 |
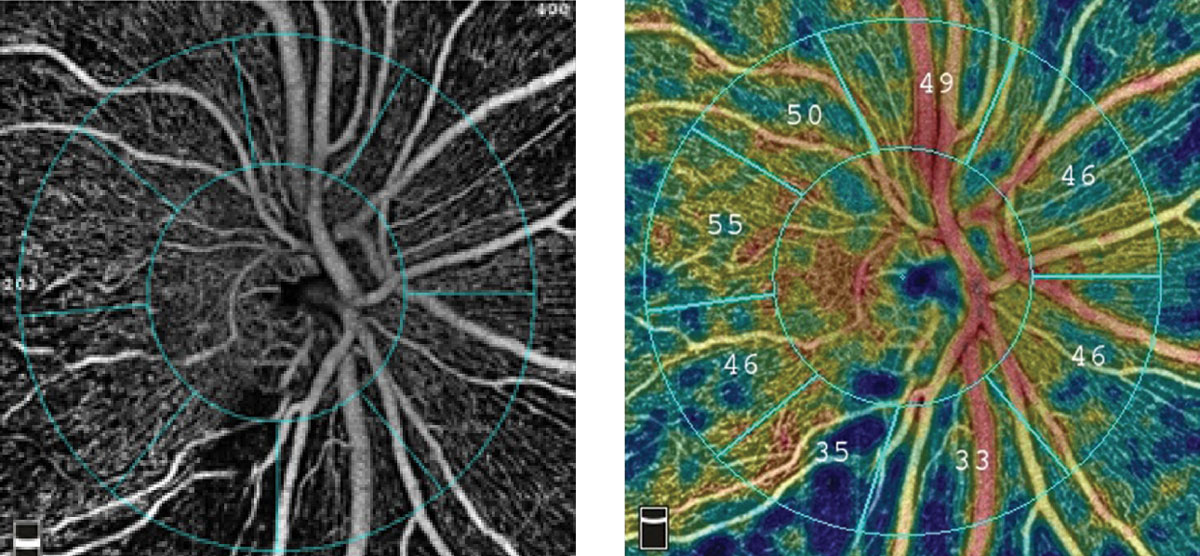
The pathogenesis of GON may involve systemic vascular dysregulation. Photo: Optovue. Click image to enlarge. |
While intraocular pressure (IOP) is the driving force behind glaucomatous optic neuropathy (GON), those with low-tension glaucoma (LTG) don’t present with elevated pressures. Researchers say there are other variables and risk factors at play that can cause cellular injury in the initiation and/or progression of GON besides IOP.
“Genetic predisposition, inflammatory and immune responses, structural and mechanical stress, mitochondrial dysfunction, oxidative stress and vascular dysfunction may modulate the pressure-associated perceived stress of the retinal ganglion cell or may even act in an IOP-independent mechanism,” the researchers explained in their paper. “Of these, one of the leading proposed mechanisms of retinal ganglion cell injury, particularly in LTG, is based on the vascular hypothesis…[which] suggests that GON occurs in part due to diminished perfusion of the optic nerve by the peripapillary microcirculation leading to retinal ganglion cell stress and ultimately cell death and atrophy.”
Their study, recently published in the Journal of Glaucoma, reported that there are multiple systemic, vascular-associated conditions associated with LTG, including systemic hypertension and hypotension, diabetes mellitus, migraine headache, peripheral vascular disease, Raynaud’s syndrome and anemia. “This study strengthens evidence for the vascular hypothesis of LTG,” they noted.
They conducted a retrospective case-control study to identify patients seen at the Mayo Clinic Department of Ophthalmology for LTG between 2005 and 2015 (n=277). An age- and sex-matched control group was also included (n=277). They selected patients with LTG because “GON is likely a multifactorial disease with a number of systemic risk factors including those that may affect a patient’s hemodynamics and ultimately their ocular perfusion pressure,” they explained in their paper.
They reported that the LTG group had significantly more myopic refractive errors (-1.6D vs. -1D), lower IOP (14.2mm Hg vs. 15.2mm Hg) and a higher cup-to-disc ratio (0.7 vs. 0.3) than the control group. They also noted that the LTG group was significantly less likely to be obese (BMI >30).
Additionally, the LTG group had significantly higher prevalence of certain systemic conditions, including hypertension, diabetes mellitus, peripheral vascular disease, migraine headache, anemia, systemic hypotension, Raynaud’s syndrome, angiotensin-converting enzyme inhibitor and calcium channel blocker use. Calcium channel blocker use remained significant after adjusting for systemic hypertension. The researchers also reported no significant differences regarding hyperlipidemia, obstructive sleep apnea (OSA), coronary artery disease, carotid stenosis, stroke, statin, ACE inhibitor, angiotensin receptor blocker, beta blocker or metformin use.
The researchers say that according to the vascular hypothesis, systemic vascular dysregulation “may play a more prominent role in LTG compared with other types of open-angle GON.” Patients with high or low blood pressure, anemia, cardiac disease or stroke are more likely to experience lower-end organ perfusion and systemic vascular dysregulation, they said.
“From a blood pressure standpoint, our study supports the parabolic nature of risk with both systemic hypertension and hypotension being risk factors for LTG,” they wrote. “Coronary artery disease and stroke have been reported to have an association with glaucoma; however, our study did not find an association with either condition.” Additionally, contrary to some studies, but aligned with others, the present study didn’t show an association between LTG and dyslipidemia.
The significant associations between LTG and Raynaud’s syndrome and between LTG and migraine in the study also support the idea of reduced perfusion as a factor in GON, the researchers explained. Raynaud’s syndrome is caused by peripheral vasospasm, leading to dysregulation of peripheral perfusion. “It’s been suggested to be an independent risk factor for the development of LTG,” the researchers wrote. “Migraines are also thought to be precipitated by a vasospastic mechanism, which could alter ocular perfusion pressure, and previous reports suggest that migraine headaches could be a risk factor for the development and progression of glaucoma. Anemia…would presumably be a vascular risk factor for LTG by reducing optic nerve oxygen delivery.”
In terms of systemic medications, the researchers say they found calcium channel blockers to have a significant association with LTG in their study, though previous literature shows conflicting evidence. Previous studies have also shown “nonsignificant risk reductions of systemic beta blockers and glaucoma development. Systemic beta blockers alter systemic vascular regulation but also play a role in aqueous production and IOP reduction, which may make finding associations between beta blockers and LTG difficult. Our study found no significant difference in the prevalence of systemic beta blocker use and LTG.”
They wrote that systemic inflammation and metabolic stress (e.g., diseases such as diabetes mellitus, obesity and OSA) may disrupt axonal transport and lead to retinal ganglion cell death. While they noted that diabetes and other causes of metabolic stress may have multiple mechanisms contributing to retinal damage, overall, they said that diabetic patients have demonstrated higher rates of LTG prevalence and glaucoma progression. “In contrast, the Advanced Glaucoma Intervention Study didn’t find diabetes to be associated with progressive visual field loss,” they noted. “It’s even been suggested that diabetes may confer a decreased risk for glaucoma. Our data show that LTG patients were significantly more likely to have diabetes mellitus, supporting the hypothesis for diabetes being a risk factor for LTG.”
Overall, the researchers say their study supports the vascular hypothesis for glaucomatous neuropathy.
Funk RO, Hodge DO, Kohli D, et al. Multiple systemic vascular risk factors are associated with low tension glaucoma. J Glaucoma. November 3, 2021. [Epub ahead of print]. |

