 |  |
When treating patients with ocular trauma, we need to know how to triage appropriately, assess the situation, evaluate and treat the condition and refer if indicated. In cases of severe globe trauma, the majority will likely be seen in the emergency room or at the specialist’s office. Nonetheless, we should be prepared to assist.
Severe globe trauma occurs when the integrity of one or more membranes of the eye is disrupted by blunt or penetrating force. It requires represents one of the biggest challenges eye surgeons will face. Historically, severe globe trauma would often result in removal of the eye.
Significant surgical advancements have allowed us to save more eyes and reconstruct if necessary, but the concept of regaining any vision was not reasonable. Through the continued refinement of surgical techniques and remarkable efforts from retinal surgeons, we are able to witness surgeries like silicone vitrectomies.
Repairing a Rupture
The presented case is trauma is from a nail injury, which caused a posterior rupture. Initial evaluation showed very little chance that the eye could be saved, but an exploratory vitrectomy/lensectomy was attempted. Upon initial presentation, a proper assessment of the posterior pole was not possible due to excessive bleeding in the vitreous cavity. Once the vitreous hemorrhage was cleared, a reasonable amount of salvageable retina was discovered amongst overwhelming scar tissue.
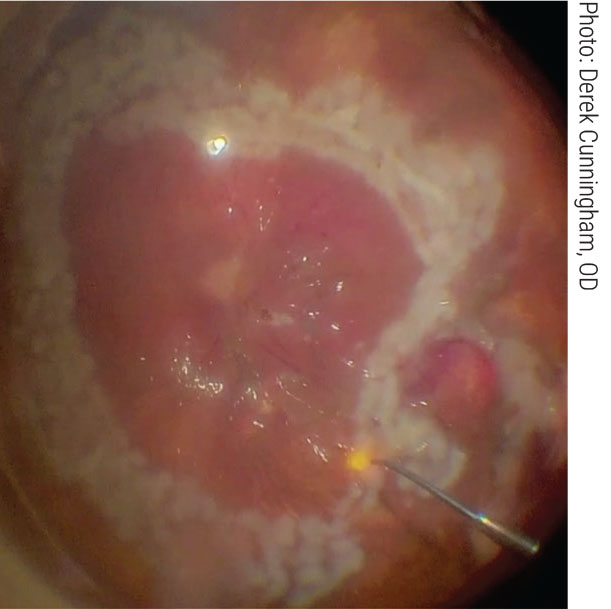 |
| Subretinal scar tissue is removed during a silicone vitrectomy. Click image to enlarge. |
In this procedure, a 360° retinectomy was performed to free up the retina so it was not tethered to one position for accessibility. The surgeon then attempted to atraumatically remove as much subretinal scar tissue as possible. The surgeon must keep a fine balance, as the more scar tissue that is removed, the greater the likelihood of choroidal hemorrhage. In this case, the surgeon was able to delaminate most of the subretinal scar tissue, greatly aiding in its removal.
The next step is to create a bubble with perfluorocarbon liquid that slowly and carefully increases the bubble size to flatten the retina. Once the retina is reasonably flat, a brush is used to manipulate the retinal tissue into position and also to try and remove remaining retinal folds. While this gentle flattening and smoothing is being done, more perfluorocarbon is added to the space. The surgeon must take exceptional care during manipulation of the retina with physical tools, as a retinal break or tear can easily happen at this stage.
Several rows of barricade laser are added around the periphery of the retina to keep it in place. An air fluid exchange is performed, and the vitreous cavity is filled with silicone oil, which acts as a reliable tamponade for the retina and is often used for complex retinal detachment surgeries.
In most cases, the oil will be removed at a later point to avoid long-term silicone oil–related complications such as glaucoma. There is a fine balance in how long to leave the oil in, though. The patient will not see as well, but it is thought that the longer the oil is left in the eye, the more you decrease risk of recurrent detachment.
Remember that even when the oil is removed, there are a significant amount of complications to watch for in addition to recurrent retinal detachment, such as emulsification, silicone oil in the anterior chamber, keratopathy, glaucoma, chronic hypotony, cataract, adherence of oil droplets to an intraocular lens, silicone oil invasion of the retina and optic nerve and unexplained visual loss following removal.
Due to the complexity of the case and potential complications, a patient like this should stay in close contact with both their optometrist and retina specialist for the remainder of their life.
This surgical case represents the extraordinary measures that can be taken to preserve a functional part of our patients’ vision. If you are ever presented with an open globe, shield the eye (but don’t patch it) to reduce the risk of any further trauma while the patient in transported to the hospital. Thankfully, these events don’t occur frequently, but we must keep trying and working with our retina colleagues to best address our patient’s vision and eye care needs.
Dr. Cunningham is the director of optometry at Dell Laser Consultants in Austin, TX. He has no financial interests to disclose.
Dr. Whitley is the director of professional relations and residency program supervisor at Virginia Eye Consultants in Norfolk, VA. He is a consultant for Alcon.

