 |
In this new column, “The Essentials,” I hope to reinforce the basic science principles and clinical techniques essential to optometry. The hope is that by revisiting these concepts in both a succinct and clinically relevant manner, we may advance our understanding as both scientists and clinicians, and ultimately provide better and more comprehensive patient care. Sometimes, recognizing a new angle on the staple anatomy, physiology and techniques can provide us with fresh, new insight into diagnosis and management.
A Case of the Nerves
A 52-year-old Caucasian male presents to your office with unilateral orbital swelling, pain and vision loss of one week’s duration. Examination also reveals restricted abduction and a hyper deviation in his left eye. His ocular history is otherwise non-contributory. His systemic history is positive for a previous diagnosis of squamous cell carcinoma (SCC) of his hard palate one year ago, for which he had undergone surgery and radiotherapy at that time. No lymphadenopathy—visible or palpable mass—is present.
What is your primary differential? Is the patient’s history pertinent to his current clinical presentation?
The evaluation of the cranial nerves is an essential part of any eye examination. If an abnormality is found, we focus on identifying the underlying etiology and, if necessary, localizing the suspected lesion through careful history, extraocular muscle evaluation and a basic neurological exam. Often, when see multiple cranial neuropathies, our first instinct is to evaluate for pathologies located within the cavernous sinus. While this is an appropriate differential consideration, as it contains multiple cranial nerves, we frequently fail to recognize that this isn’t the only site where several nerves are closely confined in a small space.1-3
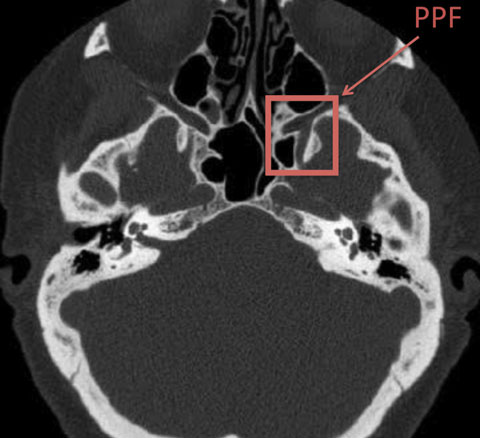 |
| This computed tomography scan shows the location of the pterygopalatine fossa. |
Same Face, New Space
The pterygopalatine fossa (PPF) is a bony space located anteriorly on each side of the skull base. This structure houses the pterygopalatine ganglion, the largest of the four parasympathetic ganglia of the head and neck. The potential for multiple cranial neuropathies exists not only because this ganglion resides within the PPF but also because this fossa acts as a passageway between several cranial compartments. Thus, it serves as a conduit for disease to spread to numerous, otherwise isolated, anatomical locations.3
The PPF is located amidst the maxillary, sphenoid and palatine bones and contains several openings and foramina (Table 1). The PPF is in communication with the orbit, oral cavity, nose, infratemporal fossa, cavernous sinus and the skull base, to name a few.1-2 Let’s review two of these openings and structures, focusing on those that act as a passageway for disease to spread to affect orbital structures.
The foramen rotundum. This space is in direct communication within the PPF, where the maxillary nerve passes. The maxillary nerve is the second branch of the trigeminal nerve (CN V2), and innervates sensation to the mid portion of the face, including the lower portion of the eye.1,2 Since this branch also runs through the cavernous sinus, any pathology within the PPF can spread directly into the cavernous sinus, and ultimately the brain, via this opening. It can be examined clinically with the cotton wisp test to check for the sensitivity in the location of each branch of the trigeminal nerve on either side.
The inferior orbital fissure. This opens into the superior portion of the PPF, allowing direct contact with the orbital cavity. Passing through the inferior orbital fissure is the zygomatic branch of CN V2, and the infraorbital artery and vein. Since there is no barrier separating the inferior and superior orbital fissures, disease can easily spread from the PPF to the inferior orbital fissure, and ultimately to the superior orbital fissure, which contains cranial nerves III, IV, VI and V1.1,2
Table 1. Review of Pterygopalatine Fossa | ||
| Opening | Contents | Innervation |
| Pterygomaxillary fissure | • Posterior superior alveolar nerve • Maxillary artery | Sensory stimulation to infratemporal maxillary |
| Foramen rotundum | • Maxillary nerve (CN V2) | Sensory stimulation to mid portion of the face |
| Vidian canal | • Vidian nerve, artery, and vein | Parasympathetic stimulation to the nose, palate and lacrimal gland |
| Pharyngeal canal | • Pharyngeal branch of the maxillary nerve and artery | Mucosa of the nasopharynx |
| Inferior orbital fissure | • Zygomatic branch of maxillary nerve • Infraorbital artery and vein | Lacrimal gland |
| Greater palatine canal | • Greater palatine nerve | Sensory and parasympathetic stimulation to mucous membrane of hard palate |
| Lesser palatine canal | • Lesser palatine nerve | Sensory and parasympathetic stimulation to soft palate, tonsils and uvula |
| Sphenopalatine foramen | • Sphenopalatine artery and vein • Nasopalatine nerve | Mucosa of anterior hard palate and nasal septum |
Clinical Impact
Why do all these openings and connections matter? Pathologies such as infections and neoplasms, which may otherwise be confined to a certain anatomic location, can easily travel via these connections to remote compartments.
In our case presentation, cavernous sinus pathologies such as a fistula are appropriate differentials. However, a tumor may spread from the PPF to the orbit through the inferior and superior orbital fissures and present in similar fashion. In this case, our patient was diagnosed with recurrent SCC involving orbital metastasis. So, be sure to bear in mind the other tight spaces that can harbor the pathologies causing your patients to experience multiple cranial neuropathies.4,5
|
1. Hansen JT, Netter FH. Essential Guide to Netter’s Anatomy. Singapore:Elsevier, 2011. Print. 2. Hansen JT, Koeppen BM, Netter FH, et al. Atlas of Neuroanatomy and Neurophysiology: Selections from the Netter Collection of Medical Illustrations. Teterboro, NJ: Icon Custom Communication, 2002. Print. 3. Khonsary S, Ma Q, Emerson J, Malkasian D, Villablanca P. Clinical functional anatomy of the pterygopalatine ganglion, cephalgia and related dysautonomias: A review. Surg Neurol Int. 2013;4(7):422. 4. Khan SN, Sepahdari AR. Orbital masses: CT and MRI of common vascular lesions, benign tumors, and malignancies. Saudi J of Ophthalmol. 2012;26(4):373–83. 5. Tashi S, Purohit BS, Becker M, Mundada P. The pterygopalatine fossa: imaging anatomy, communications, and pathology revisited. Insights into Imaging. 2016;3:1-11. |

