 |
History
A 52-year-old Caucasian female presented with a chief complaint of blurry vision in both eyes at distance and near of five months duration. She reported no trauma. While she reported having been diagnosed with pseudoxanthoma elasticum, she explained she was taking no medication for it, nor was she seeing a physician for it. She reported using bisacodyl for constipation. She denied allergies of any kind.
Diagnostic Data
Her best-corrected visual acuities were 20/80 OD and 20/150 OS. Pupils were round, equal in size, and reactive to light without an afferent pupil defect. Extraocular muscles exhibited full range of motion. Confrontation visual fields were full to finger counting OU with some blur reported using the facial Amsler.
Refraction uncovered negligible hyperopia with presbyopia, not improving visual acuity. Biomicroscopy found normal anterior segment structures with mild nuclear cataracts, both eyes.
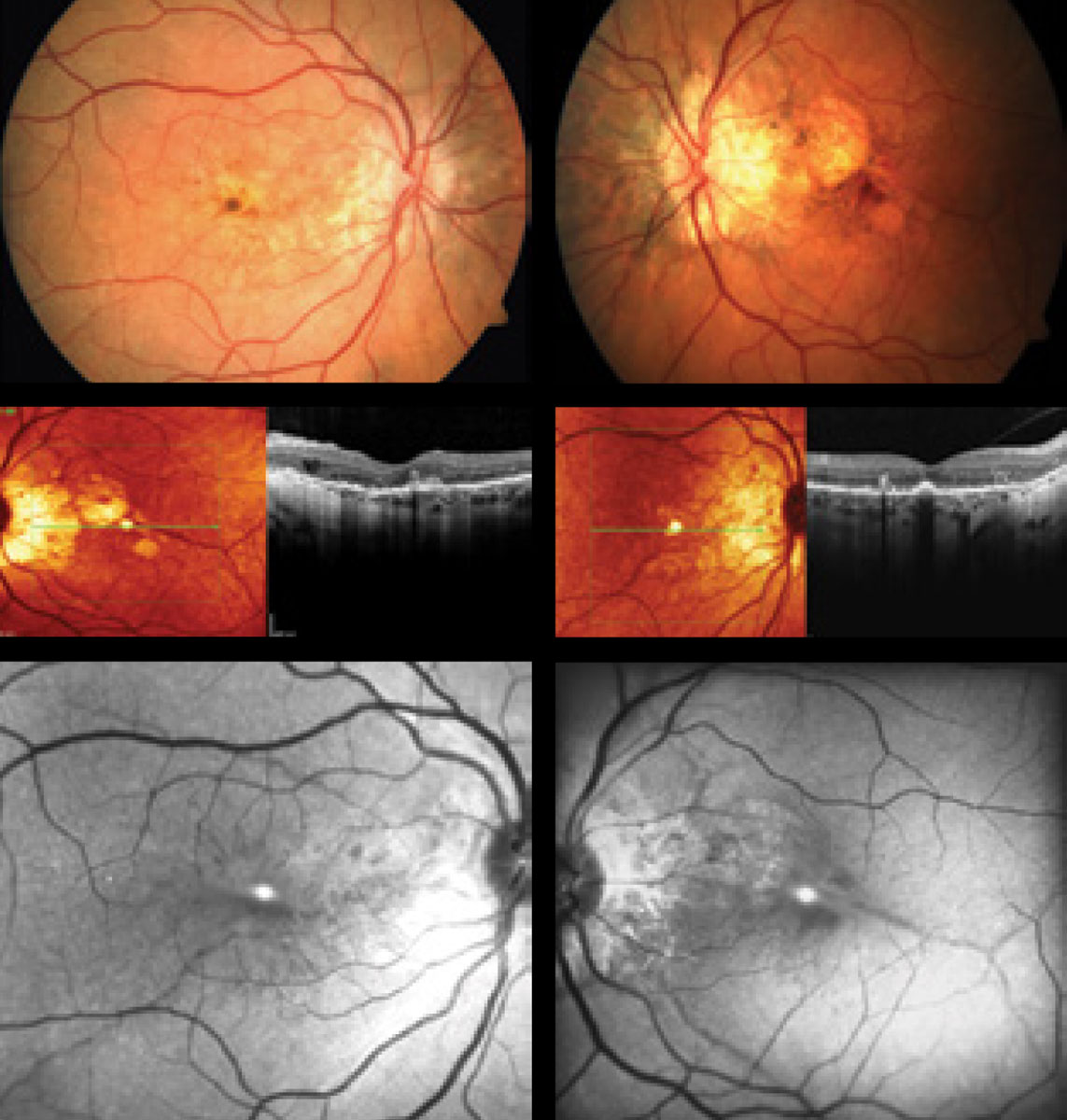
The pertinent posterior segment findings are demonstrated in the photographs.
 |
How can this 52-year-old patient’s posterior segment findings help explain her five months of blurry vision? |
Discussion
The diagnosis in this case is bilateral choroidal neovascular membrane (CNV) secondary to angioid streaks (AS).
Pseudoxanthoma elasticum (PXE), also known as Grönblad–Strandberg syndrome, is an autosomal recessive genetic disorder characterized by degeneration and mineralization of the body’s elastin fibers. Elastin is a protein found throughout the body including the skin, eyes, and blood vessels. Estimated prevalence of PXE is 1 in 25,000 to 100,000.1 It is estimated that women are twice as likely to inherit PXE as men.1 This female predilection is not, however, entirely understood. Diagnosis of PXE is made by skin biopsy or genetic testing. Typically, stains such as Von Kossa or Verhoeff’s are used to evaluate calcium or elastin, respectively. A defect in the ABCC6 gene on chromosome 16p13.1 has been associated with PXE inheritance.2 The ABCC6 gene is an organic anion transporter protein, and a defect within this gene can cause PXE.3
Those affected by PXE can present with a myriad of systemic findings. PXE can affect a wide range of organs, primarily targeting the skin, cardiovascular system, and eyes. In a small subset of individuals, gastrointestinal hemorrhage also presented as a complication with these patients. Early dermatological findings include yellowish, raised lesions, typically observed around the neck.3These lesions are often described as having a “plucked chicken” appearance. It is also not uncommon for individuals to present with multiple skin folds, typically located around the neck or armpit region. Due to excess arteriolar calcification of small to medium sized arteries, individuals will sometimes suffer with complications related to the cardiovascular system. Cardiovascular complications include, but are not limited to, angina pectoris, hypertension, mitral-valve prolapse and restrictive cardiomyopathy.3 Excessive calcification of arteries is presumably the cause of myocardial infarction in these patients. This is a rare, yet potentially fatal condition.3
Although PXE has a wide variety of systemic findings, it presents with a number of ocular findings that include: AS with secondary CNV, peau d’orange, drusen of the optic nerve head, and comet tail lesions (chorioretinal atrophy, salmon spots).4 Additionally, Agarwal et al. discovered that more than 70% of eyes in patients with PXE showed degenerative changes of the retinal pigment epithelium (RPE) that resembled pattern dystrophies.5 AS are the most renowned ocular finding in PXE, often appearing between the ages of 15 and 25 years.6 They are referred to as angioid due to their resemblance to blood vessels. Histologically, AS are the result of 50-500um of thickening, or more specifically, generalized heavy calcification of elastin fibers in Bruch’s membrane, appearing as reddish brown or gray-like streaks that course from the optic nerve.2,4 As a result, the entire retina is structurally compromised due to localized atrophy of the RPE and choriocapillaris, making these patients more susceptible to choroidal neovascular membrane (CNV) formation.4 Less prominent AS can be differentiated funduscopically from blood vessels by their depth. AS lie deeper than the retinal blood vessels and will thus cross underneath them.
The prevalence of AS in individuals with PXE approaches 100%.7,8 It is estimated that the development of CNV in patients who have AS varies between 72 to 86%.4 Since Bruch’s membrane is brittle from mineralization, individuals are more prone to retinal hemorrhage and CNV from even the most minor of trauma.9 By comparison studies have shown that the incidence of CNV after trauma is around 15%.10
Although many systemic conditions are associated with AS, Ehlers Danlos, Paget’s disease, and sickle-cell hemoglobinopathies are notable differentials, along with pseudoxanthoma elasticum.2 Ehlers Danlos is a heritable group of connective tissue disorders which affect the collagen integrity of bone, skin, blood vessels, and other organs. These individuals also have skin hyperextensibility and fragility as well as fragile bones.11 Paget’s disease is a genetic, metabolic bone disease in which there is chronic bone resorption and regrowth resulting in a structurally weakened and more vascular skeleton. Affected individuals can present with hearing loss and deformities of the skull and weight bearing bones.12 Sickle cell hemoglobinopathes affect red blood cells causing them to become crescent shaped and oxygen deprived. AS in these patients are hypothesized to be correlated with calcium deposition at the level of Bruch’s membrane.2 Other notable ocular findings include salmon patch hemorrhages, vascular occlusions and sea fan neovascularization.13 Although the previous conditions mentioned are the main diseases associated with AS, they can also be idiopathic in nature. The mnemonic PEPSI (Paget’s, Ehlers, Pseudoxanthoma, Sickle Cell and Idiopathic) is effective to quickly recall the major etiologies associated with AS.
Another ocular finding associated with PXE is peau d’ orange or leopard skin spotting. It is observable as mottling of the retina temporal to the macula. This phenomenon appears to precede the formation of AS and can be found in patients as young as 10.14,15 Spontaneous degradation of the RPE and Bruch’s membrane complex can lead to geographic atrophy with or without the presence of CNV. The mechanism of this atrophy is not well understood.14 Finally, those with PXE are prone to the formation of optic nerve head drusen. It is estimated that 0.3% of individuals in the general population have optic nerve head drusen compared to roughly 20% of PXE patients.15
Multimodal Imaging is useful in highlighting different pathological retinal processes in these cases and includes fundus autofluorescence (FAF), cross-sectional and en face optical coherence tomography (OCT), and optical coherence tomography angiography (OCT-A).
FAF provides the ability to visualize RPE-photoreceptor damage in.2 Specifically, FAF highlights over-production and accumulation of pathological fluorophores in the RPE, such as lipofuscin, in which an increased amount can be attributable to certain ocular diseases.16 Fluorophores emit light in response exposed to certain wavelengths. In the generalized interpretation of an FAF image, the retina may exhibit signs of hyperfluorescence as well as areas of hypofluorescence. Hyperfluorescence can result from the increased production of lipofuscin, retinal drusen, or defects in the photoreceptors and RPE causing a window type defect.16,17 Lipofuscin is a metabolic waste product produced by the RPE cells from breakdown of photoreceptor outer segments. This is normally a product of the retina, but accumulation of this by-product can be a sign of damage to the deep retina. On FAF significant AS may appear attenuated/hypofluorescent due to injury to remaining RPE cells and subsequent loss of pigment granules from which autofluorescence could be previously captured.2 Viewing smaller streaks may be difficult due to the RPE, whose integrity is mostly intact in these instances, absorbing some of the light.2 Optic disc drusen will exhibit hyperfluorescence on FAF, likely as a result of the increased buildup of minerals.17Cross-sectional and en face OCT in patients with PXE can better delineate deep retinal and choroidal changes.18,19 These changes include: Hyper-reflective lesions in the subretinal space resembling subretinal drusenoid deposits, breaks in Bruch’s membrane with preservation of overlying RPE, pockets of subretinal fluid not associated with CNV, outer retinal tubulation, and absence of visualization of the external limiting membrane or photoreceptor integrity line.18 En face OCT permits localization of lesions at specific subretinal layers, using their axial location on OCT cross sections.19 En face has been specifically shown to locate AS as a structural defect in Bruch’s membrane, as well as to determine the spatial relationship between AS and CNV.19
OCT-A is a non-invasive imaging technique that demonstrates flow characteristics of the retinal and choroidal vasculature network with greater precision than dye angiography.8 OCT-A has been proven to delineate CNVs closely correlated to the site of AS and adds an additional tool to monitor these patients.8
Ocular treatments involve the use of anti-VEGF agents for treating potential CNV. There are no known contraindications for the treatment of CNV in patients with AS or PXE.20-23 Studies have shown that ranibizumab, bevacizumab, and aflibercept are both safe and efficacious in the treatment of CNV, and in the reduction of sub-retinal fluid in patients with PXE and AS.20-23 Patients should be aware that multiple treatments are often necessary due to AS remaining throughout their lifetime. Treatment will be useful in minimizing reoccurrences in some patients.24Our patient underwent multiple intravitreal ranibizumab injections bilaterally resulting in presently quiescent CNVs. After vision rehabilitation this patient’s BCVAs are 20/40 OD and 20/100 OS with improved quality of life.
Referrals were made to dermatology, cardiology, and gastroenterology with correspondence and photographs; we suggested an appropriate work up. A 4mm punch biopsy of this patient’s dermis confirmed the diagnosis of PXE. The cardiology workup was remarkable for increased LDL cholesterol and simvastatin was prescribed. The gastrointestinal specialist elected to proceed with a colonoscopy, which was unremarkable. Given the risk for serious systemic conditions, the ophthalmic care physician is in a unique position to help address the global needs of PXE patients beyond the eyes. Patient education and interdisciplinary management with other professionals is critical to successful outcomes in these cases. Internal medicine, dermatology, retinal subspecialty, cardiology and gastroenterology are just a few of the professionals that will be involved in the long-term the management. Patients should monitor their vision as CNV can present even in the absence of trauma and timely consultation is crucial. Fortunately, anti-VEGF injections have shown promise in maximizing visual outcomes. With the proper care and management, patients with PXE have the potential for maintaining quality of life.
Dr. Gurwood thanks Brian Knight OD and Andrew Rixon OD, for contributing this case.
1. Chassaing N, Martin L, Calvas P, et al. Pseudoxanthoma elastic ABCC6 mutations. Journal of Medical Genetics 2005;42(12):881–892. 2. Finger RP, Charbel Issa P, Ladewig M, et al. Fundus autofluorescence in pseudoxanthoma elasticum. Retina. 2009; 29(10):1496-505. 3. Váradi A, Szabó Z, Pomozi V, et al. ABCC6 as a target in Pseudoxanthoma Elasticum. Current Drug Targets.2011; 12(5):671–682. 4.Georgalas I, Papaconstantinou D, Koutsandrea C, et al. Angioid streaks, clinical course, complications, and current therapeutic management. Ther Clin Risk Manag. 2009;5(1):81-9. 5. Agarwal A, Patel P, Adkins T, Gass JD. Spectrum of pattern dystrophy in pseudoxanthoma elasticum. Arch Ophthalmol. 2005; 123(9):923–928. 6. Laube S, Moss C. Pseudoxanthoma elasticum. Arch DisChild. 2005;90(7):754–756. 7. Uitto J, Li Q, Jiang Q. Pseudoxanthoma elasticum: molecular genetics and putative pathomechanisms. J Invest Dermatol. 2010;130(3):661–670. 8. Gal-Or O, Balaratnasingam C, Freund KB. Optical coherence tomography angiography findings of choroidal neovascularization in pseudoxanthoma elasticum. Int J Retina Vitreous. 2015;1:11. 9. Britten MJ: Unusual traumatic retinal haemorrhages associated with angioid streaks. Br J Ophthalmol. 1966;50(5):540-542. 10. Piro P, Scheraga D, Fine S. Angioid streaks: natural history and visual prognosis in: Fine SL, Owens SL, editors. Management of Retinal Vascular and Macular Disorders. Baltimore, MD: Williams and Wilkins; 1983:136–139. 11. Bowen JM, Sobey GJ, Burrows NP, et al. Ehlers-Danlos syndrome, classical type. Am J Med Genet C Semin Med Genet. 2017;175(1):27-39. 12. Indumathi CK, Dinaker C, Roshan R. Juvenile Paget’s disease. Indian Pediatr. 2009;46(4):354-6. 13. Bonanomi MT, Lavezzo MM. Sickle cell retinopathy: diagnosis and treatment. Arq Bras Oftalmol. 2013;76(5):320-7. 14. Gliem M, Zaeytijd JD, Finger RP, et al. An update on the ocular phenotype in patients with pseudoxanthoma elasticum. Front Genet. 2013;4:14. 15. Schoenberger, Scott D., and Anita Agarwal. Geographic Chorioretinal Atrophy in Pseudoxanthoma Elasticum. Am J Ophthalmol. 2013;156(4):715-23. 16. Yung M, Klufas MA, Sarraf D. Clinical applications of fundus autofluorescence in retinal disease. Int J Retina Vitreous. 2016;2:12. 17.Sepah YJ, Akhtar A, Sadiq MA, et al. Fundus autofluorescence imaging: Fundamentals and clinical relevance. Saudi J Ophthalmol. 2014;28(2):111-6. 18. Zweifel SA, Imamura Y, Freund KB, Spaide RF. Multimodal fundus imaging of pseudoxanthoma elasticum. Retina. 2011;31(3):482-491. 19. Hanhart J, Greifner H, Rozenman Y. Locating and characterizing angioid streaks with en face optical coherence tomography. Retin Cases Brief Rep. 2017;11(3):203-206. 20. FingerRP, Charbel Issa P, Hendig D,et al. Monthly ranibizumab for choroidal neovascularization secondary to angioid streaks in pseudoxanthoma elasticum: a one-year prospective study. Am J Ophthalmol. 2011;152(4):695–703. 21. El Matri L, Kort F, Bouraoui R, et al. Intravitreal bevacizumab for the treatment of choroidal neovascularization secondary to angioid streaks: one year of follow-up. Acta Ophthalmol. 2011;89(7):641–646. 22. Esen E, Sizmaz S, Demircan N. Intravitreal aflibercept for management of subfoveal choroidal neovascularization secondary to angioid streaks. Indian J Ophthalmol. 2015;63(7):616-618. 23. Sawa M, Gomi F, Tsujikawa M, et al. Long-term results of intravitreal bevacizumab injection for choroidal neovascularization secondary to angioid streaks." Am J Ophthalmol. 2009;148(4):584-90. 24. Zebardast N, Adelman RA. Intravitreal ranibizumab for treatment of choroidal neovascularization secondary to angioid streaks in pseudoxanthoma elasticum: five-year follow-up. Semin Ophthalmol. 2012;27(3-4):61-4. 25 Georgalas I, Tservakis I, Papaconstaninou D, et al. Pseudoxanthoma elasticum, ocular manifestations, complications and treatment. Clin Exp Optom. 2011;94(2):169–180. |

