 |
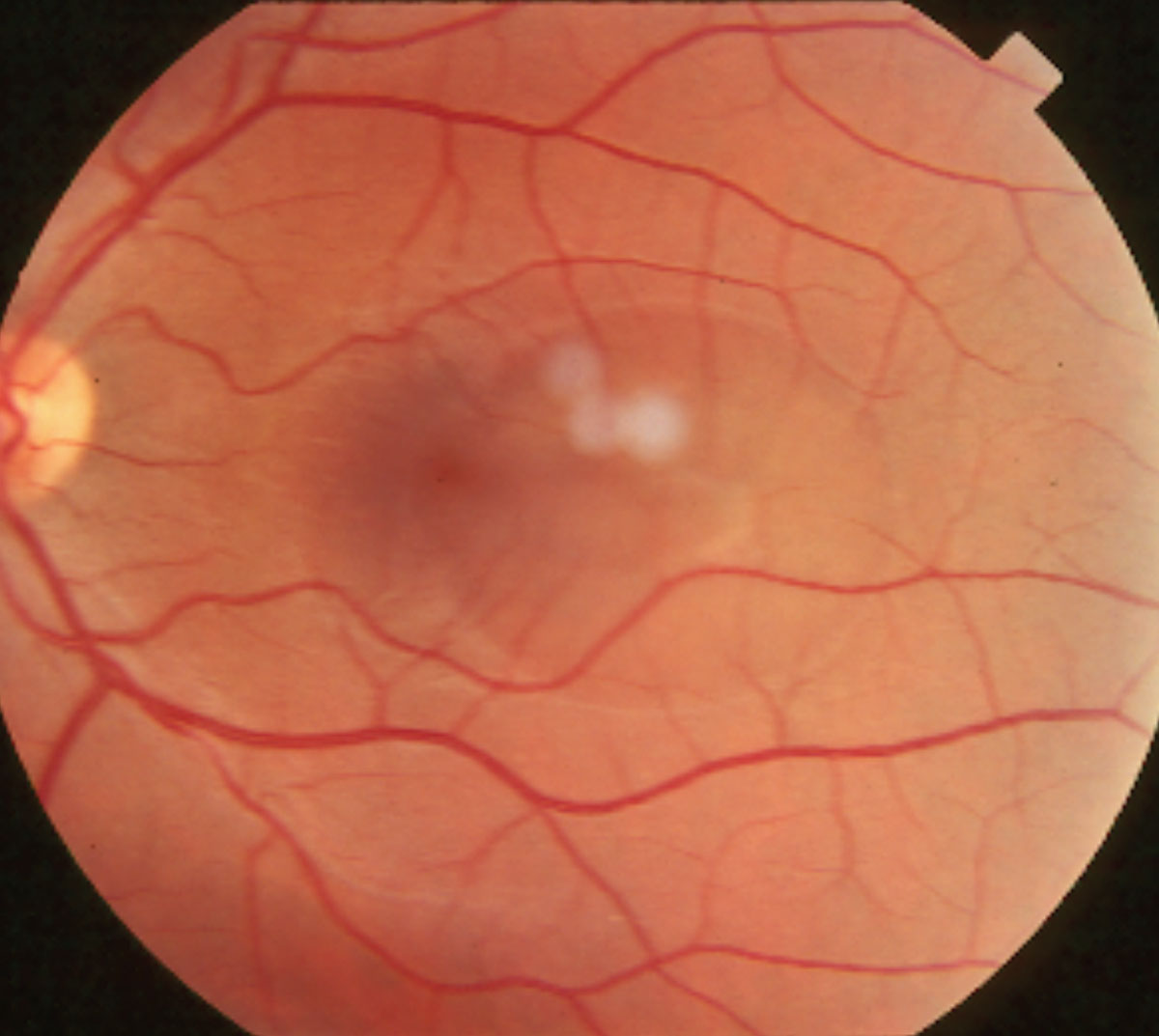
| Researchers determined that RPE damage may occur from both acute and chronic cases of CSC. Photo: Joseph W. Sowka, OD. Click image to enlarge. |
Central serous chorioretinopathy (CSC) usually occurs in young and middle-aged people. Its pathogenesis is related to the increase of choroidal vascular permeability. The gold standard for diagnosing CSC is fundus fluorescein angiography and indocyanine green angiography. However, as authors of a recent study pointed out, these methods are invasive and that may limit their clinical application. “OCT as a noninvasive examination, can accurately reflect the size and extent of the serous neurosensory detachment and pigment epithelium detachment, which can effectively help diagnose CSC,” they wrote.
The researchers studied the imaging characteristics of acute and chronic CSC on OCT to identify differences between the two and aid differential diagnoses. They examined 62 eyes of 56 patients with CSC (41 [73.21%] male) and observed image features on OCT. They measured photoreceptor outer segment (PROS) thickness above the pigment epithelium detachment (PED) coinciding with the leakage point on fundus fluorescein angiography and compared this with the mean PROS thickness outside the PED in acute cases.
They reported a total of 53 (85.48%) eyes with acute CSC and nine (14.52%) with chronic CSC. A new feature was noted in the macular detachment area: a high reflection band in the outer nuclear layer. Mean PROS thickness above the RPE layer protuberance coinciding with the leakage point was 22.7µm in acute cases, which the authors noted in the study was less than the mean PROS thickness outside the PED at 64.3µm.
They found that in two acute CSC cases, the high reflection bands were absent when the serous retinal detachment was not in the macular area. “This phenomenon was the same as in chronic CSC,” the authors wrote. “Therefore, no bands were visible when the serous retinal detachment wasn’t in the macular area.”
“It is our opinion that the highly reflective bands may be due to retinal ischemia, which develops after retinal detachment, resulting in edema in the outer nuclear layer similar to what occurs in paracentral acute middle maculopathy,” the authors wrote in their paper. “But if that’s true, it’s unclear what the reason for the absence of ischemia in the periphery of the detached area is. Perhaps the reason the band is not visible outside the macula is due to technical and optical aspects of the OCT scan going beyond the macula area.”
“Acute and chronic CSC were significantly different, although both presented with serous retinal neuroepithelial detachment and one or more lesions,” the authors continued. “In patients with acute CSC, the serous retinal detachment was mainly confined to the macular area, and the degree of detachment was significantly elevated. Patients with chronic CSC, on the other hand, had significantly shallower detachment heights and more extensive detachment than those with acute CSC that was not limited to the macular area but also extended beyond it or was multifocal.”
Additionally, both acute and chronic CSC cases showed RPE damage. Focal RPE layer protuberance was seen in acute cases within the serous retinal detachment. The authors described this as “not a typically arch-shaped pigment epithelium detachment” with the RPE intact in other areas. With OCT the researchers found that the position of the RPE layer protuberance was consistent with the location of the leakage point on fundus FA. “Therefore, we considered that the RPE protuberance found using OCT represents the position of the decompensated RPE, or in other words, the leakage point.” A total of 44 of 53 eyes with acute CSC had this feature.
They also reported extensive and large RPE damage in chronic CSC cases, including loss, proliferation or break. “The serous retinal detachment fluid moves with gravity, and when it’s not absorbed for a long time, it can also form a retinal pigment epithelium descending tract,” they noted. “Even when the fluid is finally absorbed, it will still leave a retinal pigment epithelium atrophy band, resulting in decreased visual acuity.”
Other findings included hyperreflective bright spots in the outer retina within the serous neurosensory detachment in both acute and chronic cases and fibrin exudation due to increased choroid permeability (this latter finding was less dense in acute CSC than in chronic CSC).
The authors concluded that OCT is a good, noninvasive technique for aiding clinicians in the differentiation of retinal, retinal pigment epithelium and choroidal lesions in patients with acute or chronic CSC, as well as an alternative to invasive fundus FA. They say these characteristics can also help with disease progression monitoring.
Li Y, Jin P, Lu J, et al. Analysis of optical coherence tomography in acute vs. chronic central serous chorioretinopathy. Optom Vis Sci. December 10, 2021. [Epub ahead of print]. |

