis and full resolution in a few weeks. Click image to enlarge. |
Femtosecond laser limbal relaxing incisions (LRI) may be recommended to better manage small (<1.25D) amounts of corneal astigmatism. Though more accurate than its manual predecessor, performing the LRI with a laser at an incorrect axis can still occur and cannot be undone, resulting in increased or irregular astigmatism. Additional risks of LRIs include regression and wound leak, which makes toric IOLs the safer alternative even given the risk 10 degrees or more of rotation in a small number of cases (less than 3%).9,10
An enhancement procedure like LASIK or PRK post-cataract extraction can also accurately treat residual refractive error when needed.11 In cases where the patient presents with more than 5D of corneal toricity and no other irregular corneal findings, a toric IOL to eliminate the majority of the prescription is done first, followed by a laser enhancement to fine-tune vision with much less tissue removal. Similar considerations need to be made when treating more than 2.5D of astigmatism matched with toric multifocal or extended-depth-of-focus lenses.
It’s not just a matter of opinion that optometry should be first to introduce patients to this information—research backs the idea. If the patient is feeling well cared for and well-informed beginning with their primary eye care provider, overall satisfaction tends to score higher, according to a Journal of Cataract and Refractive Surgery study.5,12 Anecdotally, we have found that the better ODs prepare a patient, the smoother the process, and the better it reflects on the optometrist. Repetition of information over time allows the patient to slowly absorb and process the information that will heavily impact their quality of life in the future.
What’s to Come?Newer IOL technology in the pipeline looks to shake up the status quo yet again. Below are but a few of the hopeful distruptors. 1. Light-Adjustable Lens (RxSight). This was FDA approved this year, but is not yet on the market. It’s the first lens that allows postoperative adjustments to address uncorrected visual acuity or even undecided visual endpoints. The lens is made of a photoreactive silicone that allows optical changes to be induced postoperatively.21 2. Eyhance monofocal IOL (Johnson & Johnson Vision). This lens aims to target the monofocal market with a mild extension toward intermediate vision using an aspheric lens design and broader defocus curve rather than a diffractive design. The purported benefit is improved “sweet spots” postoperatively compared to current monofocal IOLs. This lens may be optimal for those who do not mind wearing readers for near function and some intermediate tasks, but do not want to deal with adapting to diffractive halos and decreased contrast sensitivity. While not yet FDA approved, it has been released into the European market since February 2019.22 3. IC-8 Small Aperture Lens (AcuFocus). This lens uses the same technology as the Kamra corneal inlay to extend the depth of focus via pinhole effect. The lens is currently proceeding with clinical trials in the U.S. estimated to be completed in May of 2020. European studies have shown up to 2.25D range of focus.23,24 |
IOLs for Presbyopia
There are several categories of presbyopia-correcting IOLs on the market:
Diffractive multifocals. These lenses use several optical zones with different powers to establish separate focal points. While multifocals will offer better distance and near function (+2.50D range), some patients complain of a lack in clarity for intermediate activities. These include the Tecnis Multifocal (Johnson & Johnson Vision) and Acrysof IQ Restor (Alcon).
Extended-depth-of-focus IOLs. The Tecnis Symfony IOL (Johnson & Johnson Vision) lays claim to this category as an improvement upon conventional multifocal IOL performance. The lens uses chromatic aberration to create smoother transitions between its optical zones and fewer “dead zones” where vision is non-functional between set focal points. Surgeons estimate it provides around +1.50D of range, requiring the patient to wear readers for detailed near activities like threading a needle or beading.
Accommodating or pseudo-accommodating IOLs. In this approach, used in the Crystalens AO and Trulign Toric from Bausch + Lomb, a flexible lens bows forward, increasing the focusing power enough to improve near function of about +1.00D or more.
Trifocal IOLs. Though popular overseas for several years, this option has only recently come to our shores when Alcon launched its PanOptix IOL a few months ago. The design is said to deliver improved quality of distance, intermediate and near function compared to previous generations of multifocal IOLs.13 PanOptix has three target focal points at optical infinity, 60cm and 40cm. It comes in both spherical and toric platforms, as do the Restor 2.5 and Restor 3.0. However, PanOptix has unique technology to use more of the incoming light.
Monovision. As with contact lenses, monofocal IOLs can be chosen to establish one eye for distance and one eye for near or intermediate. If the patient’s non-dominant eye has good tolerance for blur, combining a dominant single-focus IOL with a non-dominant diffractive lens may allow the patient further freedom from spectacle wear.
Mix-and-match. Taking it a step further, personalizing vision with a multifocal lens in one eye for better near function paired with an EDOF or trifocal lens in the other may allow full range of vision by supplementing the intermediate zone. The possibilities are endless, but careful assessment of clinical findings is important in ruling out those with contraindicated findings.14
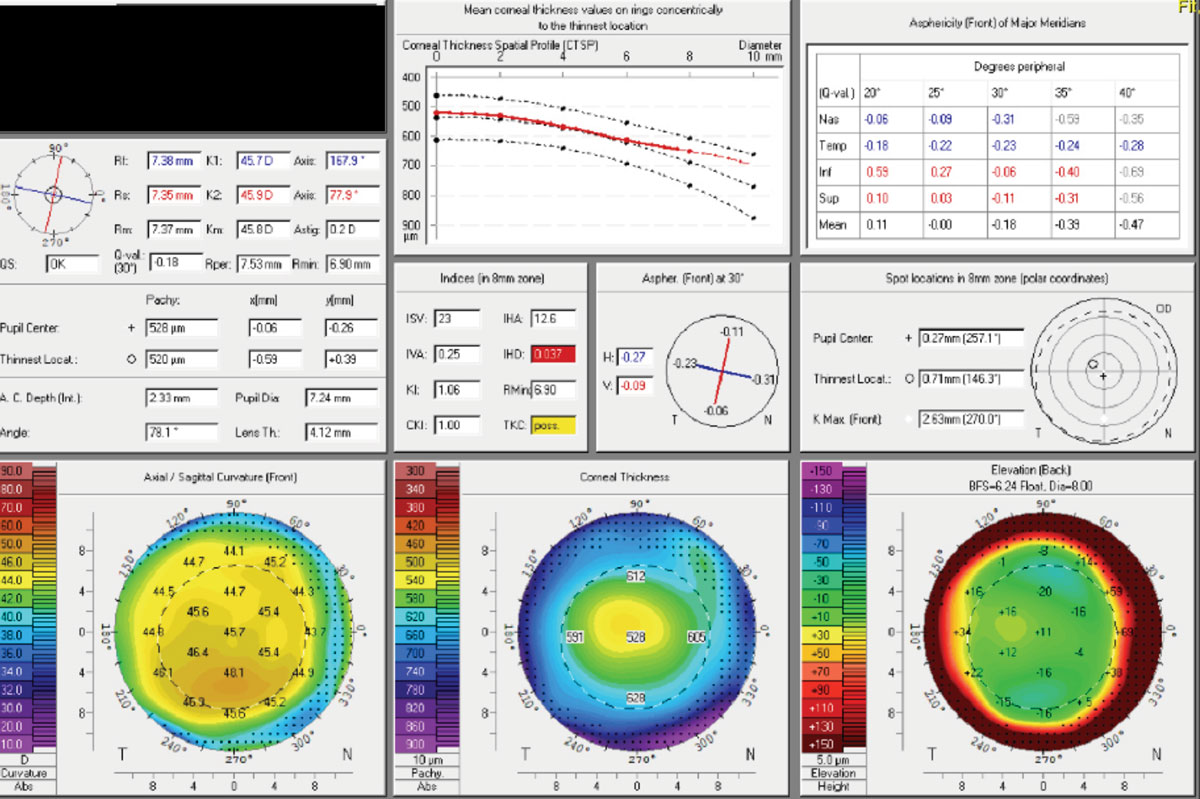 |
| Forme fruste keratoconus can be subtle and is often missed in routine eye exams. Tools such as the Pentacam help identify those with irregular astigmatism as these patients are contraindicated for toric and presbyopia-fixing IOLs. Click image to enlarge. |
The goal is to minimize patients’ need for corrective lenses according to their distinct lifestyle requirements. Unfortunately, there is no lens that can completely guarantee absolute freedom from glasses 100% of the time. As the primary care provider, it is important to emphasize a personalized strategy that best matches the patient’s goals while establishing limitations. Reasons for Dissatisfaction
Even if you’ve done your job right prior to cataract surgery—evaluated patients thoroughly for ocular surface disease, explained the benefits and shortcomings of their chosen lens option and prepared them for a neural adaptation period—the patient may still experience dissatisfaction with a premium IOL. Luckily, many of the following postoperative complications are treatable.
Most easily detected is residual refractive error. Once stability of the cornea is established with topography and manifest refraction, the patient can enhance their acuity with LASIK or PRK, which is much more customizable and predictable compared to cataract surgery. Enhancement procedures are often reviewed with patients who have a history of more than two years.
Secondly, and most easily treated, is posterior capsular opacification, which can occur in up to 40% of patient following cataract surgery.15 Hazing of the posterior capsule is typically more common in younger patients, as well as those with diabetes, history of uveitis, and traumatic cataracts.16-19 The typical complaint consists of slow return of glare and blur in vision after a period of clarity following cataract surgery.
Preparing the patient ahead of time about the risks and potential treatments alleviates the misunderstanding that the original cataract surgery “didn’t work.” Instead, the YAG capsulotomy becomes an anticipated step in clearer vision. Time of treatment may vary based on surgical clinics, but the general rule is that it’s safe to proceed once there is enough peripheral capsule scarring and fibrosis to secure the intraocular lens, which may take up to three months.
A more frustrating post-op complication is cystoid macular edema, also known as Irvine-Gass syndrome. Preventative care with a non-steroidal anti-inflammatory drug, in addition to the typical steroid and antibiotic combination, is used to minimize inflammatory reaction by disrupting the prostaglandin cascade. Fortunately, vision loss is usually temporary and responds quickly to restarting topical anti-inflammatory therapy. More severe or stubborn cases may require intravitreal injections with retina specialist. The most important thing as a primary eye care provider is to catch the presentation early as visual prognosis is better the sooner treatment is initiated.20
Lastly, even if there are no post-op complications, the patient may still be upset. The abundance of information that the patient considers at the cataract evaluation may lead to key concepts being forgotten—for example, the loss of near function in monofocal IOL use. In addition, they may hear “miracle” stories from friends and family members that are not realistic for their own case. Therefore, repetition of information over several visits with their primary eye care provider is important in allowing the patient to absorb the important key points fully before surgery.
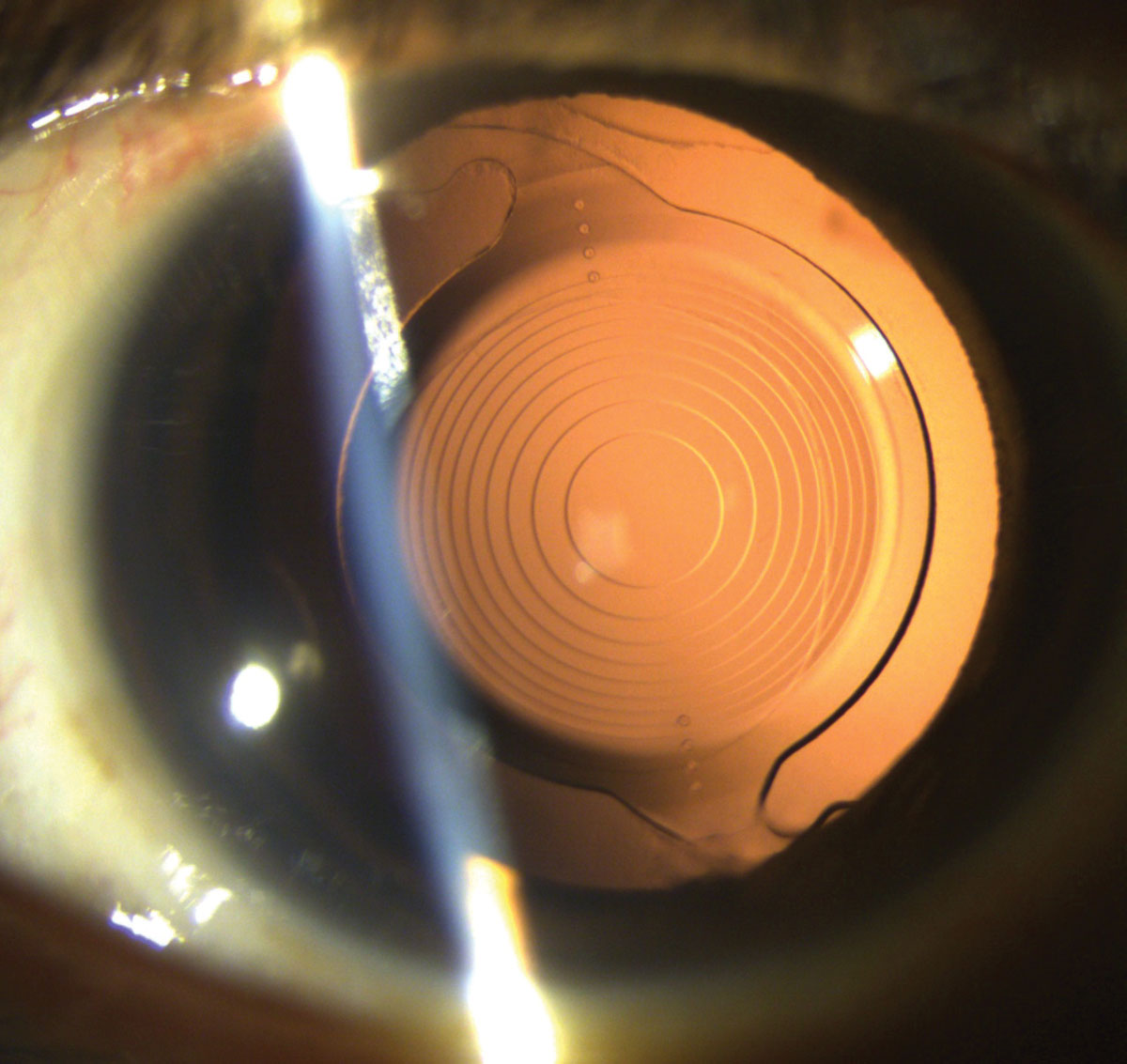 |
| This patient’s Toric Symfony IOL was implanted one day before this photo was taken. Click image to enlarge. |
It Starts With Us
Unfortunately, no matter how much we try, there is no way of determining which patients will absolutely adapt well to a premium lens. Most information is gained through the process of discussing patients’ expectations and visual goals. Keep in mind that, although someone is clinically a good candidate for a premium lens on paper, their lifestyle and personality may exclude them. The more you can understand their hobbies, occupational requirements, and are able to determine which visual functions are most important to change, the more likely they will be matched with the proper IOL.
Though patients are becoming more accustomed to doing their own research, they may only be reading the manufacturer information, which tends to leave out the potential negatives of their product. It is essential that the eye care provider educate the patient about the compromise and gains of the options. If they are unable to give up sharp near function without need for glasses, then they may ultimately be a better candidate for monofocal IOLs with near endpoints or monovision if they have a history of success using soft contact lenses. The additional chair time that it takes in the initial discussion will save you and the patient a lot of time and frustration in trying to fix or adapt to an “unexpected” visual outcome.
Individuals with higher distance visual demands (e.g., sharp shooters, photographers, long haul truck drivers, historical emmetropes) tend to struggle with the lower contrast sensitivity and haloing effects of the presbyopia-correcting IOLs. Instead, they tend to prefer the sharpness of monofocal lenses, certainly opting for astigmatism correction to neutralize astigmatic aberrations. In particular, those who spend a lot of time in scotopic settings; for example, truck drivers often have to drive long distances at night. Postoperative halos and starbursts from multifocal and extended depth of focus lenses may make it very difficult for them to perform their job safely.
On the other end of the spectrum, it is easy to fall into the trap of prioritizing distance vision for all patients. Myopic patients who enjoy near tasks such as crafting, reading, computer use or hairstyling may prefer to remain with an intermediate (-1.25D) or near (-2.50D) endpoint. This is a great opportunity to trial different options using soft contact lenses to simulate the loss of these working distances if they opt for distance vision.
As the primary eye care provider, consider beginning the process of determining lens selection early, when cataracts are first detected but before the patient is symptomatic. Build rapport and patient loyalty by addressing their long-term needs early on. Begin the conversation on what their ideal vision would be within the limitations of the current technology. Start trialing different modes of vision from monovision to multifocal to single focus or even a multifocal/single focus combination.
The early conversation and the ability for the patient to functionally trial their options will make the whole process a lot less foreign and confusing when it actually comes time for surgery. Trialing each option for a week with your patient will help them easily rule out the option of monovision or premium lenses if they are unable to adapt.
At times, the different lens options and packages that are reviewed at the time of surgery can be overwhelming. Our job as the primary care doctor of optometry is to guide them to the right choice. In the words of Malcolm Gladwell, we, as doctors, are “in the relationship business.” We have the opportunity to spend more time with a patient in an exam setting than other health care professions listening and learning their needs and goals. Furthermore, we have the amazing privilege of altering the way they see the world in the blink of an eye by providing personalized lifestyle vision.
Dr. Roan is a staff optometrist at Pacific Cataract & Laser Institute in Bellevue, WA.
1. Samadi B, Lundstrom M, Kugelberg M. Improving patient-assessed outcomes after cataract surgery. Euro J Ophthalmol. journals.sagepub.com/doi/abs/10.5301/ejo.5000927. March 1, 2017. Accessed November 2, 2019. 2. Kirwan C, Nolan J, Stack J, Moore T, Beatty S. Determinants of patient satisfaction and function related to vision following cataract surgery in eyes with no visually consequential ocular co-morbidity. Graefes Arch Clin Exp Ophthalmol. 2015;253(10):1735-44. 3. AcrySof IQ Toric [product information]. MyAlcon. www.myalcon.com/professional/cataract-surgery/intraocular-lens/acrysof-iq-monofocal-iol/biomaterial. 2009. 4. Rudalevicius P, Lekaviciene R, Auffarth G, Liutkeviciene R, Jasinskas V. Relations between patient personality and patients’ dissatisfaction after multifocal intraocular lens implantation: clinical study based on the five factor inventory personality evaluation. Eye (Lond). September 20, 2019. Accessed November 2, 2019. 5. Brga-Mele R, Chang D, Dewey S, et al. ASCRS Cataract Clinical Committee Multifocal intraocular lenses: relative indications and contrainidcations for implantation. J Cataract Refract Surg. 2014;40:313-22. 6. Jordan L. Whither monofocal toric IOLs? Rev Ophthalmol. 2018;25(3):32-4. 7. Ho V, Stanojcic N, O’Brart N, O’Brart D. Refractive surprise after routine cataract surgery with multifocal IOLs attributable to corneal epithelial basement membrane dystrophy. J Cataract Refract Surg. 2019;45(5):685-9. 8. Bakewell B. Dealing with zonular dehiscence. EyeWorld. www.eyeworld.org/article-dealing-with-zonular. March 2011. Accessed November 2, 2019. 9. Potvin R, Kramer B, Hardten D, Berdahl J. Toric intraocular lens orientation and residual refractive astigmatism: an analysis. Clin Ophthalmol. 2016;10(9):1829-36. 10. Kaur M, Shaikh F, Falera R, Titiyal J. In J Ophthal. 2017;65(12):1301-13. 11. Kent C. Toric IOLs: More options, more patients. Rev Ophthalmol. 2014;21(1):20-69. 12. Nijkamp M, Nuijts R, Borne B, et al. Determinants of patient satisfaction after cataract surgery in three settings. J Cataract Refract Surg. 2000:6(9):1379–88. 13. Smith S, Overby B. Alcon Introduces AcrySof IQ PanOptix Trifocal IOL in the U.S., the First and Only FDA-Approved Trifocal Lens. www.alcon.com/media-release/alcon-introduces-acrysof-iq-panoptix-trifocal-iol-us-first-and-only-fda-approved. August 27, 2019. Accessed November 2, 2019. 14. Walter K. Refractive cataract surgery: success through Technis personalized vision. Ophthalmol Times. www.ophthalmologytimes.com/sites/default/files/legacy/mm/digital/media/OT-JJV-Walter.pdf. 2018. Accessed November 2, 2019. 15. Steinert R. Nd:YAG laser posterior capsulotomy. American Academy of Ophthalmology. www.aao.org/munnerlyn-laser-surgery-center/ndyag-laser-posterior-capsulotomy-3. November 4, 2013. Accessed November 2, 2019. 16. Pandey S, Apple D, Werner L, et al. Posterior capsule opacification: A review of the aetiopathogenesis, experimental and clinical studies and factors for prevention. Ind J Ophthalmol. 2004;52:99-112. 17. Ebihara Y, Kato S, Oshika T, et al. Posterior capsule opacification after cataract surgery in patients with diabetes mellitus. J Cataract Refract Surg. 2006;32(7):1184-7. 18. Rahman I, Jones N. Long-term results of cataract extraction with intraocular lens implantation in patients with uveitis. Eye. 2005;19(2):191-7. 19. Krishnamachary M, Rathi V, Gupta S. Management of traumatic cataract in children. J Cataract Refract Surg. 1997;23(Suppl 1):681-7. 20. Wittpenn J, Silverstein S, Heier J. A randomized, masked comparison of topical ketorolac 0.4% plus steroid vs steroid alone in low-risk cataract surgery patients. Am J Ophthalmol. 2008 Oct;146(4):554-560. 21. Bethke W. RxLAL: Say Goodbye to Postop Surprise? Rev Ophthalmol. 2018;25(1):12-66. 22. Findl O. Surgeon finds new monofocal IOL lands in a visual sweet spot. Ophthalmol Times. www.ophthalmologytimes.com/iols/surgeon-finds-new-monofocal-iol-lands-visual-sweet-spot/page/0/1. September 3, 2019. Accessed November 2, 2019. 23. Study of S-649266 or Best Available Therapy for the Treatment of Severe Infections Caused by Carbapenem-resistant Gram-negative Pathogens (CREDIBLE - CR). clinicaltrials.gov/ct2/show/NCT03633695. April 25, 2019. Accessed November 2, 2019. 24. The IC-8 IOL. crstodayeurope.com/wp-content/uploads/sites/5/2017/09/0917CRSTEuro_insert_AcuFocus.pdf. Cataract Refract Surg. September 2017. Accessed November 2, 2019 |

