In the past few years, we Americans have increased our intake of vitamins and minerals to enhance our health. For instance, more than 50% of elderly persons currently use some form of dietary supplement.1 Sales of supplements in the United States topped $20.3 billion in 2004 (an increase of nearly 13% since 2001).2 National Institutes of Health funding for dietary supplement research topped $117 million in 2002, with over 350 research projects currently under way.
An impressive body of research clearly shows nutritional support can affect the development of eye conditions and that elderly persons have different metabolic needs that must be met by using nutritional supplements. Research on prevention and treatment of chronic degenerative diseases of agingsuch as cataract, macular degeneration, glaucoma and dry eyeis constantly growing. The beneficial effect of nutrition on these conditions is strongly supported by peer-reviewed research.
The Research
The term nutraceutical was coined in 1989 by Stephen DeFelice, M.D., who defined a nutraceutical as any substance that may be considered a food or part of a food and provides medical or health benefits, including the prevention and treatment of disease.3 Yet the term nutraceutical, as commonly used in marketing, has no regulatory definition.
With the 2001 publication of the Age-Related Eye Disease Study (AREDS), doctors began looking for more scientific information on the benefits of nutritional therapy.4 In 2002, the American Medical Association reversed its long-held position that multivitamins and dietary supplements were not necessary for persons consuming a proper diet. The AMA now recommends that all adults take multivitamins daily because studies have shown that the diets of most Americans are inadequate. It seems that the medical profession now recognizes that very few people actually get enough antioxidants and essential nutrients in their diet.5
Micronutrients and Eye Health
Here are some of the nutrients involved with eye health and disease control:
Retinol. Retinol (pre-formed vitamin A) is essential for wound healing and proper immune function. Retinol binds to the protein opsin in the rod cells to form the visual pigment rhodopsin (visual purple). Vitamin A in the form of retinol also plays an central role in the development of the mucins of the tear film.
The B vitamins. The coenzyme activity of the B-complex vitamins is required for optimal metabolism of all foods. Furthermore, research strongly suggests that supplementation with vitamins B6, B12 and folate can help keep homocysteine levels within the normal range. Recent research suggests a strong relationship between elevated plasma homocysteine levels and exudative neovascular AMD.6,7
Excessive supplementation with individual B vitamins can mask systemic deficiencies of other B vitamins. So, instruct patients to take a full complement of B-complex at the same time.
Lutein and zeaxanthin. More than a dozen carotenoids have been found in the blood, but only two specific xanthophyll carotenoidslutein and zeaxanthinaccumulate in the fovea. The naturally dark golden-yellow pigments of these carotenoids filter out potentially phototoxic blue light and near-ultraviolet radiation from the macula. The generally accepted functions of these two dietary xanthophylls are to provide pigment to the macula and to foster antioxidant activity (along with other job-specific antioxidants) to protect the eye against singlet oxygen and peroxyl radicals.8-10
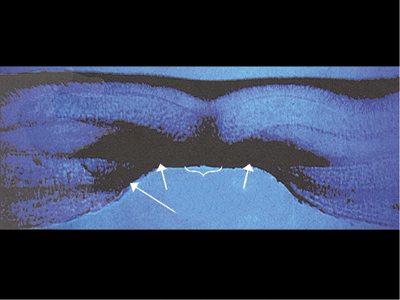
While many articles have stressed the importance of lutein in macula function, recently published and ongoing research suggests that zeaxanthin is the predominant pigment in the central fovea.11 The fovea selectively places zeaxanthin in its very center, where the greatest protection from blue light radiation is needed. Because zeaxanthin contains 11 double bonds, versus the 10 double bonds in lutein, it offers more powerful antioxidant protection than does lutein against phototoxic damage caused by blue and near-ultraviolet light radiation.11
Researchers now believe that it is more likely that the macular pigment is entirely of dietary origin, and a recent study suggests that both healthy and diseased maculae can accumulate and stabilize both lutein and zeaxanthin.12 This is of particular interest to patients diagnosed with AMD, as well as to those who supplement their diets with these carotenoids to help prevent macular degeneration.13
Lutein and zeaxanthin are found in many of the brightly colored fruits and vegetables. Recent research estimates an approximate ratio of 5:1 for lutein compared to zeaxanthin intake in the typical U.S. diet, primarily because lutein is found in much higher amounts than zeaxanthin in most fruits and vegetables.14
 |
|
Research suggests the zeaxanthin pigment in the central macula spreads outward to the periphery of the macula and to the other parts of the retina. |
Zeaxanthin and lutein are also found in the rod outer segments and retinal pigment epithelium cells where they may have multiple functions. These two carotenoids are less susceptible to oxidation by pro-oxidants than are hydrocarbon carotenoids such as beta-carotene and lycopene.16 Researchers have suggested that lutein and zeaxanthin compete with beta-carotene for transport space, so excessive supplemental beta-carotene can limit the very-low-density, low-density and high-density lipoproteins in their transport of the much-needed dietary xanthophylls into the retina.17
One of the most common concerns with supplement manufacturers is that they include large amounts of beta-carotene (as a vitamin A source) in their products. This concept of more-is-better is a common misconception where vitamins and minerals are concerned. These manufacturers should very closely monitor the findings of these studies when developing formulations for patients who have visual concerns.
A recent study suggests that vitamins C and E and supplemental zeaxanthin provide significant protection against photosensitized lipid peroxidation.18 This study suggests that a higher concentration of antioxidants can spare zeaxanthin, which may allow it to provide central macular pigment for a longer time before bleaching out or decomposing.
Lycopene. Of all the carotenoids, lycopene has been shown to exhibit the highest physical quenching rate of singlet oxygen. Lycopene has very high antioxidant activity and exerts a protective effect against various diseases, including cataracts, aging of retinal pigment epithelial cells, prostate cancer and lower urinary tract symptoms in older men. Although lutein, zeaxanthin and their metabolites constitute the major carotenoids in human ocular tissues, lycopene also has been detected in high concentrations in the ciliary body and retinal pigment epithelium.19
Nutritional Concerns
Heres a look at a few nutritional components and how they are involved in eye health and overall health.
Reactive oxygen species. Oxidative damage with the unregulated production of reactive oxygen species (ROS) has been implicated in a growing list of clinical disorders such as macular degeneration, cataracts, arteriosclerosis, rheumatoid arthritis, cancer, stroke, Parkinsons disease and Alzheimers disease.
A recent clinical study suggests that a balanced combination of alpha-tocopherol, lipoic acid, coenzyme Q10, acetyl-L-carnitine and selenomethionine can successfully regulate production of ROS, as well as modulate apoptosis.20 The study found that only supplementation with a complete antioxidant formula regulated the production of mitochondrial ROS, as well as the process of ROS-mediated apoptosis. From a clinical perspective, combining several different antioxidant compounds in the composition of formulas likely offers a greater benefit than that provided by the use of a single compound or even formulas containing a limited spectrum of antioxidant compounds.
Minerals. Most manufacturers of multiple vitamins now include the full spectrum of minerals that are necessary for the utilization of most vitamins and phytochemical antioxidants. However, minerals (e.g., magnesium, sodium, copper, zinc) compete metabolically, and too much of one can interfere with another and can be harmful. For example, long-term supplemental zinc can block absorption of copper, which is necessary for bone-marrow red cell production.
In addition, the type of mineral compound makes a difference. Using zinc oxide requires an appropriate amount of copper oxide added to the formulation. The use of monomethionine zinc is the most bioavailable form of zinc and the only form that does not interfere with copper absorption. Excessive intake of supplemental zinc is detrimental to overall body health, including the health of the brain and the prostate.21-23
A Question of Balance
If each nutrient is a part of the vastly complex human biochemistry, then all the components in the infinite chemical balance of life should also be present so they can work together properly. Balance is more important than individual micronutrients.
In terms of biological and antioxidant activity, the impact on the oxidant-antioxidant balance should be expected to be greater if the formulas being used contain a wider spectrum of antioxidant compounds than with those that contain a limited number of antioxidant compounds. The protection provided by antioxidant therapy is likely to depend more on the number and diversity of antioxidants in the formulas than on the antioxidant efficacy of any single compound or ingredient.
Every diet should be backed up with a full-spectrum supplement that further guarantees daily consumption of the vital nutrients that often are destroyed by commercial food production processes.
Take the increase in cases of scurvy, for example. The National Health and Nutrition Examination Survey (NHANES III) reported 13% of men and 9% of women in the United States have blood vitamin C levels that indicate scurvy.25
Anything that affects the eye affects the entire body. The eye reflects the health of the body, with a number of specific target areas.
|
Not All Omega-6 Fatty Acids Are Bad However, good health also depends on omega-6 gamma linolenic acid (GLA), which is a downstream metabolite of omega-6 linoleic acid, and is found in sources such as black currant seed oil, borage oil and evening primrose oil. This compound is a necessary component in the downstream metabolism of omega-6 fatty acid to the series one anti-inflammatory prostaglandins (PGE1s), which are associated with healthy mucosal tissue and healthy tear film. The human body cannot metabolize omega-3 fatty acids to these specific anti-inflammatory prostaglandins.25 (See Metabolic Pathways of Omega-3 and Omega-6 Fatty Acids, below)
Successful DGLA downstream metabolism of omega-6 to the anti-inflammatory PGE1 is secured by the omega-3 acids (eicosapentaenoic acid [EPA] and docosahexaenoic acid [DHA], preferably from fish oil), which block arachidonic acid, if those particular omega-3 metabolites are present in the body. Adequate amounts of nutrient cofactors in the bodyincluding vitamins A, C and B6, magnesium, zinc, and gamma tocopherolsstabilize both omega-6 and omega-3 fatty acids and enhance the delta-6-desaturase enzymatic conversion of omega-6 fatty acid to the anti-inflammatory PGE1. They also enhance the delta-6 and delta-5 desaturase enzymatic conversion of omega-3 alpha-linolenic-acid (ALA) to EPA/DHA and the series three anti-inflammatory prostaglandins.26 All fatty acids compete for the same metabolic desaturase, so for good health, people should consume fewer trans fat omega-6s and more GLA omega-6s and DHA/EPA omega-3s.27 The body requires all of the essential fatty acids for optimal health. They are particularly important for the patient who has dry eye because PGE1s from omega-6 interrupt the inflammatory loop associated with chronic dry eye syndrome. The PGE1s also increase the anti-inflammatory immunosuppressive effects of cyclosporine. |
Regarding supplements: Why recommend a supplement that only supports your patients eyes, when you can recommend one supplement that also slows the progression of all chronic degenerative diseases and supports the prevention of vascular disease, diabetes and cancer? This is truly the embodiment of primary-care practice.
Dr. Anshel, a principal of Corporate Vision Consulting in Encinitas, Calif., has authored two books and lectures nationally on nutrition and the eyes. He is also an author, consultant and frequent lecturer on computer vision syndrome.
1. Radimer K, Bindewald B, Hughes J, et al. Dietary supplement use by US adults: data from the National Health and Nutrition Examination Survey, 1999-2000. Am J Epidemiol 2004 Aug 15;160(4):339-49.
2. Supplement Business Report 2005. Nutr Bus Jrnl 2005 Oct.
3. DeFelice SL. What is a true nutraceuticalandWhat is the nature and size of the U.S. nutraceutical market? The Foundation for Innovation in Medicine. Press release. 24 March 1994. www.fimdefelice.org/archives/arc.whatisnut.html. (Accessed 25 April 2006).
4. Age-Related Eye Disease Study Research Group. A randomized, placebo-controlled, clinical trial of high-dose supplementation with vitamins C and E, beta carotene, and zinc for age-related macular degeneration and vision loss: AREDS report no. 8. Arch Ophthalmol 2001 Oct;119(10):1417-36.
5. Fletcher RH, Fairfield KM. Vitamins for chronic disease prevention in adults: clinical applications. JAMA 2002 Jun 19;287 (23):3127-9.
6. Axer-Siegel R, Bouria D, Ehrlich R, et al. Association of neovascular age-related macular degeneration and hyperhomocysteinemia. Am J Ophthalmol 2004 Jan;137(1):84-9.
7. Abu El-Asrar AM, Abdel Gader AG, Al-Amro SA, Al-Attas OS. Hyperhomocysteinemia and retinal vascular occlusive disease. Eur J Ophthalmol 2002 Nov-Dec;12(6):495-500.
8. Bone RA, Laundrum JT, Friedes LM, et al. Distribution of lutein and zeaxanthin stereoisomers in the human retina. Exp Eye Res 1997 Feb;64(2):211-8.
9. Gale CR, Hall NF, Phillips DI, Martyn CN. Lutein and zeaxanthin status and risk of age-related macular degeneration. Invest Ophthalmol Vis Sci 2003 Jun;44(6):2461-5.
10. Wooten BR, Hammond BR. Macular pigment: influences on visual acuity and visibility. Prog Retin Eye Res 2002 Mar;21(2): 225-40.
11. Toyoda Y, Thomson LR, Langner A, et al. Effect of dietary zeaxanthin on tissue distribution of zeaxanthin and lutein in quail. Invest Ophthalmol Vis Sci 2002 Apr;43(4):1210-21.
12. Koh HH, Murray IJ, Nolan D, et al. Plasma and macular responses to lutein supplement in subjects with and without age-related maculopathy: a pilot study. Exp Eye Res 2004 Jul;79(1):21-7.
13. Rapp IM, Maple SS, Choi JH. Lutein and zeaxanthin concentrations in rod outer segment membranes from perifoveal and peripheral human retina. Invest Ophthalmol Vis Sci 2000 Apr;41(5):1200-9.
14. Junghans A, Sies H, Stal W. Macular pigments lutein and zeaxanthin as blue light filters studied in liposomes. Arch Biochem Biophys 2001 Jul 15;391(2):160-4.
15. Bone RA, Landrum JT, Friedes LM, et al. Distribution of lutein and zeaxanthin stereoisomers in the human retina. Exp Eye Res 1997 Feb;64(2):211-8.
16. Shaban H, Richter C. A2E and blue light in the retina: the paradigm of age-related macular degeneration. Biol Chem 2002 Mar-Apr;383(3-4):537-45.
17. Roodenburg AJ, Leenen R, van het Hof KH, et al. Amount of fat in the diet affects bioavailability of lutein esters but not of alpha-carotene, beta-carotene, and vitamin E in humans. Am J Clin Nutr 2000 May;71(5):1187-93.
18. Krinsky NI, Landrum JT, Bone RA. Biologic mechanisms of the protective role of lutein and zeaxanthin in the eye. Annu Rev Nutr 2003;23:171-201. Epub 2003 Feb 27.
19. Gupta SK, Trivedi D, Srivastava S, et al. Lycopene attenuates oxidative stress induced experimental cataract development: an in vitro and in vivo study. Nutrition 2003 Sep;19(9):794-9.
20. Hagen TM, Liu J, Lykkesfeldt J, et al. Feeding acetyl-L-carnitine and lipoic acid to old rats significantly improves metabolic function while decreasing oxidative stress. Proc Natl Acad Sci U S A 2002 Feb 19;99(4):1870-5.
21. Bush AI, Pettingell WH, Multhaup G, et al. Rapid induction of Alzheimer A beta amyloid formation by zinc. Science 1994 Sep 2;265(5177):1464-7.
22. Lee JM, Zipfel GJ, Park KH, et al. Zinc translocation accelerates infarction after mild transient focal ischemia. Neuroscience 2002;115(3):871-8.
23. Leitzman MF, Stampfer JF, Wu K, et al. Zinc supplement use and risk of prostate cancer. J Natl Cancer Inst 2003 Jul 2;95(13): 1004-7.
24. Hampl JS, Taylor CA, Johnston CS. Vitamin C deficiency and depletion in the United States: the Third National Health and Nutrition Examination Survey, 1988 to 1994. Am J Public Health 2004 May;94(5):870-5.
25. Furse RK, Rossetti RG, Zurier RB. Gamma linolenic acid, an unsaturated fatty acid with anti-inflammatory properties, blocks amplification of IL-1 beta production by human monocytes. J Immunol 2001 Jul 1;167(1):490-6.
26. Barabino S, Rolando M, Camicione P, et al. Systemic linoleic and gamma linolenic acid therapy in dry eye syndrome with an inflammatory component. Cornea 2003 Mar;22(2):97-101.
27. Wu D, Meydani M, Leka LS, et al. Effect of dietary supplementation with black currant seed oil in the immune response of healthy elderly subjects. Am J Clin Nutr 1999 Oct;70(4):536-43.