 |
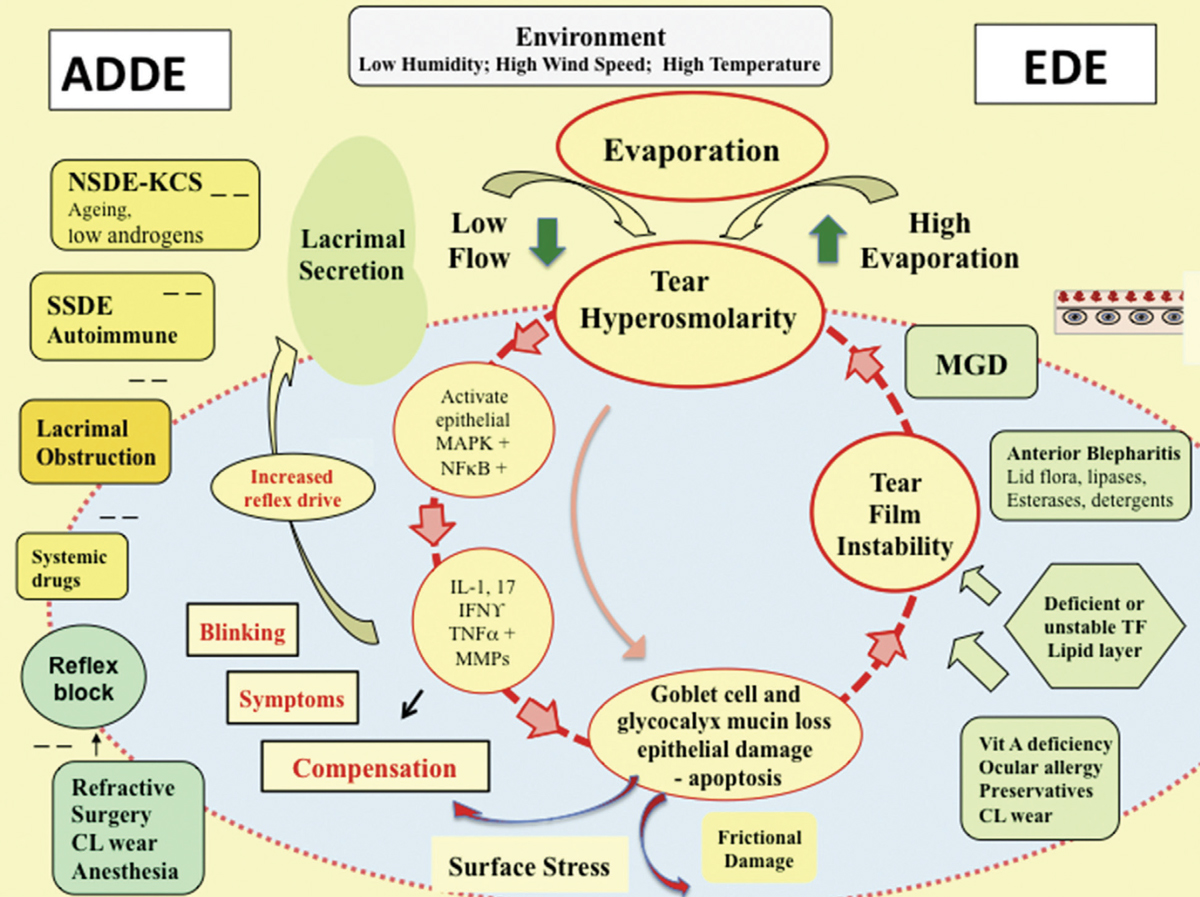
| Hyperosmolarity plays a pivotal role in the complex pathogenesis of dry eye disease. Photo: From Ocular Surface (2017) 441–515, Bron AJ, de Paiva CS, Chauhan SK, et al. TFOS DEWS II pathophysiology report, p. 460. Click image to enlarge. |
A recent study in Australia analyzed the largest sample of tear film osmolarity measurements in patients—standard and post-refractive—undergoing dry eye assessment prior to refractive procedures. The researchers believed that the analysis of a broad range of subjects is necessary to promote understanding of the relationship between tear film osmolarity and dry eye parameters. Although the majority of patients can be expected to fall within normal ranges, the team determined a reasonable percentage will be diagnosed with tear hyperosmolarity and therefore are at risk of DED.
The study reviewed 1,404 patients (1,357 standard and 47 post-refractive) who underwent screening for laser refractive surgery. Tear film osmolarity was conducted and patients refrained from eye drops two hours beforehand. The mean age of the standard population was 39.00 compared with the post refractive group 51.89. The overall mean preoperative spherical equivalent was -2.78DS and mean keratometry was 43.52D.
The researchers found that 82.6% of patients in the standard population remained below the standard cut-off point for hyperosmolarity (308mOsm/L), which suggested that tear film homeostasis is common in younger, healthy patients.
“Of interest to a clinical diagnosis of DED, the average inter-eye difference of our cohort was 8.17mOsm/L—a marker of unstable tear film,” the authors explained. “Although only 31.6% of patients recorded a difference above 8mOsm/L, over half of the patients had at least one eye above the standard threshold for hyperosmolarity, confirming the likelihood that hyperosmolar patients will exhibit significant asymmetry between eyes.”
Age appeared to impact mean tear film osmolarity values. The researchers broke down the study population by age to reflect the potential surgery population and the plausible impact on the accuracy of outcomes (i.e., 40 and younger to represent a corneal refractive population and 40 and older a lens-based procedure).
“The mean difference between eyes indicated increasing hyperosmolarity with time,” the authors explained. “Although both populations on average retained normal tear film osmolarity values, patients more appropriate to lens-based procedures may have subtle hyperosmolarity concerns.” They added this may impact the number of patients requiring tear film optimization prior to cataract surgery, but further studies are required.
The study found a positive correlation between tear film osmolarity and subjective assessment (Ocular Surface Disease Index) in the standard population but not the post-refractive surgery cohort. That the majority of osmolarity values remained below the threshold for hyperosmolarity in all OSDI classifications suggested additional factors outside clinical dry eye signs contributing to the patient’s level of ocular surface disease comfort. Of note, a greater percentage of patients in the standard group reported a previous experience of dry eye compared with the post-refractive cohort. The team suspects that routine contact lens wear, significantly higher in the standard cohort, may represent the main consideration in the patient response (58.4% vs. 17.0%).
Authors also found a history of contact lens wear resulted in a significantly lower tear film osmolarity value compared with non-wearers, showing that osmolarity may be altered by contact lenses. However, if the patient is in good health, it’s not likely to be a significant difference.
Xuan R, Franzco ML, Franzco GS, Hodge C. Prevalence of tear film hyperosmolarity in 1,150 patients presenting for refractive surgery assessment. J Cataract Refract Surg. August 9, 2021. [Epub ahead of print]. |

