 |
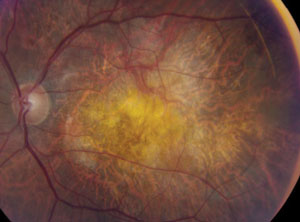
A low BCVA in addition to the presence of IRF could indicate a risk of subretinal fibrosis. Photo: Mark T. Dunbar, OD. Click image to enlarge. |
Early diagnosis of eyes with neovascular AMD (nAMD) at risk of subretinal fibrosis development is key to timely intervention and effective therapy. Diagnostic markers would allow for risk stratification in treatment-naïve eyes, but reliable predictors for the condition’s development are lacking. Moreover, the diagnosis of subretinal fibrosis is challenging because interpretation of current gold-standard imaging modalities such as color fundus photography (CFP) and fluorescein angiography (FA) is inherently subjective. Even on high-resolution spectral-domain optical coherence tomography (SD-OCT), diagnosis is not straightforward.
Researchers in Vienna, Austria, have determined that the presence of a subretinal macular neovascular component, intraretinal fluid (IRF) and shiny hyperreflective material on SD-OCT and low baseline best-corrected visual acuity (BCVA) are easily identifiable parameters indicating an increased risk for subretinal fibrosis in treatment-naïve nAMD eyes.
The study enrolled 45 eyes of 45 participants with treatment-naïve nAMD and treated them according to a standardized treat-and-extend protocol. SD-OCT, CFP and FA, as well as novel imaging modalities OCT and OCT angiography (OCT-A), were performed to detect subretinal fibrosis after one year and find baseline predictors for subretinal fibrosis development.
Baseline OCT-A scans were evaluated for quantitative features such as lesion area, vessel area, vessel junctions, vessel length, vessel endpoints and mean lacunarity. The study found no quantitative baseline microvascular predictors for subretinal fibrosis. After 12 months, eight eyes (18%) developed subretinal fibrosis. Eyes with subretinal fibrosis had worse baseline BCVA and a higher prevalence of IRF and shiny hyperreflective material at baseline.
“Confirming previous observations, we found that a subretinal lesion component (type 2 or mixed-type macular neovascularization) is more common in eyes with subretinal fibrosis development, which may suggest that not the microvascular structure but the location of the macular neovascularization complex (sub-retinal pigment epithelium vs. subretinal) may be more critical for the condition’s development,” the researchers noted.
Roberts PK, Schranz M, Motschi A, et al. Baseline predictors for subretinal fibrosis in neovascular age-related macular degeneration. Sci Rep. 2022;12(1):88. |

