Recent advances in technology have brought about many new diagnostic and therapeutic modalities. These devices have the potential to dramatically improve our efficiency and ability to properly diagnose and treat our patients.
Some technologies have received much of the recent hype in the eye care community, such as optical coherence tomography (Humphreys OCT), retinal laser polarimetry (LDTs GDx with VCC), and retinal thickness analysis and tomography (Talias RTA and Heidelbergs HRT II).
But in the background, other technological advances may have missed the spotlight, and many more are just about to surface. Here are some of the lesser-touted devices that may become valuable assets for both eye care professionals and their patients.
Auto Subjective Refraction
Topcons new BV-1000 system may prove to be very useful in some practice settings. Topcon says the BV-1000, which received FDA approval in December 2003, is the first patient-driven automated subjective refraction system.
The system includes a
simultaneous binocular autorefractor, an autokeratometer, an automatic chart projector, and a patient-driven vision tester. Voice prompts guide the patient through a practitioner selected subjective refraction process. The patient responds by manipulating one of the four joysticks. Test results are documented on a full-page prescription printout and a built-in roll out paper printout. The BV-1000 can interface with Topcons autolensmeters and its computerized vision tester.

Topcons BV-1000 uses voice prompts for its automated subjective refracting process.
Word has it that the BV-1000 is used as a stand-alone device in malls in Japan to refract customers who can then fill their prescriptions at the nearest optical. Its unlikely that patients in the United States will ever be examined solely by a Dr. BV-1000. But with confirmation and refinement of the prescription by a licensed practitioner, this state-of-the-art refracting system may prove useful in the high-volume practice. Suggested list price is $43,000, which includes the unit, table and PC.
Anterior Segment Imaging
How many times have you told a patient that his cataract has advanced during the previous year, or that she has the start of a cataract? What if you could show the patient and yourself the actual degree or progression of opacification of the lens? What if you could view the entire anterior segment in 3-D? The Oculus Pentacam Comprehensive Eye Scanner appears to answer some of these questions.
The Pentacam combines many anterior segment analyses into one piece of equipment. Using a rotating Scheimpflug camera, it can produce 3-D images of the anterior structures. The corneal topographer measures 25,000 points on the front and back corneal surfaces to draw a true elevation map. Axial and tangential maps can also be selected. Pachymetry measurements can be obtained from anywhere on the cornea, centrally and peripherally.

Oculus Pentacam Comprehensive Eye Scanner.
The Pentacam automatically calculates anterior chamber volume, height and angle in degrees, and detects and quantifies lens opacification. You can also obtain specific manual measurements of the anterior chamber diameter, implantable contact lens (ICL) vault, and anterior chamber IOL location. These functions allow the Oculus Pentacam to serve as a valuable primary care and comanagement tool.
Contact the company for pricing information.
Ultrasound Pachymetry
Thanks to the results of the Ocular Hypertension Treatment Study (among other studies),
pachymetry has been a hot topic lately. Put simply, pachymetry is the measurement of the thickness of the cornea. But accurate corneal thickness measurement is not so simple. Ultrasound, optical, and optical coherence tomography provide different methods for obtaining this measurement.
Pachmate DGH 55 handheld pachymeter.
Ultrasound pachymetry, due to its portability, accuracy and ease of use, has become the preferred method in many eye care settings.
While ultrasound pachymetry in itself is not new technology, it has recently become the de facto standard in the diagnosis and management of glaucoma since it was the method used in the OHTS study. That study showed that, as a general rule, a central corneal thickness of less than 555m should be viewed as a risk factor for the development of glaucoma. Pachymetry allows the calculation of adjusted intraocular pressures by taking into account that thicker corneas can give falsely high IOP measurements.
Choosing a pachymeter among the numerous brands and styles can be a daunting task. Whether you are looking for portability, capability or precision, there is a pachymeter that will fit your needs. Here are some of the new pachymeters on the market today:

Pocket II Precision Pachymeter from Quantel.
Handhelds. With regard to size and portability, the Pachmate DGH 55 handheld pachymeter by DGH Technologies weighs less than nine ounces and is less than seven inches long. It can rapidly store up to 25 measurements bilaterally and gives audio feedback indicating valid measurements and completion of measurement groups.
Another handheld, Quantels Pocket II Precision Pachymeter is about the size of a videocassette tape and weighs 16 ounces. It operates on four AA batteries and can be connected to a standard computer printer, allowing a full-size printed record.
A Palm Pilot-like device, the IOPac from Heidelberg Engineering has five built-in formulas to correct CCT measurements for true IOP. Or, you can program up to three formulas of your own. It can store up to 1,000 measurements, and can hook up to your PC through a USB port or to your printer by infrared transmission.
For $2,995 for the Pachmate 55, $3,395 (non-discounted price) for the Pocket II, and $3,495 for the IOPac, you can put one of these little devices in your pocket, literally. (A base model IOPac, without the full features, goes for $2,495.)
Portables. Other pachymeters may be a bit larger, but still offer portability. Some of these come with more featuresfor example, both of the following pachymeters can be connected to a printerbut they all do the job of measuring central corneal thickness.
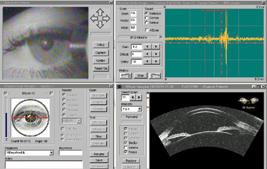
Artemis-2, from Ultralink LLC, is a high frequency ultrasound eye-arc scanner.

The Cornea-Gage Plus 2 by Sonogage weighs about five pounds, but offers great precision with a 50 MHz transducer that allows epithelial and direct flap measurements. It has a continuous read mode and will calculate averages for each measurement. The price tag on this device can run around $2,850.
DGH Technologies also offers the Pachette 2, another portable device. It quickly and automatically stores 50 measurements and simultaneously displays the current measurement and the average of all measurements on a LCD display. It also has a FLAP option for measuring the thickness of LASIK flaps. This one is priced about $2,795.
Combination Instruments. If you are looking for the latest device with all the bells and whistles, take a look at some of the newest instruments that combine pachymetry with scanning technology.
The new Echoscan US-1800 by Nidek, which recently received FDA approval in November 2003, is a pachymeter and A-scan combination unit. Inputs and options are selected via a 10.4-inch LCD touch screen. The instrument has an integrated thermal printer and can perform advanced IOL calculations. But if you order the instrument, dont forget to ask for the pachymeter probe, which is listed as optional. The list price for the Echoscan US-1800 is $8,500.
Another combination instrument is the Artemis-2 by Ultralink LLC. The company says this is the worlds first very high frequency digital ultrasound eye-arc scanner. Its an A-scan, B-scan and pachymeter all in one. Testing results are displayed on a 15-inch LCD display in a multi-window format. It allows for a full
corneal thickness profile that can be displayed as a pachymetric topography. It will also provide 2-D and 3-D thickness images of the flap, residual stromal bed, and anterior and posterior chamber structures. The company says this instrument is poised to be the technology for monitoring phakic IOL patients. This instrument is custom built, and there are fewer than two dozen in the U.S. at this time. The price is $89,000.

Nideks Echoscan US-1800.
This is by no means a complete list of pachymeters on the market. There are several other manufacturers and pachymeters available.
Corneal Viscoelasticity
Now that OHTS has called everyone to hop onto the pachymetry bandwagon, new technology might be altering the way we think about intraocular pressure. Are two corneas identical if measurements show they have the same thickness and the same pressure?
Traditional methods of attaining intraocular pressure include non-contact tonometry and Goldmann applanation tonometry, both of which are subject to the effects of corneal resistance. Another factor to consider in the battle against glaucoma is the corneal response (or hysteresis). The Ocular Response Analyzer (ORA) from Reichert is the first instrument of its kind to perform both pachymetry and corneal response.
In a single, cornea-free measurement, the ORA records two applanation events; one as the cornea moves inward and a second as the cornea moves outward returning to its original shape. The difference between these two measurements is known as the corneal hysteresis. This is an indication of the biomechanical properties of the cornea that include thickness, rigidity, hydration and other yet undetermined factors.

Reicherts Ocular Response Analyzer.
With this information in hand, the ORA gives us a new ocular parameter called Excess Ocular Pressure (EOP). This is the deviation from normal population pressure, based on traditional IOP and complete corneal effects. This population normality is based upon a database of IOPs and corneal hystereses of 144 normal (and primarily Caucasian) eyes between the ages of 25 and 65. Further studies, the company says, have shown this normative data to be transferable to many populations.
An important aspect to this new technology relates to current treatment parameters. While the ORA allows confirmation of elevated or normal IOP taken via traditional methods, it most importantly brings to light false positives. These are cases in which the IOP appears elevated but the EOP, which takes into account corneal biomechanics, is not. Typically, we would put these patients through a glaucoma work-up and then possibly on medication. This new technology could prevent this eventuality.
In addition, the Ocular Response Analyzer can be used to predict refractive surgery outcomes and monitor for corneal ectasia. The instrument hits the market this month at a suggested list price of $16,071.
Monitoring Blood Glucose
But my blood sugar is normal!
How many times have you heard those words come out of your patients mouth? Along with the overuse or abuse of contact lenses, this is perhaps one of our greatest frustrations in primary eye care. Unfortunately, we must either rely on patients to remember their blood sugar or hemoglobin A1c levels or hope that their primary care doctor or endocrinologist sends us the desired information. A new device called the A1cNow by Metrika may help us to win some of these battles.
While measuring blood glucose on a daily basis remains the standard of care for all diabetics, the measurement is limited to the specific moment the test is performed. Daily monitoring is essential for making immediate adjustments, but hemoglobin A1c (HbA1C) testing shows a patients average blood glucose over the previous 60-90 days.
This measurement is possible due to red blood cells in the body. They contain hemoglobin, which becomes glycated by excess sugar in the body. As blood sugar increases, the amount of glycated hemoglobin present in the blood stream also rises. Red blood cells live approximately three months. Not by coincidence, this is the time frame of the test. The percentage of hemoglobin glycated that is considered normal or non-diabetic is 4-6%.
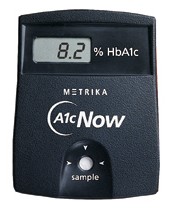
A1cNow blood glucose monitor from Metrika.
A1cNow is a single-use disposable monitor that can be used in the physicians office or by the patient at home. Once a diluted sample of blood is added to the monitor, results are available in eight minutes. It has been shown to have an accuracy of over 99%. This new technology will not only allow patients to have better control of their diabetes, but put to rest many of the questions that we may have about their diabetes management.
The device retails for $25 and can be purchased in drug stores.
Historically, the profession of optometry has embraced new developments and technologies to enhance patient care. Advanced technology allows us to better treat and manage disease, and to better detect undiscovered problems. The devices described here may prove to enhance our knowledge and practice ability.
The authors have no financial interest in any of these products or companies.
Dr. Gardner is currently completing a primary care residency at Nova Southeastern University in Ft. Lauderdale, Fla. He plans to practice in Philadelphia next year. Dr. Taub is currently completing a pediatric/binocular vision/primary care residency at Nova Southeastern University, where he plans to remain as an instructor.

