 |
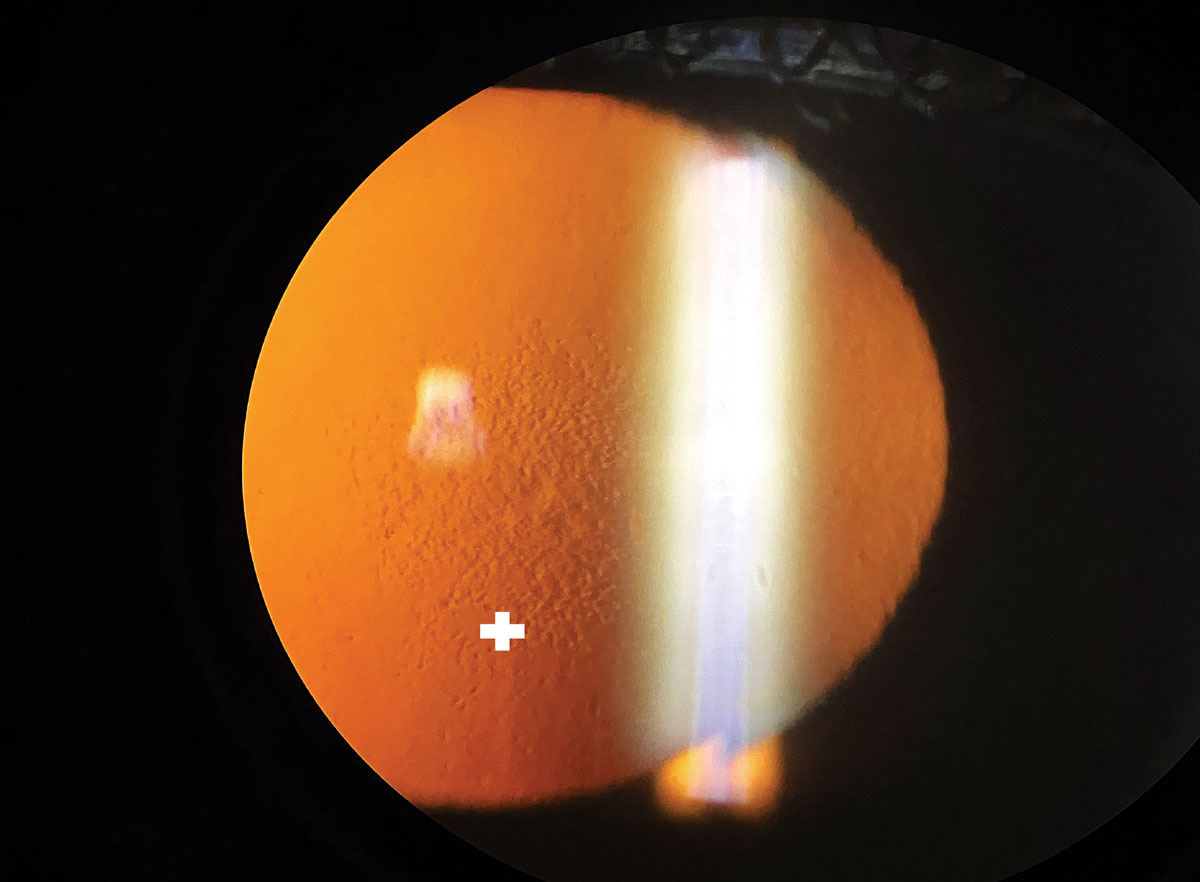
| Occasionally, donor corneas may be positive for corneal guttata; however, this study observed that most cases are mild and don't affect graft survival rate. Photo: Bhawan Minhas, OD. Click image to enlarge. |
Typically presenting as droplet-like changes in the posterior cornea, corneal guttata is an ocular pathology that destroys endothelial cells by causing accumulations and deposits of collagen and fibril fibers in Descemet’s membrane. The condition may progress and lead to endothelial cell loss or changes in size or shape and, in some cases, a reduction in corneal transparency, which then characterizes the patient’s condition as clinically manifested Fuchs’ endothelial corneal dystrophy (FECD).
The only way to treat FECD currently is with a corneal transplant, most commonly via Descemet membrane endothelial keratoplasty (DMEK). Despite taking precautions, occasionally, corneal guttata may be found in donor corneas after transplantation, which reduces the chance of graft survival. A recent study found that the rate of corneal guttata in patients post-DMEK was almost 20%, though only around 2% of cases were classified as clinically significant.
The retrospective study included 466 patients who underwent a total of 664 procedures (DMEK and triple-DMEK). Endothelial specular microscopy images were used to determine the postoperative prevalence and progression of corneal guttata, and severity grades were classified as either G0 (without corneal guttata) or G1-G3 with increasing severity of corneal guttata. The clinical parameters measured at an average of 19.6 months post-DMEK included central corneal thickness, visual acuity, endothelial cell density, pleomorphism and polymegethism.
Of the 18.8% of eyes with corneal guttata after transplantation, 16.9% were classified as G1, 1.4% as G2 and only 0.5% as G3. The researchers noted, “The examination of clinical parameters showed significant differences between healthy and low-grade corneal guttata (G0/G1) and high-grade corneal guttata (G2/G3).” They observed a significant deterioration in the corrected distance visual acuity as severity increased. Central corneal thickness values also increased between G0 (534µm) and G2 (549µm)/G3 (558µm). In addition, significant increases in pleomorphism and polymegethism were detected.
In terms of graft survival, no significant differences were detected between patients with corneal guttata and those without. Graft failure occurred in 4.8% of cases in eyes not affected by corneal guttata, while those affected had a graft failure rate of 5.3%.
The researchers pointed out, “Due to this small time frame between the date of the operation and corneal guttata detection, it can be assumed that corneal guttata may already have been present on the graft preoperatively.” They added that there’s also a possibility that “intraoperative endothelial stress and interactions with the new host environment might also be potential risk factors for endothelial damage and corneal guttata in the early postoperative course.”
The good news is that low-grade corneal guttata, which is characteristic of most affected patients, has almost no impact on the clinical outcomes of DMEK. Because patients with high-grade corneal guttata in this study had several significantly affected clinical parameters during follow-up, the researchers recommend closely monitoring patients post-DMEK for earlier detection of potential disease.
Schmitz LM, Safi T, Munteanu C, et al. Prevalence and severity of cornea guttata in the graft following Descemet membrane endothelial keratoplasty (DMEK). Acta Ophthalmol. June 2, 2022. [Epub ahead of print]. |

