 |
Amiodarone is one of the most effective medications to treat ventricular and supraventricular arrhythmias. Long-term use, however, is associated with vision loss secondary to optic neuropathy.
 |
| Both optic nerves are hyperemic and have blurred temporal margins, OD>OS. Click image to enlarge. |
Case Report
A 66-year-old Caucasian male presented with blurry vision that had gradually worsened over the past two months. He was unsure if this was a monocular or binocular phenomenon and had not found relief with glasses.
The patient’s health history was positive for myocardial infarction and coronary artery stenting two years prior. He was taking amiodarone and apixaban for paroxysmal atrial fibrillation, lisinopril and metoprolol for hypertension, metformin for type 2 diabetes and atorvastatin for hyperlipidemia. He undergoes continuous positive airway pressure therapy for obstructive sleep apnea.
Clinical Examination
Corrected visual acuities were 20/20 OD and 20/25+2 OS, intraocular pressures were 16mm Hg OD and 17mm Hg OS, blood pressure was 161/94mm Hg and heart rate was 56bpm. Anterior segment exam revealed grade two whorl keratopathy OD and grade one OS. Dilated lens exam revealed grade two nuclear sclerosis OU.
The right optic nerve had a small cup-to-disc ratio (0.1/0.1) with hyperemic, blurred temporal margins. There was noticeable nerve head elevation with edema temporally and multiple small flame hemorrhages. C/D ratio OS was also small (0.15/0.15) with a crowded appearance and mild hyperemia superiorly and inferiorly. The left disc margins were distinct and without hemorrhages. Macular disease was not present OD, and only mild pigmentary changes were observed in the left macula. There was a small choroidal nevus with benign features in the posterior pole OS.
Though OCT of the retinal nerve fiber layer (RNFL) was normal at first glance, the square appearance and dark color of the thickness map raised further suspicion for disc edema OD. The map revealed asymmetric average RNFL thicknesses, with the right eye measuring 10µm greater than the left, and overall low retinal thickness most evident superior and temporal to the optic nerve, sparing the central foveal subfield.
Visual field testing OD revealed normal threshold sensitivities with a few peripheral points of decreased sensitivity that did not display clinically significant patterns. Testing of the left eye revealed an inferonasal area of low sensitivity, which may be indicative of prior optic neuropathy and influenced by age-related macular degeneration.
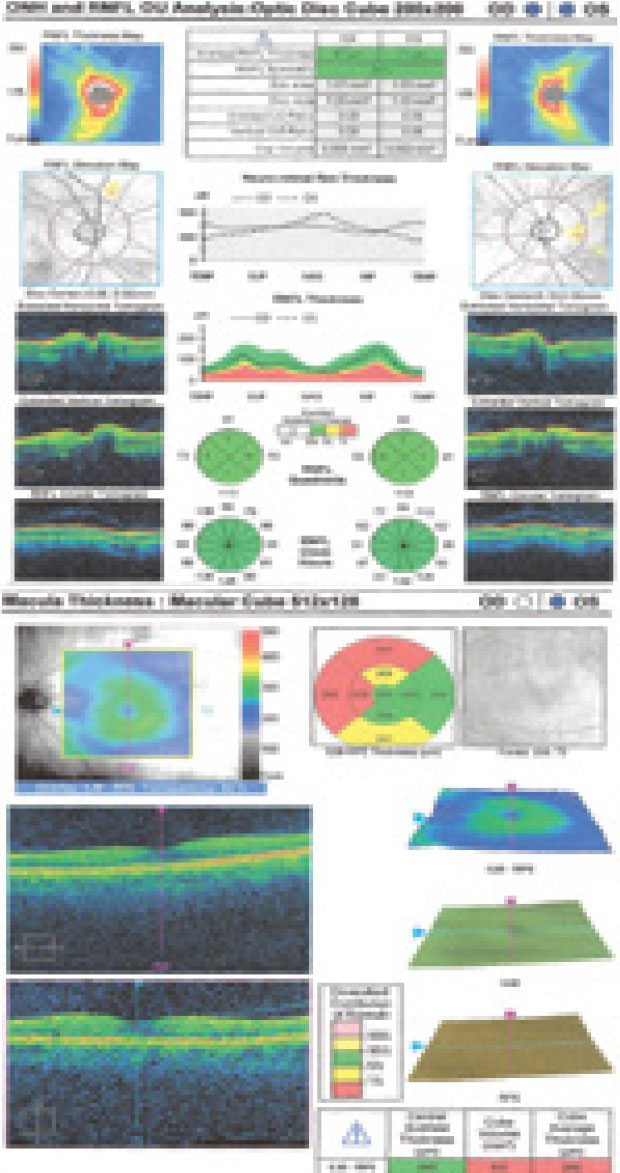 |
| RNFL thickness findings on OCT. Click image to enlarge. |
Patient Outcome
Serologic testing to rule out infectious and inflammatory etiologies showed normal results. Magnetic resonance imaging and venography showed no signs of abnormality.
The patient’s cardiologist elected to discontinue amiodarone and continue apixaban and metoprolol. He inserted a heart monitor to detect atrial fibrillation, which did not recur.
A neuro exam revealed a superior altitudinal visual field defect using a 30mm red target (OD>OS) and a 40% decrease in red desaturation OD. Repeat visual field testing did not show any significant defects. The assessment corroborated the concern for amiodarone-associated optic neuropathy (AAON). The patient was followed closely by his team and showed slow improvement and eventual resolution of the disc edema OD over three months.
A Drug That Gives and Takes
Heart disease is the leading cause of death in the US, affecting millions of Americans.1 Luckily, therapies such as amiodarone can help those with life-threatening cardiac arrhythmias.1 Amiodarone is the most widely prescribed antiarrhythmic in the US.2,3 Unfortunately, the drug’s efficacy may come at a price.
Oral amiodarone is lipophilic and has a half-life of 60 to 142 days.3,4 Because of its biphasic properties, it interferes with the movement of phospholipids across the intracellular membrane and accumulates in membrane-rich structures.1 Its toxins can negatively affect tissues throughout the body.5 Prolonged use is associated with pulmonary toxicity, thyroid dysfunction, peripheral neuropathy, tremor, ataxia with staggering gait, gastrointestinal disturbances and ocular manifestations.5,6
Ocular changes are common, with the majority developing verticillate keratopathy. Patients taking moderate to high doses may develop anterior subcapsular cataract. Maculopathy has also been reported.
 |
| Visual field testing results. Click image to enlarge. |
Optic Neuropathy Look-alikes
AAON’s presentation is highly variable; tit may appear as unilateral or bilateral optic disc swelling with hemorrhages.1,4 Clinical manifestation typically begins within 12 months of the start of therapy, with a median onset of four months for subtle, mild vision loss that gradually resolves over another few months.
Typical characteristics include insidious onset of visual loss and bilateral protracted disc edema over months. A wide spectrum of optic nerve involvement is possible. Some patients are asymptomatic while others have substantial visual dysfunction, with either acute or insidious vision loss, and simultaneous bilateral or sequential disc edema.1,6,7 Conflicting evidence exists regarding acuity stabilization and visual field defect resolution in patients with AAON, but early detection and amiodarone discontinuation could make a difference in visual prognosis.1,5,6
Because many patients taking amiodarone often have associated vascular risk factors, clinical distinction from non-arteritic anterior ischemic optic neuropathy (NAION) can be a challenge.7 NAION is the most common acute optic nerve disorder in patients over 50. It results from ischemic insult to the nerve head and is characterized by acute, monocular, painless vision loss with disc swelling.8 Risk factors include previous NAION, sleep apnea, older age, HLA-A29 antigen, chlamydia, diabetes, oral fever blisters, hypertension and small, crowded optic nerves.8
NAION occurs equally among men and women, while AAON is more common in men. Disc edema in NAION generally resolves within weeks, while it could take months to fully clear up in AAON. Unlike with AAON, neurological signs are absent in NAION.7,8 Mean visual acuities tend to linger around 20/60 in NAION and 20/30 in AAON.
The distinction between AAON and NAION remains controversial, as characteristics overlap. Clinicians must act on ocular changes in amiodarone users by identifying them early and considering drug discontinuation for the best outcomes.
Dr. Hyatt is in private practice in San Antonio, TX. She is a Fellow of the American Academy of Optometry (AAO).
Dr. Slagle is the supervisor of the Salem VA Medical Center’s optometry residency program. He is a Fellow of the AAO.
Dr. Hui is in private practice in Illinois.
Dr. Greene practices at the Salem VA Medical Center and supervises optometry interns and residents.
1. Murphy MA, Murphy JF. Amiodarone and optic neuropathy: the heart of the matter. J Neuro-Ophthalmol. 2005;25(3):232-6. 2. Mansour AM, Puklin JE, O’Grady R. Optic nerve ultrastructure following amiodarone therapy. J Neuro-Ophthalmol. 1988;8(4):231-8. 3. Giardina EG, Passman R. UpToDate. Amiodarone: clinical uses. www.uptodate.com/contents/amiodarone-clinical-uses. Accessed February 4, 2020. 4. Cheng HC, Yeh HJ, Huang N, et al. Amiodarone-associated optic neuropathy: a nationwide study. Ophthalmology. 2015;122(12):2553-9. 5. Wang AG, Cheng HC. Amiodarone-associated optic neuropathy: clinical review. Neuro-Ophthalmology. 2017;41(2):55-8. 6. Johnson LN, Krohel GB, Thomas ER. The clinical spectrum of amiodarone-associated optic neuropathy. J Natl Med Assoc. 2004;96(11):1477-91. 7. Purvin V, Kawasaki A, Borruat FX. Optic neuropathy in patients using amiodarone. Arch Ophthalmol. 2006;124:696-701. 8. Madhura T, Volpe NJ. UpToDate. Nonarteritic ischemic optic neuropathy: prognosis and treatment. www.uptodate.com/contents/nonarteritic-ischemic-optic-neuropathy-prognosis-and-treatment. Accessed February 4, 2020. |

