 |
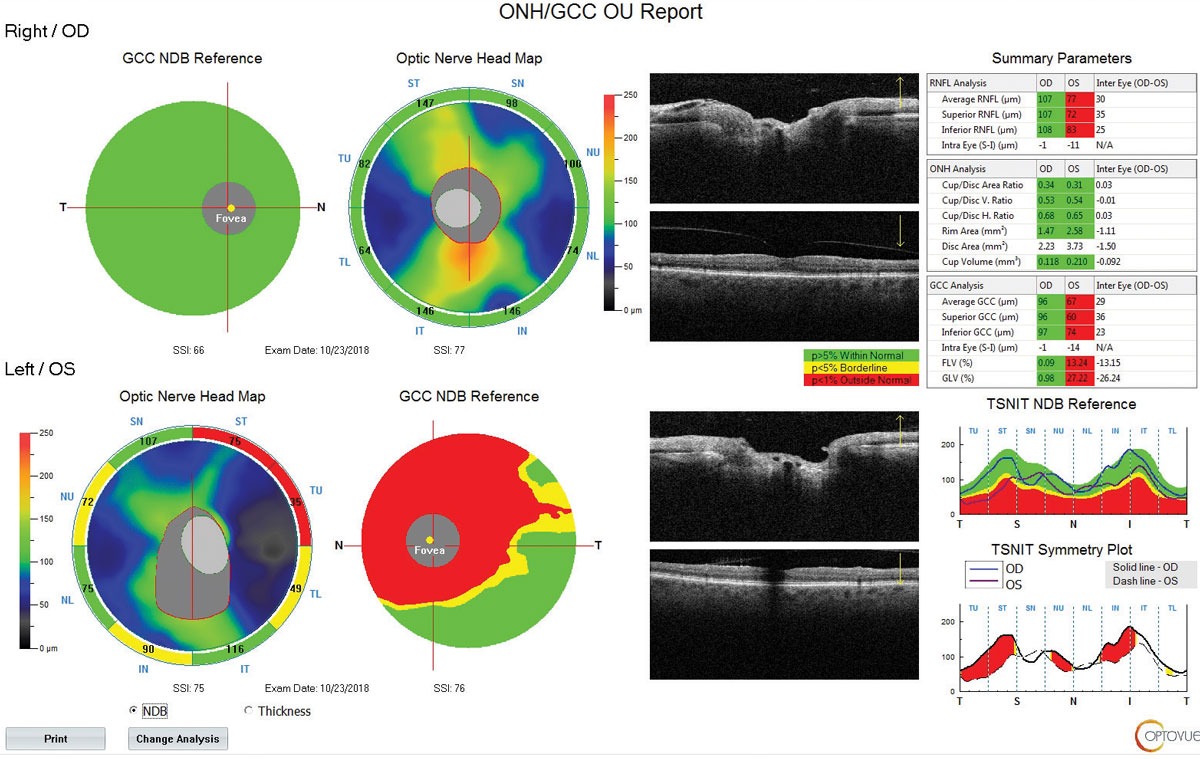
| Assessing microvasculature dropout may help detect patients with aggressive POAG. Photo: Michael Cymbor, OD. Click image to enlarge. |
To better understand the relationship between macular ganglion cell complex thickness and choroidal microvasculature dropout in primary open-angle glaucoma (POAG), researchers initiated a longitudinal study to explore the rate of ganglion cell complex thinning among POAG patients with and without microvasculature dropout. The data demonstrated that global ganglion cell complex thinning was significantly faster in eyes with microvasculature dropout compared with those without the condition.
This analysis included patients from the Diagnostic Innovations in Glaucoma Study with at least 1.5 years of follow-up and a minimum of three visits. All enrolled patients underwent OCT-A and SD-OCT imaging. The researchers used linear mixed-effects models to compare rates of global and hemisphere ganglion cell complex thinning among patients with and without microvasculature dropout.
Sixty-three patients—36 eyes with microvasculature dropout and 37 eyes without—were followed for a mean of 3.3 years. Among the eyes with microvasculature dropout, 16 showed the condition in the inferior region and 15 eyes had microvasculature dropout located in both the inferior and superior sectors.
In 30 out of 36 eyes, microvasculature dropout was localized in the inferotemporal region. Additionally, the study authors reported that the presence of microvasculature dropout as well as its area and angular circumference were independently correlated with a faster rate of thinning.
Microvasculature dropout could be an independent predictor for accelerated ganglion cell complex loss among glaucoma patients, especially in early-stage disease. “The rate of ganglion cell complex thinning was faster in eyes with evidence of microvasculature dropout and thinner ganglion cell complex loss at baseline,” the study authors concluded. “The rate of ganglion cell complex loss thinning was significantly higher in both superior and inferior regions and the extent of microvasculature dropout was also associated with the rate of ganglion cell complex thinning in the future.”
Based on these findings, the researchers suggest that assessment of microvasculature dropout, especially among patients with early POAG, could be useful for the detection of individuals at a high risk of rapid progression and who may need more intensive management.
Micheletti E, Moghimi S, El-Nimri N, et al. Relationship of macular ganglion cell complex thickness to choroidal microvasculature dropout in primary open-angle glaucoma. Br J Ophthalmol. January 13, 2022. [Epub ahead of print]. |

