Mention therapeutic lenses, and most of us immediately think of a soft lens. However, in certain cases gas permeable (GP) lenses can be used for therapeutic purposes, especially in cases of corneal irregularity.
Here, well look at specific situations in which GP lenses can help correct corneal irregularity.
Indications Special Considerations for Penetrating Keratoplasty, Keratoconus Patients Penetrating keratoplasty and keratoconus patients are among your most challenging contact lens fits. Here are some specific considerations for these patients. Penetrating Keratoplasty Keratoconus
An irregular corneal surface does not allow for optimum vision. Gas permeable lenses, however, trap the tears to fill in that irregularity. This can improve the level of vision beyond any spectacle correction. For this reason, we consider these lenses therapeutic.
Some examples of when we might use gas permeable lenses:
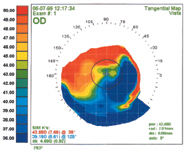
A steep-to-flat topography is one alteration of the cornea that can occur after penetrating keratoplasty. A reverse geometry lens was the best option for this patient.
Keratoconus. GP lenses are the mainstay for treating moderate and advanced keratoconus. With the many designs available today, a large proportion of the keratoconus patients can appreciate improved visual acuity.1 Some 65% of patients in the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) study wore GP lenses in both eyes.2
Penetrating injury. If an injury is superficial and confined to the epithelium, the tissue will usually heal, but if it goes through to the stroma or into the anterior chamber, scarring and irregularity may result. A gas permeable lens may then be necessary to maximize visual recovery.
Dystrophies and degenerations. Corneal dystrophies (map-dot-fingerprint, lattice degeneration, etc.) may result in irregularity and decreased visual function. If tolerable from a comfort standpoint, a gas permeable lens may improve visual function.
GP lenses are ideal for visual rehabilitation in patients with pellucid marginal degeneration, especially in patients whose condition is advanced. Surgical intervention, such as penetrating keratoplasty and thermokeratoplasty, is an option, especially when the vision or comfort with lenses is no longer acceptable, but surgery provides poor long-term reduction of astigmatism.3
Terriens marginal degeneration also can create distortion. Rigid lenses may optimize the vision for those patients.
Post-PK patients. Optical indications for GP lenses following penetrating keratoplasty include irregular astigmatism, spherical and/or astigmatic anisometropia or a combination of these.4
Consider several lens designs. Some fitters empirically start with a large diameter flat design (either a standard design or a proprietary post-PK design). You might start with a toric design if the patient has significant astigmatism or consider a reverse geometry design for an oblate cornea. Other lens designs to consider: aspheric, biaspheric and bitoric lenses.
Larger diameter lenses are usually more successful than smaller ones. You want to vault the center area and have the contact lens rest on the more peripheral portion of the cornea.
Comfort and biomicroscopy must both be acceptable. The patient should be able to wear the lens for as many hours as desired (or as close to this as possible), and the lens needs to stay in the eye. If you observe corneal changes as the patient increases wearing time, modifications or a refit may be necessary.
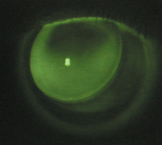
Fluorescein analysis is imperative. Because of all the hills and valleys that can occur, do not expect to observe a normal fluorescein pattern. Try to distribute the weight bearing forces evenly and look for corneal changes such as superficial punctate keratitis, early neovascularization or edema. If you observe changes, continue the fitting process.
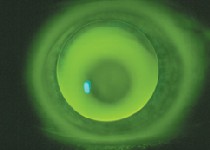
An apical touch fluorescein pattern provides better endpoint acuity than if you completely vault the cone. Courtesy: Timothy B. Edrington, O.D.; CLEK Study Group
Beware of sutures. If sutures remain, on occasion, one may break. The patient will experience foreign-body sensation. The suture must be removed and the patient placed on an antibiotic until the cornea heals. Youll need to reassess the contact lens fit, because removal of broken sutures often changes the shape of the cornea.
Be aware of the signs and symptoms of graft rejection. These include a decrease in vision, pain and redness. Patients may associate these with their lenses. Instruct them to return immediately if symptoms do not improve within hours of lens removal.
Consider the shape of the cone. Is it a nipple cone or an oval sagging cone? Remember that lenses tend to center at the steepest part of the cornea. Because nipple cones usually occur somewhat centrally, most keratoconic designs have a good chance of success. For patients with lower sagging cones, you may need to find a design that is larger in diameter and optic zone. The lens will center over the steepest part of the cornea, which is in that low area. If the patient is not looking out of the optic zone, he or she will not experience good vision.
Go for the light touch. Look for the base curve/optic zone to house the cone. Most GP lens wearers in the CLEK study (88%) were fitted with apical touch.2 A light touch over the cone provides the patient with a better endpoint acuity than if you completely vault the cone. So when Im fitting keratoconus patients, this, to me, is the ideal fluorescein pattern. Also, strive for alignment as best you can in the peripheral portion.
Beware of scarring. If the patient has scarred corneas, I choose a larger diameter lens and try to vault the scarred area.S.I.C.
Excessive postoperative astigmatism is usually the biggest visual complication of corneal transplant surgery. The amount of astigmatism present depends on the surgeons technique, how the host and the graft oppose, plus the patients healing factors. One study found that best-corrected visual acuity improved from less than 20/40 with spectacles alone to better than 20/30 with a GP lens.4
Unsuccessful LASIK. Contact lenses are valuable for helping improve poor acuity that results from unsuccessful LASIK. One study found that patients fit with spectacles achieved a mean acuity of 20/30, while those who were fit with contact lenses had a mean acuity of 20/20.5
GP lenses can also help patients who have post-LASIK ectasia and may, at times, be the only alternative for patients with induced irregular astigmatism. Indeed, in the latter group, GP lenses provided the best visual performance and patient tolerance, according to one study.6,7
Moderate Choices
When fitting patients with irregular corneas, I usually prefer a material with a moderate amount of oxygen permeability. Higher Dk materials are ideal for corneas that need as much oxygen as possible (such as those of a diabetic patient) and for those occasional circumstances that necessitate overnight lens wear.
Even though more oxygen passes to the cornea, with higher Dk materials, the irregular corneal surface and the blinking forces of the lids may cause the higher Dk to flex. A lower Dk material, however, resists flexure and offers better acuity.
My initial choice of lens material depends on the patients needs and Rx. For example, if the patient requires -3.00D of correction, the edges wont be as thick, so Im willing to start with a lower DK material. If the patient requires a -5.00D or hyperopic correction, Im more likely to start with a material that offers more oxygen transmission in those thicker areas.
Even Distribution
While there are many special fitting considerations for each disorder, there are some general guidelines.
Youll want to distribute the weight-bearing forces of the contact lens as evenly as possible over the entire cornea. You dont want any heavy areas of bearing or excessive clearance.
Corneal topography is a great asset for fitting. Assess the entire topography of the cornea, then choose your lens design according to the shape factor. Use fluorescein analysis to assess the fit and guide any lens design changes that may be necessary.
Remember, a contact lens will center over the steepest part of the cornea. With some unusual shape patterns, a patient may wind up with a decentered lens that extends onto the sclera or has significant edge lift inferiorly adjacent to the steeper side. For these patients, you may need to rely on lid interaction to stabilize the lens. Youll also need to increase the diameter of the lens and the optic zone. (Dont forget to flatten the base curve to maintain the same saggital depth.) Sometimes a biaspheric design may be the best option.
As with any GP fit, youll go through the troubleshooting process. Expect to observe areas that are flatter or steeper and adjust the lens parameters accordingly. Remember that youre not dealing with a normal-shaped cornea, so you wont get a normal-shaped fluorescein pattern.
Dr. Cutler, a contact lens consultant, is in private practice in Wyndmoor and Blue Bell, Pa. She is an adjunct faculty member at Pennsylvania College of Optometry.
1. Lim N, Vogt U. Characteristics and functional outcomes of 130 patients with keratoconus attending a specialist contact lens clinic. Eye 2002 Jan;16(1):54-9.
2. Szczotka LB, Barr JT, Zadnik K. A summary of the findings from the Collaborative Longitudinal Evaluation of Keratoconus (CLEK) Study. CLEK Study Group. Optometry 2001 Sep;72(9):574-84.
3. Biswas S, Brahma A, Tromans C, Ridgway A. Management of pellucid marginal corneal degeneration. Eye 2000 Aug;14(Pt 4):629-34.
4. Wietharn BE, Driebe WT Jr. Fitting contact lenses for visual rehabilitation after penetrating keratoplasty. Eye Contact Lens 2004 Jan;30(1):31-3.
5. Hau SC, Ehrlich DP. Contact lens fitting following unsuccessful refractive surgery. Ophthalmic Physiol Opt. 2003 Jul;23(4):329-40.
6. Randleman JB, Russell B, Ward MA, et al. Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology 2003 Feb;110(2):267-75.
7. Alio JL, Belda JI, Artola A, et al. Contact lens fitting to correct irregular astigmatism after corneal refractive surgery. J Cataract Refract Surg 2002 Oct;28(10):1750-7.

