Currently, 35.7% of all adults living in the US are obese.2 When adjusting for demographic variations, the highest obesity rates are observed in non-Hispanic black women (58.5%) and the lowest rates are observed in non-Hispanic white women (32.2%).3
 In 2012, no state had an obesity incidence lower than 20%, as measured by body mass index (BMI).1 Further, 13 states had an obesity incidence equal to or greater than 30%.4 To put these figures into context––just 30 years ago, the highest incidence of adult obesity documented in any state’s population was still lower than that recorded in the least obese state’s population today.5
In 2012, no state had an obesity incidence lower than 20%, as measured by body mass index (BMI).1 Further, 13 states had an obesity incidence equal to or greater than 30%.4 To put these figures into context––just 30 years ago, the highest incidence of adult obesity documented in any state’s population was still lower than that recorded in the least obese state’s population today.5
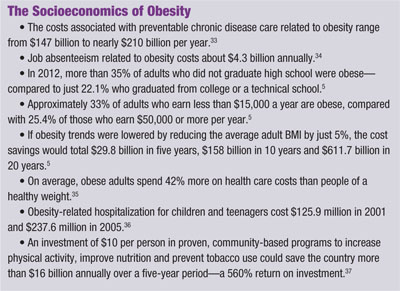
Suffice it to say that contemporary obesity rates in America simply aren’t sustainable––either financially or medically.
There is a bit of good news, however. In August 2013, the CDC announced that in 18 states, obesity rates decreased among preschool children from low-income families when compared to 2012 figures.4 Several states also have independently reported progress in reducing childhood obesity using a multifaceted approach of education, school lunch improvements and increased physical activity levels.5
It is also worth noting that since 2005, adult obesity rates have increased more slowly than they did during the two decades prior. In fact, from 2012 to 2013, only one state’s obesity level increased (Arkansas), while all others remained unchanged.5 So, it seems that comprehensive efforts aimed at curtailing obesity-related disease appear to be taking hold––albeit slowly.
But unless your patient base is overwhelmingly healthy, active, fit and young, chances are that obesity rates in your practice mirror those seen in the general US population. Be honest––how often do you discuss weight-related health complications with your patients? If you’re like most optometrists, it probably isn’t a standard component of your management plan. This approach must change, however, if we are ever going to have a reasonable chance of halting the obesity epidemic.
Obesity’s Impact on the Eye and Body
During the last three decades, we’ve seen a proportionate increase in the incidence of obesity and potentially life-threatening systemic conditions, such as hypertension, carotid artery disease, coronary heart disease and stroke, type 2 diabetes, sleep apnea and certain forms of cancer.5 The association between excess body weight and the aforementioned systemic diseases is well established.
 However, until only recently, the vast majority of care providers have not included excess body weight as a primary risk factor in the pathogenesis of several visually devastating ocular conditions. The American Optometric Association Practice Guidelines for Comprehensive Adult Eye and Vision Examination consider patients with diabetes and/or hypertension to be among those “at risk” for significant ocular complications. These patients should undergo a comprehensive evaluation annually, compared to every two years for healthy individuals.2
However, until only recently, the vast majority of care providers have not included excess body weight as a primary risk factor in the pathogenesis of several visually devastating ocular conditions. The American Optometric Association Practice Guidelines for Comprehensive Adult Eye and Vision Examination consider patients with diabetes and/or hypertension to be among those “at risk” for significant ocular complications. These patients should undergo a comprehensive evaluation annually, compared to every two years for healthy individuals.2
Here’s a brief overview of several obesity-related conditions that yield both systemic and ocular complications:
• Hypertension. More than 75% of hypertension cases can be causally linked to obesity.6 Hypertension frequently is associated with cardiovascular disease, heart failure, ischemic stroke, intracerebral hemorrhage and chronic kidney disease—primary contributors to morbidity and mortality in US adults.7
The American Heart Association’s guidelines include a “caution” or “pre-hypertension” category, which is defined as a systolic blood pressure between 120mm Hg and 139mm Hg and/or diastolic pressure between 80mm Hg and 89mm Hg.8 In recent years, patients in this category are more likely to be placed on antihypertensive therapy rather than instructed to modify their diets and increase exercise levels.9
Fortunately, the AHA offers an interactive tool on its website (www.heart.org) that educates patients about the various ways they can reduce their blood pressure via lifestyle modification. Patients can use the program to estimate how much lower their blood pressure would be if they lost five, 10 or even 20 pounds.
The most common ocular manifestations of hypertension include hypertensive retinopathy, retinal vascular occlusions, cranial nerve palsies and optic neuropathy.10-12 Frequently, patients present with mild hypertensive retinopathy, which is characterized by arteriolar narrowing/constriction, arteriovenous nicking, or other vascular changes that are most evident at the locations of arteriole and venule crossing.13,14
Typical optometric management includes documentation in the patient’s chart, proper education about the condition, and a recommendation to adhere to their primary care provider’s prescribed treatment. In most cases, patients who exhibit these retinal findings also are overweight or obese. Therefore, to reduce the incidence of further disease progression, weight loss strategies must be addressed in the patient’s comprehensive management plan.
• Diabetes. In the early 1990s, approximately 7.8 million Americans had an active diagnosis of diabetes. Today, that figure is approximately 25.8 million.5 Nearly 40% of US adults currently are diabetic or pre-diabetic, and most of them don’t even know it.5
Worse yet, by 2020, it is estimated that this figure will climb to 50%, yielding an enormous increase in health care spending to provide care for these patients.15 So, early intervention for at-risk patients is essential.
There are clear optometric practice guidelines for the management of diabetic retinopathy, the most common retinal vascular cause of vision loss.16 Clearly, overweight or obese individuals have a much greater likelihood of developing type 2 diabetes.
So, be sure to refer these patients to their primary care provider for evaluation if a year or more has passed since their last physical examination. Also, be especially diligent when examining obese patients for early signs of diabetic eye disease.
• Other common conditions. Approximately one-third of all cancer deaths are linked to either obesity or a lack of physical activity.17 And while these cancers aren’t always detected as primary ocular tumors, it is still important to inform patients that being overweight or obese can increase their risk for several types of cancer.
Sleep apnea is strongly associated with obesity, especially when the diagnosis is made via measurement of waist and neck circumference.18,19 Sleep apnea can contribute to several ocular conditions, including glaucoma and keratoconus.
Continuous Positive Airway Pressure (CPAP) is the mainstay of therapy for patients with sleep apnea; however, weight reduction is far more effective at preventing long-term systemic and ocular complications.18
Obesity is now recognized as an independent risk factor for age-related macular degeneration.20,21 Dietary modification can be highly protective against the development and progression of early AMD. At-risk patients should be encouraged to increase their daily intake of leafy greens and brightly colored vegetables (e.g., orange peppers), which are rich in lutein and zeaxanthin.
Additionally, obese patients should be encouraged to lose excess weight through increased physical activity and low-glycemic diets to further protect against AMD. Just keep in mind that nutritional supplementation alone, without comprehensive dietary modification, will not provide optimal protection against macular degeneration.20,21
The Psychosocial Impact of Obesity
In America, thinner people frequently stigmatize overweight people. It occurs on television shows, in magazine articles and in day-to-day life. Teachers, college admissions counselors, employers, nutritionists, and even doctors and nurses may ascribe negative attributes to obese people based solely upon their weight.22-26 Associated stereotypes are prevalent, and overweight and obese individuals often are characterized as lazy, unsuccessful, undisciplined and willless.27
The misguided perception that shaming obese people could perhaps motivate them to lose weight secondary to guilt is unsupported. To the contrary, research suggests that such callous regard for overweight individuals poses serious health risks, creates social anxiety, and interferes with more effective efforts to reduce or prevent obesity.28 Youths who are teased about their weight are more likely to engage in variety of unhealthy behaviors, including binge eating, anorexia or purging.29,30
To date, wide-scale public health efforts have been largely successful in curtailing escalating obesity rates in America. Both lay people and health care professionals alike still believe that the condition of obesity is an issue of personal control.27
And while dietary choices and lifestyle habits certainly are a primary cause of obesity, the complex and intricate genetic, endocrine, psychological and behavioral drivers for food intake and energy regulation are not completely understood.
Much like patients with an opioid dependency, many people who struggle with obesity exhibit an uncontrollable attraction to food.31,32 In both instances of addiction, the same areas of the brain are stimulated by similar chemical substances.31,32 Thus, the prevalent belief that overeating is entirely the result of reduced willpower is unsubstantiated. This erroneous generalization impairs obesity intervention efforts and reduces access to quality care, which can create additional psychological stress on the patient.27
Connect With Your Patients
Specific, practical and interactive resources are essential when discussing the relationship between obesity and health complications with your patients. Conduct a comprehensive search in your practice area for registered dieticians or other reputable nutrition and wellness coaches. You may find that your community––on a local, county or state level––already has obesity-counseling resources in place.
For example, community centers often offer cooking instruction and exercise classes for those interested in weight loss. Also, walking clubs frequently can be found at indoor shopping malls.
Further, a number of excellent websites are available to provide useful tools and other information regarding healthy weight control strategies, nutritional guidelines and diabetes management. Some of the most helpful sites include:
• www.Heart.org/HEARTORG/Conditions/HighBloodPressure
• www.cdc.gov/healthyweight/index.html
• www.diabetes.org
Obesity Management for Kids and Teens
Considering all of the factors involved, children and teenagers currently are in the best position to slow or even reverse the escalating obesity rate in America. As primary health care providers, optometrists can contribute to these efforts using a sensitive, supportive approach with overweight and obese pediatric patients and their parents.
Several resources are available to help calculate pediatric BMIs (up to age 19)––including the CDC’s calculation tool, www.cdc.gov/healthyweight/children. Additionally, this website offers an excellent, printable resource for parents to help their children reach and maintain a healthy weight. Similar information is presented at www.patient.co.uk/health/obesity-and-overweight-in-children, along with a variety of interactive resources from the UK.
Affiliated with the Let’s Move initiative, www.healthykidshealthyfuture.org offers free online training, presentations and interactive quizzes for children, parents and health care providers. These materials are designed to emphasize the fundamental importance of healthier lifestyle decisions starting in infancy.
Another useful assessment tool for parents can be found at www.webcalcsolutions.com/Parenting-Assessments/child-obesity-risk. Here, visitors can find a simple, eight-question quiz that’s designed to help determine a child’s risk of becoming overweight.
Many of the aforementioned websites offer printable brochures and wall charts designed for pediatric education and often include literature on associated lifestyle considerations, such as proper hydration, tobacco avoidance, exercise routines and good sleep habits.
Historically, optometrists largely have been passive observers in the fight against obesity-related disease. Going forward, however, it is imperative that we educate ourselves about the potential ocular and systemic ramifications of obesity, as well as develop the skills necessary to help create effective, individualized management plans for our patients. But, in order to do so, we must first disengage from the outdated notion that weight management is not within our scope of care.
Dr. Reed is an associate professor at Nova Southeastern University College of Optometry in Fort Lauderdale, Fla., where she teaches ocular disease, ocular pharmacology and nutrition, and primary clinical care.
1. Fryar CD, Carroll MD, Ogden CL. National Center for Health Statistics. Prevalence of Overweight, Obesity, and Extreme Obesity Among Adults: United States, Trends 1960-1962 through 2009-2010. Available at: www.cdc.gov/nchs/data/hestat/obesity_adult_09_10/obesity_adult_09_10.htm. Accessed February 21, 2014.
2. Casser L, Carmiencke K, Goss D, et al. Optometric Clinical Practice Guideline: Comprehensive Adult Eye and Vision Examination, 2nd ed. St. Louis: American Optometric Association; 2005.
3. Flegal KM, Carroll MD, Kit BK, Ogden CL. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999-2000. JAMA. 2012 Feb 1;307(5):491-7.
4. The US Centers for Disease Control and Prevention. Adult Obesity Facts. Available at: www.cdc.gov/obesity/data/adult.html. Accessed February 21, 2014.
5. Levi J, Segal L, Thomas K, et al. Robert Wood Johnson Foundation. F as in Fat 2013: How Obesity Threatens America’s Future. Available at: www.rwjf.org/content/dam/farm/reports/reports/2013/rwjf407528. Accessed February 21, 2014.
6. The Obesity Society. Health Effects of Obesity. Available at: www.obesity.org. Accessed February 21, 2014.
7. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003 May 21;289(19):2560-72.
8. American Heart Association. About high blood pressure. Available at: www.heart.org/HEARTORG/Conditions/HighBloodPressure/AboutHighBloodPressure/About-High-Blood-Pressure_UCM_002050_Article.jsp. Accessed February 21, 2014.
9. Kaplan NM. Systemic hypertension: Treatment. In: Bonow RO, Mann DL, Zipes DP, et al (eds.). Braunwald’s Heart Disease: A Textbook of Cardiovascular Medicine, 9th ed. Philadelphia: Saunders Elsevier; 2011.
10. Chapin J, Carlson K, Christos PJ, Desancho MT. Risk factors and treatment strategies in patients with retinal vascular occlusions. Clin Appl Thromb Hemost. 2013 Dec 11.
11. Tamhankar MA. Biousse V, Ying GS, et al. Isolated third, fourth, and sixth cranial nerve palsies from presumed microvascular versus other causes: a prospective study. Ophthalmol 2013 Nov;120(11):2264-9.
12. Mohsenin A, Mohsenin V, Adelman RA. Retinal vascular tortuosity in obstructive sleep apnea. Clin Ophthalmol. 2013;7:787-92.
13. Henderson AD, Bruce BB, Newman NJ, Biousse V. Hypertension-related eye abnormalities and the risk of stroke. Rev Neurol Dis. 2011;8(1-2):1-9.
14. Cheung CY, Ikram MK, Sabanayagam C, Wong TY. Retinal microvasculature as a model to study the manifestations of hypertension. Hypertension. 2012 Nov;60(5):1094-103.
15. Wang YC, McPherson K, Marsh T, et al. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet. 2011 Aug 27;378(9793):815-25.
16. Cavallerano J. Optometric Clinical Practice Guidelines: Care of the patient with diabetes mellitus. St. Louis: American Optometric Association; 2009.
17. American Cancer Society. Cancer Facts and Figures, 2012. Available at: www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-031941.pdf. Accessed February 21, 2014.
18. Lee Ck, Tefera E, Colice G. The effect of obesity on outcomes in mechanically ventilated patients in a medical intensive care unit. Respiration. Respiration. 2014 Jan 23. [Epub ahead of print]
19. Mazzuca E, Battaglia S, Marrone O, et al. Gender-specific anthropometric markers of adiposity, metabolic syndrome and visceral adiposity index (VAI) in patients with obstructive sleep apnea. J Sleep Res 2014 Feb;23(1):13-21.
20. Munch IC, Linneberg A, Larsen M. Precursors of age-related macular degeneration: association with physical activity, obesity, and serum lipids in the Inter99 eye study. Invest Ophthalmol Vis Sci 2013 Jun;54(6):3932-40.
21. Chakravarthy U, Wong TY, Fletcher A, et al. Clinical risk factors for age-related macular degeneration: a systematic review and meta-analysis. BMC Ophthalmol. 2010 Dec 13;10:31
22. Sikorski C, Luppa M, Brahler E, et al. Obese children, adults and senior citizens in the eyes of the general public: results of a respresentative study on stigma and causation of obesity. PLoS One. 2012;7(10):e46924.
23. Sikorski C, Luppa M, Kaiser M, et al. The stigma of obesity in the general public and its implications for public health – a systematic review. BMC Public Health. 2011 Aug 23;11:661.
24. Swift JA, Tischler V, Markham S, et al. Are anti-stigma films a useful strategy for reducing weight bias among trainee healthcare professionals? Results of a pilot randomized control trial. Obes Facts. 2013;6(1):91-102.
25. Puhl R, Wharton C, Heuer C. Weight bias among dietetics students: implications for treatment practices. J Am Diet Assoc. 2009 Mar;109(3):438-44
26. Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009 May;17(5)941-64.
27. Puhl RM, Heuer CA. Obesity stigma: Important considerations for public health. Am J Public Health. 2010 Jun;100(6):1019-28.
28. Annis NM, Cash TF, Hrabosky JK. Body image and psychosocial differences among stable average weight, currently overweight, and formerly overweight women: the role of stigmatizing experiences. Body Image. 2004 May;1(2):155-67.
29. Neumark-Sztainer D, Falkner N, Story M, et al. Weight-teasing among adolescents correlations with weight status and disordered eating behaviors. Int J Obes Relat Metab Disord. 2002 Jan;26(1):123-31.
30. Libbey HP, Story MT, Neumark-Sztainer DR, et al. Teasing, disordered eating behaviors, and psychological morbidities among overweight adolescents. Obesity (Silver Spring). 2008 Nov;16 Suppl 2:S24-9.
31. Rui L. Brain regulation of energy balance and body weight. Rev Endocr Metab Disord. 2013 Dec;14(4):387-407.
32. Egecioglu E, Skibicka KP, Hansson C, et al. Hedonic and incentive signals for body weight control. Rev Endocr Metab Disord. 2011 Sep;12(3):141-51.
33. Cawley J, Meyerhoefer C. The medical care costs of obesity: An instrumental variables approach. J Health Econ. 2012 Jan;31(1):219-30.
34. Cawley, J, Rizzo JZ, Haas K. Occupation-specific absenteeism costs associated with obesity and morbid obesity. J Occup Environ Med. 2007 Dec;49(12):1317-24
35. Finkelstein EA, Trogdon JG, Cohen JW, et al. Annual medical spending attributable to obesity: Payer-and service-specific estimates. Health Aff (Millwood). 2009 Sep-Oct;28(5):w822-31.
36. Trasande L, Liu Y, Fryer G, et al. Effects of Childhood Obesity On Hospital Care and Costs, 1999-2005. Health Aff (Millwood). 2009 Jul-Aug;28(4):w751-60.
37. Trust for America’s Health. Prevention for a Healthier America; Investments in Disease Prevention Yield Significant Savings, Stronger Communities, 2008. Available at: http://healthyamericans.org/reports/prevention08. Accessed January 25, 2014.

