26th Annual Surgery Report- MIGS: Indications and Complications |
As the first—and so far only—trifocal intraocular lens (IOL) available in the United States, the PanOptix (Alcon) is different from any other multifocal IOL in our armamentarium. Our surgery center has been working extensively with this new lens, and the results have been favorable so far. As with all multifocal IOLs, the PanOptix does involve trade-offs, and your patient must be realistic about what this lens can deliver. However, it also brings some new features not available in other lenses.
This article discusses the new lens design, how to identify good and bad candidates, how it compares with other lenses and post-op tips.
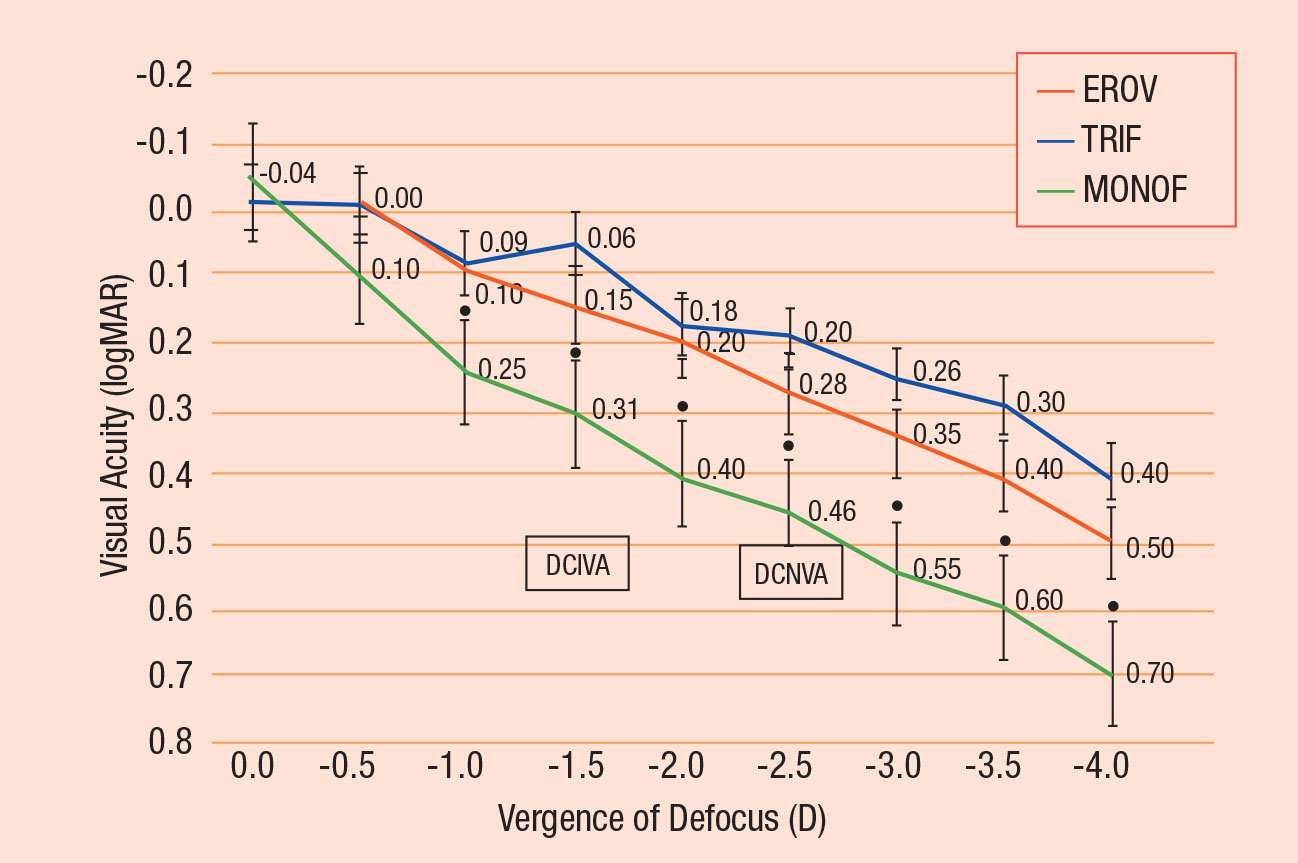 |
| Fig. 1. Mean binocular visual acuity with correction for distance vision measured four months postoperatively through three different IOLs: the Alcon PanOptix (blue), the J&J Symfony (red) and the Alcon monofocal AcrySof SN60WF (green). The PanOptix demonstrates peaks at plano, -1.50 and -2.50.11 Click image to enlarge. |
A Different Kind of IOL
The PanOptix is an ultraviolet-filtering, foldable, one-piece lens. The anterior surface has an inner 4.5mm diameter diffractive zone and is designed with a slight negative spherical aberration to counteract the positive spherical aberration of the average human cornea.1 The PanOptix has three focal points: emmetropia, +1.67D (60cm, or 24”) and +2.50D (40cm, or 16”). The lens distributes 44% of incoming light energy to the far focus, 22% each to the intermediate and near foci, while 12% is lost.2
Previously, multifocal IOLs available in the United States created a bifocal optical system (with the ability to extend depth of focus in some cases). As a result, surgical centers have had to match the appropriate lens to the patient’s preferred near point. The PanOptix’s trifocal design makes this decision less important, and the three foci correspond well to most common tasks that require sharp acuity, such as driving, computer use and reading (Figures 1 and 2).
Good vision in any multifocal IOL requires tight astigmatism control. PanOptix is available in toric powers, with half-diopter steps that correspond to corneal astigmatism from roughly 1.00D to 2.50D. Keep in mind, only corneal astigmatism (i.e., keratometry) justifies a toric IOL, not total refractive astigmatism.
Update Your Candidate Pool
Personality type is the key predictor of success with any multifocal IOL, including PanOptix.3 Ideally, your patient should have a positive approach to life and be strongly motivated to see without glasses. Researchers have studied correlations between personality traits and satisfaction with multifocal IOLs and found patients with dominant traits of conscientiousness and agreeableness have the highest satisfaction.4
Patient selection should also include an individual’s hobbies and habits. For example, a patient who wants to hike, shop online and read, all without glasses, might be well served by the three focal points of the PanOptix.
A patient’s visual status is another important factor. Hyperopes have generally been the low-hanging fruit for multifocal IOLs; they often begin wearing correction later in life and are sometimes strongly motivated to return to freedom from glasses.
Historically, clinicians have shied away from promoting multifocal IOLs to myopes, as they are often highly accustomed to wearing glasses. However, we have found that myopes can be strong candidates for the PanOptix, since the lens allows them to keep their functional near vision while also providing useful intermediate and distance vision. However, they must be aware and accepting of the aberrations intrinsic to multifocal IOLs.
Diffractive optics are not a biologically evolved focusing system, and even the best candidates usually require an adaption period.5 Neuroadaptation refers to changes the brain undergoes to accommodate a new condition—in this case, the visual system learning to work with a new way of seeing. According to fMRI studies, this process continues for approximately six months after implantation of a multifocal IOL.6 It can be helpful to educate potential candidates that, while their vision should be good initially, they may notice improvements for months after the procedure.
For patients with very mild cataracts, you can trial multifocal contact lenses before surgery as a rough approximation of the kind of vision they can expect with a multifocal IOL.7 The simulation is rough but can yield important insights.
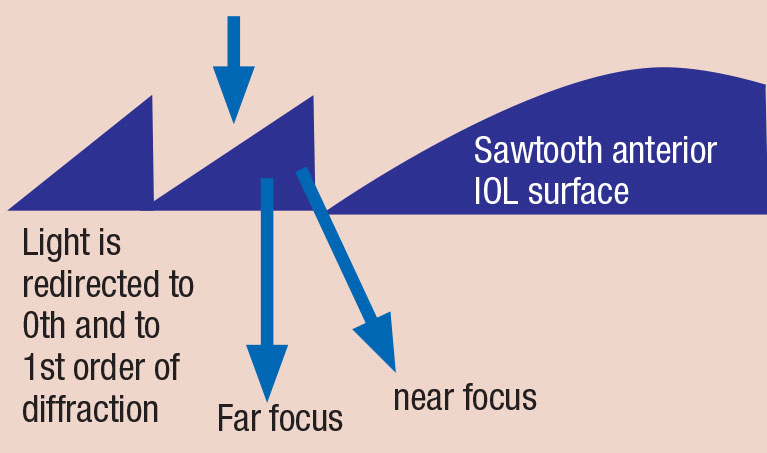
A Quick Guide to Diffractive Optics
Most modern multifocal IOLs now incorporate diffractive optics, because difraction offers better use of light with fewer dysphotopsias than simple refraction. Diffraction occurs when light passes a sharp-edged obstruction—for instance, the concentric saw-tooth pattern on the surface of a multifocal IOL—and it propagates forward as waves. The speed of light is faster in aqueous than in the lens material, so the thicker side of each saw-tooth delays the light by approximately half a wavelength. When the light waves exit the posterior lens surface, they produce bands of constructive and destructive interference: bands where the light reinforces itself, and bands where the light negates itself.1,2 Typically, bifocal IOLs use the base refractive power of the IOL for far vision and diffracted light to create a near focus (first-order diffraction). However, diffraction must also bend some light in diminishing amounts toward even closer foci (e.g., second order, third order, etc.). This light is lost to useful vision and produces glare and haloes. The second diffractive order has a vergence that is double the amount of the first order, so if the bifocal is designed for a +3.00D add, the second order will have a vergence power of +6.00D.3 Trifocal IOLs use light diffracted to both an intermediate and a near focus.4 They are designed so that the otherwise wasted light from the intermediate focal point’s second diffractive order strengthens the near focal point. This is why bifocal IOLs lose about 19% of incident light, while the PanOptix only loses 12%.
|
Red Flags
The PanOptix, like all IOLs, comes with trade-offs, and you must give candidates realistic expectations of what the lens can and cannot deliver.
The lens creates permanent haloes and starbursts around all point sources of light; these are especially evident at night, but may also cause a slight softening of vision during the daytime. Patients who require crisp vision above all else, or patients who need sharp nighttime vision (e.g., bus drivers or truckers), will be happier with single-focus IOLs.
Individuals with a dominant personality trait of neuroticism (i.e., they report frequent mood swings, are often anxious or irritated, struggle to relax and often feel down) are not likely to enjoy multifocals of any kind and will do better with a simpler lens.8
Dissatisfaction with multifocal IOLs is also strongly correlated with personality traits of orderliness and compulsive checking.8 In your clinic, these traits may manifest as frequent dissatisfaction with their vision correction, and a multifocal IOL is likely a mistake for these patients.
The three focal points of the PanOptix are well-suited to many activities, but be cognizant of the patient’s specific distance needs. A cellist, for instance, will want sharp vision at their music stand, typically close to 36”. A hunter who wants to see the iron sight on the end of their firearm may want a focal distance at 40”. The PanOptix’s 24” intermediate point will not help at those distances.
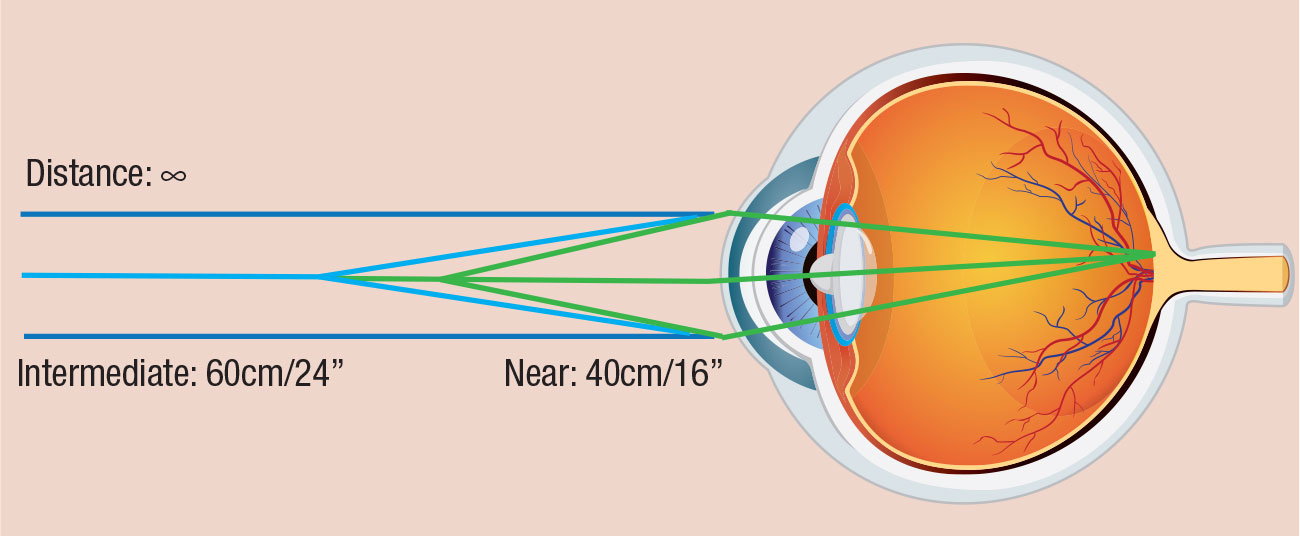 |
| Fig. 2. PanOptix is designed for three focal points: plano (distance), intermediate (60cm, or 24”), and near (40cm, or 16”). Image adapted from Alcon. Click image to enlarge. |
Some Things Don’t Mix
Almost any ocular disease that permanently limits vision, such as corneal and macular diseases, is an absolute contraindication for a PanOptix IOL. Like all multifocal IOLs, PanOptix degrades contrast sensitivity, and these diseases compound this effect.
Many surgeons will implant a PanOptix in post-LASIK patients if everything else is favorable, but very few will do so if the patient has undergone radial keratotomy. We do not offer the PanOptix to monocular or amblyopic patients, as the lens works best binocularly.
Dry eye also represents a challenge. Multifocals rarely give chronic dry eye patients stable enough vision to be worth the cost. However, if you feel confident the dry eye can be successfully managed for the patient’s lifetime, it is reasonable to consider the PanOptix. It is important to discuss this carefully with your patient to make sure they fully understand their commitment.
The PanOptix must control astigmatism to work well. If your patient has corneal astigmatism in excess of 3.00D, even the toric version will not provide good vision.
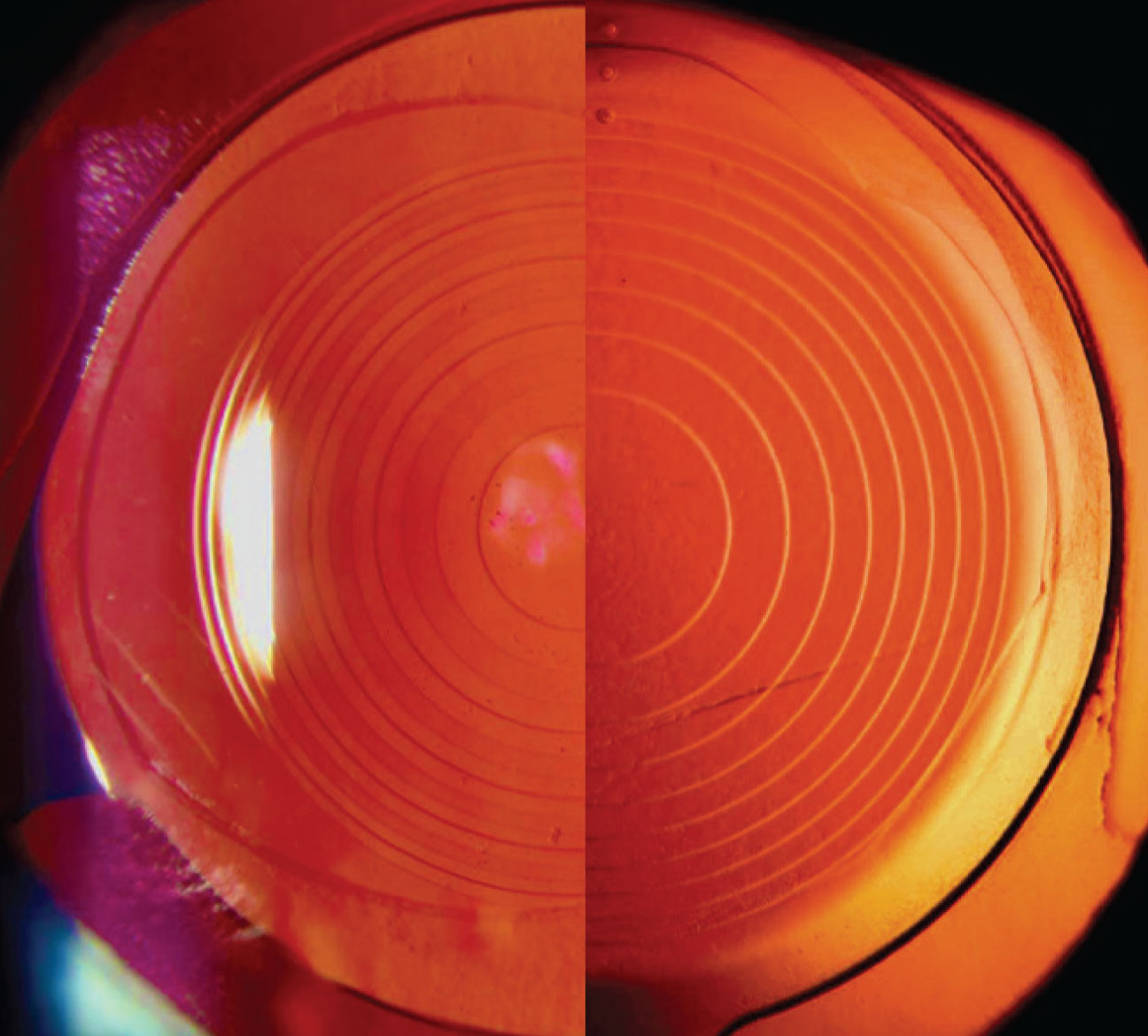 |
| Fig. 3. Side-by-side slit lamp view of the PanOptix (left) and the Symfony (right). The PanOptix has a smaller central optic and syncopated ring spacing. Images: Aaron Bronner, OD. Click image to enlarge. |
The Competition
PanOptix enters a US market dominated by single-focus IOLs. At present, only 7% of cataract patients elect multifocals—all others choose monofocals. Due to its trifocality, PanOptix already has proven itself a formidable competitor in the current IOL landscape. Head-to-head studies comparing PanOptix to bifocal IOLs are rare, but so far, the limited investigations tend to show greater patient satisfaction and fewer visual side effects with the PanOptix.2
Perhaps the most significant competitor to the PanOptix is the Symfony (Johnson & Johnson Vision). Although the Symfony and the PanOptix have very different designs, they are currently the most optically sophisticated IOLs available domestically (Figure 3). The Symfony, marketed as an extended depth of vision IOL, is functionally akin to a bifocal IOL, with a near point at +1.75D (57cm, or 22”). This causes the focal points to overlap, especially through a small pupil.9
In head-to-head trials between the PanOptix and the Symfony, patients’ distance and intermediate vision were indistinguishable between the two IOLs, but uncorrected near vision was better with the trifocal.9,10 Both lenses are known for reduced glare and haloes compared with other multifocals.11,12
In optical bench comparisons, PanOptix and Symfony rate almost identically. They measure similarly on modulation transfer function, which combines resolution (i.e., acuity) and contrast sensitivity into one graph, and on the Strehl ratio, which quantifies how much an optical system aberrates a point source of light.11,13 Their resolution is not as crisp as that of a monofocal, but close.
We have implanted several patients with a PanOptix in one eye and a Symfony in the other to achieve a variation of monovision, and have observed good results. Anecdotally, these patients report a very slight superiority in crispness at distance through the Symfony compared with the PanOptix. Thus, I consider the Symfony a good IOL for active patients who prioritize acuity but would like some near vision, and I suggest the PanOptix for patients who pursue a wide range of activities and want to read without glasses.
On the Horizon
The PanOptix is not the only trifocal IOL in the global market, since these IOLs have been available outside the US since 2010. Besides the PanOptix, the worldwide market leaders are AT Lisa (Carl Zeiss Meditec) and FineVision trifocal extended depth-of-focus lens (PhysIOL). Both AT Lisa and FineVision come in toric models, and they share many of the high-performance qualities of the PanOptix.1 The crucial difference is that their intermediate focus is at 1.67D (80cm, or 31”), which is significantly less useful than the 24” intermediate focal point of the PanOptix. For comparison, a 31” focal point is the comfortable reading distance for an individual who is 6’8”. Other pseudo-accommodative IOLs are in the pipeline, and these appear to offer several advantages. Poised to enter the market soon are several non-diffractive IOLs, including the Alcon Vivity and Johnson & Johnson Eyehance, both of which purport to use advanced manipulation of the wavefront to achieve an extended range of focus with minimal compromise to distance vision.2 Also, Johnson & Johnson expects to soon release an updated and more powerful version of the Symfony IOL—the Symfony Plus—as well as a hybrid extended depth of focus/multifocal lens, the Synergy IOL.3 The AcuFocus IC-8 uses a much older technology to extend the depth of focus: the pinhole effect. The IC-8 has an opaque annular mask with a central aperture diameter of 1.36mm. Crucially, doctors have found it is still possible to do a fundus exam and even retinal procedures in patients implanted with this IOL.4
|
Post-op Coaching
Your PanOptix patient will depend on you to guide them through the post-op period. Remind your patient that, due to the necessary neuroadaptation, they will continue to see subtle improvements in their vision over time. We have noticed a tendency for relatively poor vision at the one-day exam despite an absence of any vision-limiting issues, which generally recovers by the one-week mark.
As with all multifocal IOLs, the PanOptix performs best with a good tear film, so you may need to recommend frequent instillation of non-preserved artificial tears.
The PanOptix also works best when it is well-centered behind the pupil. Small levels of decentration do not appear to significantly diminish the lens power. However, if the lens is so far decentered that part of its central optic is occluded by the pupil’s edge in bright light, consider calling the surgery center. Unfortunately, there is little a surgeon can do to correct this short of a pupilloplasty or IOL exchange.
If your patient complains of blur, your first step is to rule out an inaccurate refractive outcome, as this accounts for the majority of dissatisfied multifocal patients.14 Refractions may have a somewhat soft endpoint, as the patient is able to simultaneously focus through multiple levels of vergence. The trick is to come out of plus slowly and take the first endpoint that gives 20/20 vision. If refractive error is the problem, the surgical center may consider an exchange or refractive laser.
The PanOptix is highly vulnerable to astigmatism, so if your patient is dissatisfied with their vision and you are noticing astigmatism of 1.00D or greater, consider referring back to the surgeon for a surgical fix—a rotation if the problem is a toric that isn’t situated on its intended axis, or LASIK or limbal relaxing incisions if that makes more sense.15
Many patients will want to know their odds of becoming free of glasses. Spectacle independence post-surgery depends significantly on patient personality and motivation. Still, the results so far have been encouraging. In studies, 67% to 96% of patients who received the PanOptix report never having to wear glasses for any purpose.11,16-18
Final Thoughts
Since their introduction to the market many years ago, multifocal IOLs have steadily improved. We owe it to our patients to learn the benefits, contraindications and clinical care for each new lens. No lens can replicate natural, pre-presbyopic vision, and doctor and patient alike must acknowledge that reality. Still, with its improved range of vision, useful focal points and minimal aberrations, the PanOptix will undoubtedly expand the candidate pool for multifocal IOLs.
Dr. Kuhn-Wilken is a staff optometrist at Pacific Cataract & Laser Institute in Tualatin, OR.
| 1. Kohnen T, Marchini G, Alfonso JF. Innovative trifocal (quadrifocal) presbyopia-correcting IOLs: 1-year outcomes from an international multicenter study. J Cataract Refract Surg. 2020;46:1142-48. 2. Sudhir RR, Dey A, Bhattacharrya S, et al. AcrySof IQ PanOptix intraocular lens versus extended depth of focus intraocular lens and trifocal intraocular lens: a clinical overview. Asia-Pac J of Opthalmol. 2019;8(4):335-49. 3. Fiske DW. Consistency of the factorial structures of personality ratings from different sources. J Abnormal Soc Psychol.1949:44(3):329-44. 4. Rudalevicius P, Lekaviciene R, Auffarth GU, et al. Relations between patient personality and patients’ dissatisfaction after multifocal intraocular lens implantation: clinical study based on the five factor inventory personality evaluation. Eye. 2020;34(4):717-24. 5. Alió JL, Pikkel J, eds. Multifocal intraocular lenses: the art and the practice. Switzerland: Springer International Publishing; 2014. 6. Rosa AM, Miranda AC, Patricio MM, et al. Functional magnetic resonance imaging to assess neuroadaptation to multifocal intraocular lenses. J Cataract Refract Surg. 2017;43:1287-96. 7. Dalton M. Trifocal outperforming other premium lenses. Eyeworld. 2017. www.eyeworld.org/trifocals-outperforming-other-premium-lenses. Accessed October 15, 2020. 8. Mester U, Vaterrodt T, Goes F, et al. Impact of personality characteristics on patient satisfaction after multifocal intraocular lens implantation: results from the “happy patient study.” J Refract Surg. 2014;30(10):674-78. 9. Loicq J, Willet N, Gatinel D. Topography and longitudinal chromatic aberration characterizations of refractive-diffractive multifocal intraocular lenses. J Cataract Refract Surg. 2019;45:1650-59. 10. de Medeiros AL, Motta AFP, Vilar BV, et al. Comparison of visual outcomes after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of an extended depth of focus intraocular lens with a diffractive bifocal intraocular lens. Clin Opthalmol. 2017:11;1911-16. 11. Monaco G, Gari M, Di Censo F, et al. Visual performance after bilateral implantation of 2 new presbyopia-correcting intraocular lenses: Trifocal versus extended range of vision. J Cataract Refract Surg. 2017;43(6):737-47. 12. Ruiz-Mesa R, Abengózar-Vela A, Ruiz-Santos M. A comparative study of the visual outcomes between a new trifocal and an extended depth of focus intraocular lens. European J Ophthalmol. 2018;28(2):182-87. 13. Cochener B, Boutillier G, Lamard M, et al. A comparative evaluation of a new generation of diffractive trifocal and extended depth of focus intraocular lenses. J Refract Surg. 2018;34(8):507-14. 14. De Vries NE, Webers CAB, Touwslager WRH. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011; 37:859-65. 15. Carones F. Residual astigmatism threshold and patient satisfaction with bifocal, trifocal, and extended range of vision intraocular lenses. Open J Ophthalmol. 2017;7:1-7. 16. Mencucci R, Favuzza E, Caporossi O, et al. Comparative analysis of visual outcomes, reading skills, contrast sensitivity, and patient satisfaction with two models of trifocal diffractive intraocular lenses and an extended range of vision intraocular lens. Graefe’s Arch Clin Exper Ophthalmol. 2018;256:L1913-22. 17. Kohnen T, Herzog M, Hemkeppler E, et al. Visual performance of a quadrifocal (trifocal) intraocular lens following removal of the crystalline lens. Am Journal of Ophthalmol. 2017;12:52-62. 18. Singh B, Sharma S, Dadia S, et al. Comparative evaluation of visual outcomes after bilateral implantation of a diffractive trifocal intraocular lens and an extended depth of focus intraocular lens. Eye Contact Lens. 2020;46(5):314-18. |