 |
Q: My post-LASIK patient has severe neuropathic ocular pain. I have tried punctal occlusion, Restasis, Xiidra, oral doxycycline and topical steroids to no avail. What other choices do I have?
A: Individuals with a particular dry eye profile may have a neuropathic etiology to their ocular complaints, according to Divy Mehra, BS, and Anat Galor, MD, MSPH, of the Bascom Palmer Eye Institute. They note that neuropathic ocular pain can be frustrating for patients, as they exhibit dry eye symptoms but do not find relief with traditional therapies, and practitioners, who face treatment challenges.
The Ins and Outs
Neuropathic ocular pain is caused by a lesion or disease within the trigeminal system and may manifest as spontaneous or evoked ocular pain.1 Nerve abnormalities can occur in peripheral nerves and central pathways connecting the cornea and ocular surface to the brain. They result in subthreshold activation of nociceptive neurons following subnormal or abnormal stimuli.1
Neuropathic ocular pain is a diagnosis of exclusion and should be preceded by a complete history, thorough examination and effective management of eyelid, conjunctiva and tear film abnormalities. Factors suggestive of neuropathic ocular pain include specific comorbidities (migraine, fibromyalgia), signs (pain upon touch, distal nerve termination, swelling and hyperreflectivity) and symptoms (wind and light sensitivity), as well as sign and symptom disagreement (with symptoms outweighing signs) and resistance to dry eye therapy.2-6
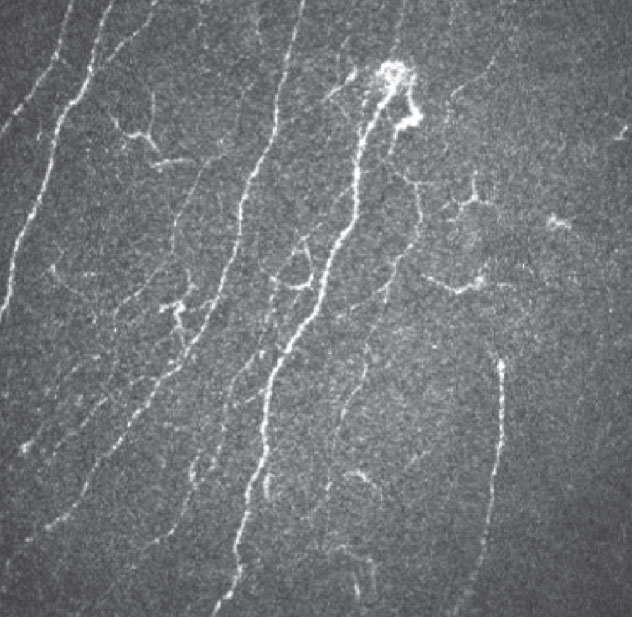 |
| In vivo confocal microscopy can identify swollen distal nerves. Click image to enlarge. |
The Ocular Pain Assessment Survey and Neuropathic Pain Symptom Inventory were developed to assess ocular pain. Nerve testing can also be incorporated into the clinical examination. For example, corneal sensation can be tested with a cotton tip or dental floss. Hypersensitivity to touch suggests hyperalgesia. The proparacaine challenge test evaluates the effect of topical anesthesia on ocular symptoms. Anesthesia should dampen the firing of peripheral, or corneal, nociceptors, eliminating pain from ocular surface damage or peripheral nerve abnormalities. Persistent pain following anesthesia suggests central, or non-ocular surface-related, mechanisms are involved.
First, treat all nociceptive sources of pain, such as tear dysfunction and ocular surface inflammation. If a neuropathic contributor is suspected, consider therapies targeting neural pathways. Local therapies, such as autologous serum tears or other blood products, may prove effective in those with peripheral ocular pain.
If a central component is suspected, consider systemic neuromodulators. Alpha2-delta ligands gabapentin and pregabalin have shown efficacy in managing neuropathic ocular pain. Other systemic neuromodulators may be used alone or in conjunction with alpha2-delta ligands, including serotonin-norepinephrine reuptake inhibitors, tricyclic antidepressants and antiepileptics.
Adjuvant therapies have also been used to target peripheral and central neural pathways, including transcutaneous electrical nerve stimulation, botulinum toxin A injection, periocular or ganglion blockage with a corticosteroid/anesthetic combination and acupuncture.
Importantly, neuropathic ocular pain has been linked to mood disorders and poor psychological coping mechanisms.7 An interdisciplinary approach addressing psychological, behavioral and neurological factors is imperative to successfully manage these cases.
Dr. Shovlin, a senior optometrist at Northeastern Eye Institute in Scranton, PA, is a fellow and past president of the American Academy of Optometry and a clinical editor of Review of Optometry and Review of Cornea & Contact Lenses. He consults for Kala, Aerie, AbbVie, Novartis, Hubble and Bausch + Lomb and is on the medical advisory panel for Lentechs.
1. IASP terminology. www.iasp-pain.org/education/content.aspx?itemnumber=1698. Accessed December 10, 2020. 2. Farhangi M, Diel RJ, Buse DC, et al. Individuals with migraine have a different dry eye symptom profile than individuals without migraine. Br J Ophthalmol. 2020;104(2):260-4. 3. Vehof J, Smitt-Kamminga NS, Kozareva D, et al. Clinical characteristics of dry eye patients with chronic pain syndromes. Am J Ophthalmol. 2016;162:59-65. 4. Kalangara JP, Galor A, Levitt RC, et al. Characteristics of ocular pain complaints in patients with idiopathic dry eye symptoms. Eye Contact Lens. 2017;43(3):192-8. 5. Ong ES, Felix ER, Levitt RC, et al. Epidemiology of discordance between symptoms and signs of dry eye. Br J Ophthalmol. 2018;102(5):674-9. 6. Aggarwal S, Cavalcanti BM, Regali L, et al. In vivo confocal microscopy shows alterations in nerve density and dendritiform cell density in Fuchs’ endothelial corneal dystrophy. Am J Ophthalmol. 2018;196:136-44. 7. Patel S, Felix ER, Levitt RC, et al. Dysfunctional coping mechanisms contribute to dry eye symptoms. J Clin Med. 2019;8(6):901. |

