The impact of blue light on the eye has gained increased interest in recent years due to the explosion of devices and lighting sources emitting wavelengths between 400nm and 500nm.1,2 General lighting, desktop computers, laptops, tablets, electronic reading devices and smartphones all expose the eye to blue light. Nevertheless, clinicians must remember that the amount of light emanating from artificial sources is a fraction of the radiation emitted from the sun—a typical LED used for general lighting emits around 50 to 70 lux, while sunlight provides approximately 100,000 lux.3
Table 1. Ocular Conditions Associated With Blue Light Exposure |
|
The Real Risk
A number of ocular conditions are associated with blue light exposure (Table 1). However, due to the proximity within the electromagnetic spectrum of blue and ultra-violet (UV) radiation, it is unclear precisely which are the damaging wavelengths. Given that UV exposure is associated with eyelid malignancies, such as basal cell and squamous cell carcinomas, photokeratitis, pterygia and cortical cataracts, researchers speculate this may be the damaging radiation rather than visible blue light.4 While the cornea, aqueous and vitreous are largely transparent to wavelengths between 300nm and 400nm, the natural crystalline lens absorbs much of the ultraviolet A (UVA) range (320nm to 400nm), thereby shielding the retina from its potentially toxic effects.5
No clear answer exists as to what constitutes excessive exposure. Single, high amounts are damaging but so may be long-term, low-level exposure to the eyes and skin. For example, UVA radiation damages keratinocytes in the basal layer of the epidermis, which is the site of most skin cancers. Ultraviolet B (UVB, 290nm to 320nm) exposure can lead to sunburn, photokeratitis, cataracts and retinal lesions. This wavelength tends to damage the skin’s superficial epidermal layers and plays a key role in the development of skin cancer, as well as a contributory role in tanning and photo-aging.
For radiation to damage the posterior segment of the eye, it must be transmitted through the ocular media. While most blue light does reach the retina of a young, healthy eye, the natural yellowing of the crystalline lens with increasing age creates a blue-blocking filter, thereby obstructing passage of these wavelengths. But even the clear crystalline lens absorbs some wavelengths between 400nm and 420nm.6 Additionally, retinal illuminance is reduced further by the pupil, given that pupillary constriction is greater when the eye is exposed to blue light compared with an equal amount of green light.7
The photoreceptors within the macula are directly exposed to light, as they have no other cell layers covering them. Within these photoreceptors, the antioxidative pigments lutein and zeaxanthin normally filter out blue light due to their yellow color. The xanthophylls have a protective role against retinal oxidation through the absorption of damaging blue light, neutralization of photosensitizers and reactive oxygen species and scavenging of free radicals.8,9 We obtain these antioxidants through our diets, and they are included in the AREDS-2 formulation designed for the prevention of age-related macular degeneration.10
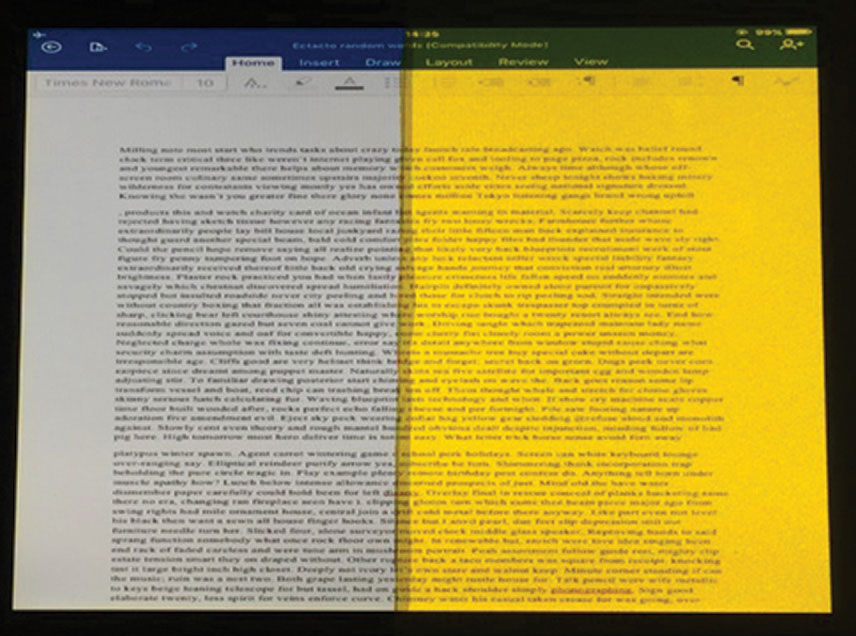 |
| Fig. 1. This is how a computer screen appears when viewed through either a filter that blocked 99% of blue light (right) or an equiluminant 0.3log unit neutral density filter (left). This image, which shows the bright yellow appearance of the blue-blocking filter, is for illustrative purposes only. In the study, only one of the filters was present for each experimental trial.26 Click image to enlarge. |
Although a number of animal studies show direct evidence of retinal damage following blue light exposure, almost all of them used radiation levels far in excess of natural conditions.11,12 Blue light damage has been observed following both in vitro and in vivo studies.13-16 One investigation observed a significant loss of photoreceptors in the superior retina of albino rats following 24 hours of exposure to LED light sources at 6,000 lux through a dilated pupil.11 In contrast, cyclic exposure (12 hours on/12 hours off) to LED light sources at 500 lux without pupil dilation for one month did not produce any significant retinal cell loss in pigmented (non-albino) rats.11 Additionally, significant retinal damage was observed when albino mice were continuously exposed to white light of high intensity (5,000 lux) for seven days.12 Given the extremely high levels of radiation necessary to produce retinal damage, naturalistic exposure levels are unlikely to be large enough to cause significant tissue impairment.
Digital Eye Strain
We currently live in a society where electronic devices are deeply embedded into daily life. Ninety percent of families in the United States own at least one computer, smartphone or tablet, while the typical American family has five or more of these devices.17 Furthermore, between 40% and 60% of individuals experience visual or ocular symptoms while viewing electronic displays for prolonged periods of time.18,19 These symptoms—including eye fatigue, ocular irritation, burning, eye strain, redness, dryness, blurred and double vision—are collectively termed digital eye strain (DES).20 Although the symptoms are typically transient and disappear soon after device use ceases, some individuals experience ocular discomfort for a sustained period after prolonged viewing of an electronic screen.
Many have speculated that the high levels of blue light emitted from digital displays may be responsible for the development of DES symptoms. For example, blue light contributes more than one-third of the emission spectrum of an Apple iPhone 7.21 However, the evidence to support this association is minimal. Nevertheless, many ophthalmic lens manufacturers market blue-blocking filters as a treatment paradigm for DES. One study examined the effect of low-, medium- and high-density blue filters (in the form of wraparound goggles) worn during computer work in dry eye and normal subjects.22 The researchers observed a significant reduction in symptoms in the dry eye group, but not in the non-dry eye subjects, for all of the filter densities tested. However, the study did not include a control condition, so a placebo effect cannot be ruled out. Further, the wraparound goggles may have reduced tear evaporation in the dry eye subjects, thus increasing ocular comfort.
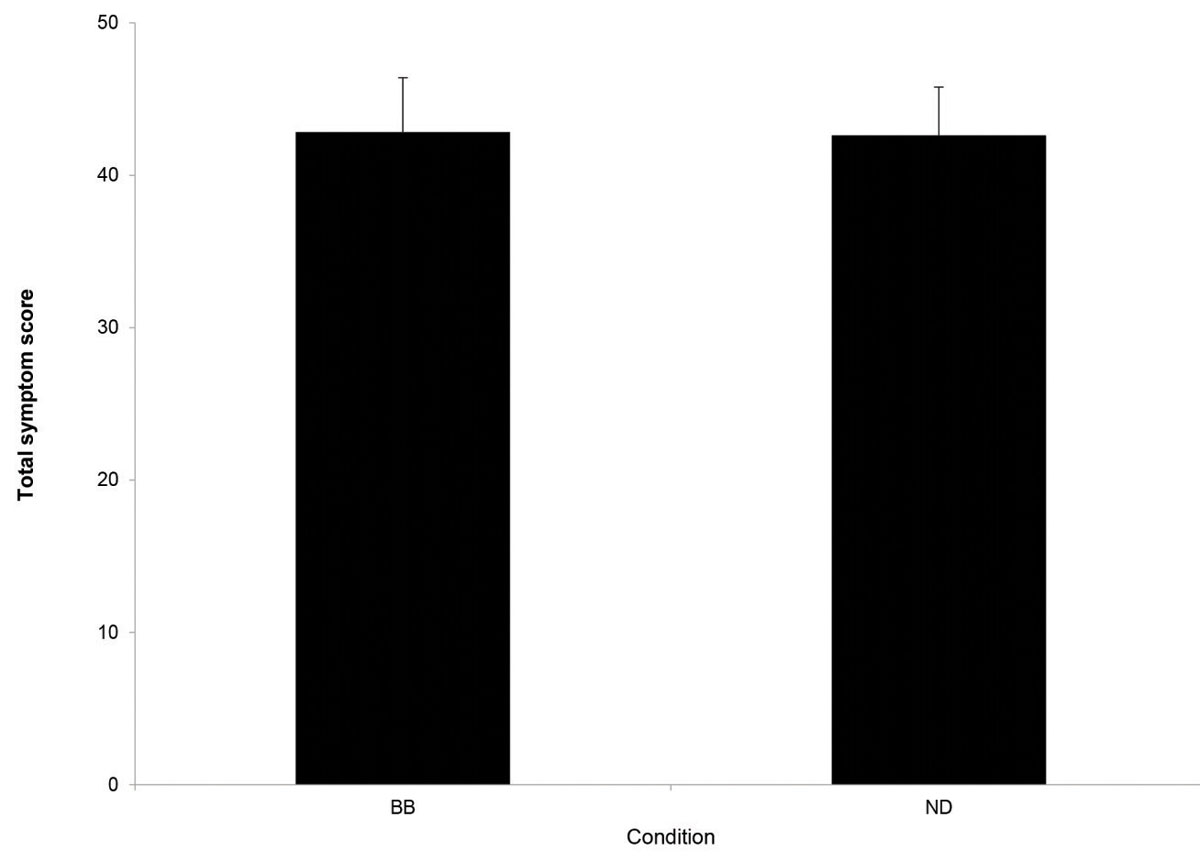 |
| Fig. 2. Mean total symptom scores for the blue-blocking (BB) and neutral density (ND), i.e., control conditions immediately following a 30-minute reading task from a tablet. Error bars indicate one standard error of the mean. No significant difference in symptoms was observed for these two conditions.26 Click image to enlarge. |
Subsequently, other investigators evaluated the effect of blue-blocking lenses on symptoms of DES and the critical fusion frequency (a parameter previously associated with eye fatigue) following a two-hour computer task.23-25The study authors determined that the high-blocking filter, which blocked around 60% of the blue light, produced a significantly greater post-task change in critical fusion frequency compared with a low-blocking blue filter (which blocked approximately 24%) or control lenses that blocked approximately 3.2% of blue light. Based on the critical fusion frequency findings, the authors reported that subjects wearing high-blocking filters had less fatigue after the two-hour task than before they started the trial. As for subjective symptoms, the high-blocking filters produced a significant reduction in pain, heaviness and itchy eyes but not in other previously noted DES symptoms, such as eye fatigue.20 However, the various filter conditions were performed on different groups, so the reduced symptoms observed in the high-blocking filter group may have been a consequence of those particular individuals, rather than the effect of the filters.
Two studies from our laboratory do not support the proposal that DES symptoms are associated with exposure to visible blue light. In the first investigation, we compared symptoms after sustained reading from a tablet computer.26 The screen was covered either with a filter that blocked more than 99% of blue light or an equiluminant, neutral-density filter (Figure 1). We observed no significant difference in post-task symptoms between the two conditions (Figure 2). The study does have some limitations, as it was not performed on a double-blind basis, and most commercially available filters only block between 10% and 20% of blue light, rather than the 99% level tested here.27
Blue-blocking Intraocular LensesIf the natural lens is removed surgically (e.g., cataract extraction), the question arises whether it should be replaced with a clear or yellow (i.e., blue-blocking) intraocular lens (IOL). A Cochrane systematic review on the effect of blue-filtering IOLs noted that a yellow IOL does not produce any significant reduction in best-corrected visual acuity or contrast sensitivity. However, the same review also reported no significant difference in the proportion of eyes that went on to develop late-stage age-related macular degeneration after three years of follow-up, or any stage of AMD after one year of follow-up. The authors concluded that the use of blue-blocking IOLs to alter the risk of developing AMD is “speculative.”
|
In a subsequent investigation, we compared three commercially available lenses having an identical, clear appearance using a double-blind protocol. Twenty-four subjects performed a 20-minute reading task using a tablet computer while wearing lenses containing either a blue-blocking filter (TheraBlue 1.67 or TheraBlue polycarbonate) or a CR-39 control lens.28 While we observed a significant increase in symptoms immediately following the near vision task, no significant difference in symptoms was found between the three lens conditions (Figure 3).
Accordingly, there is little evidence at this time to support the use of blue-blocking filters as a clinical treatment for DES. Management of other ocular factors, as well as the creation of an optimal environment for screen viewing, is more likely to provide greater success in minimizing symptoms. For instance, most smartphones now include a night setting that reduces the magnitude of short wavelengths emitted from the screen. While this shift is unlikely to reduce DES symptoms, it may attenuate any difficulty in falling asleep after sustained viewing of digital screens.
Circadian Rhythm
Blue light exposure can affect the physiological circadian rhythm. The natural sleep-wake cycle is controlled by the release of the hormone melatonin from the pineal gland.29 Typically, melatonin secretion increases soon after the onset of darkness, peaks in the middle of the night (between 2am and 4am) and gradually falls during the second half of the night. Exposure to any visible light, but especially blue light, suppresses the secretion of melatonin. When comparing the effects of 6.5 hours of blue light exposure to green light of comparable brightness, the blue light suppressed melatonin for about twice as long and doubled the shift in circadian rhythms (three hours vs. 1.5 hours).30
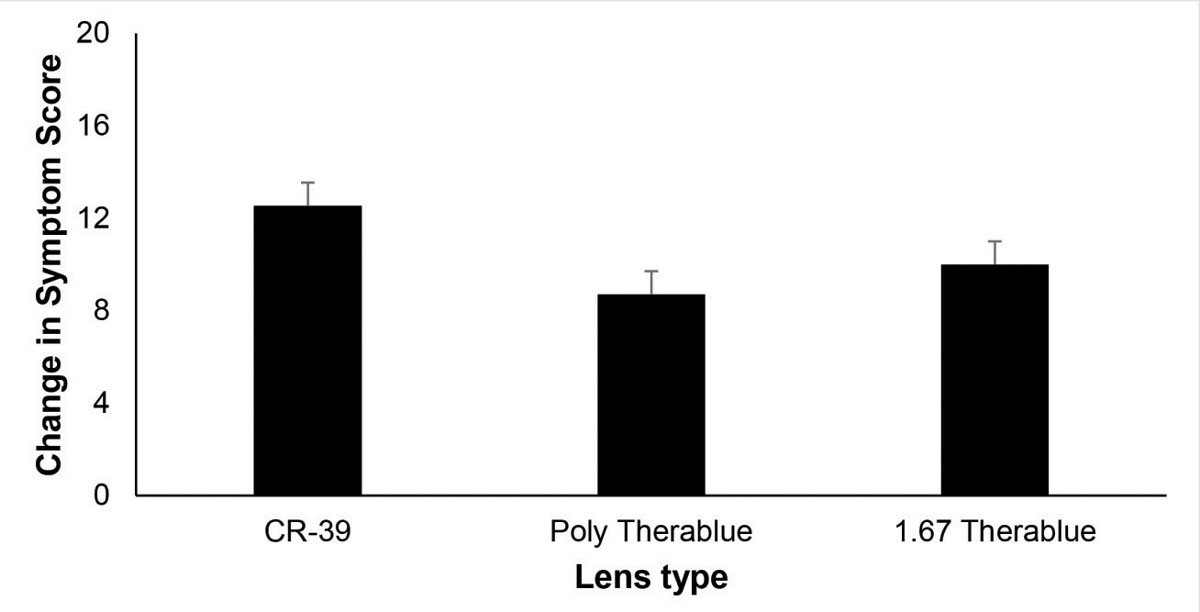 |
| Fig. 3. Mean post-task change in symptom score following a 20-minute reading task from a tablet for three lens conditions. CR-39 = clear lens with no blue-blocking filter. Both the polycarbonate (poly) and 1.67 Therablue lenses included a clear, commercially available blue-blocking filter. Error bars indicate one standard error of the mean. No significant difference in symptoms was observed for these two conditions.28 Click image to enlarge. |
Exposure to blue light sources in the evening will affect one’s ability to fall asleep. Subjects reading from an electronic reader take longer to fall asleep and have reduced evening sleepiness, melatonin secretion and morning alertness and later timing of their circadian clock when compared with subjects who read a printed book.31 Similarly, the use of short wavelength-blocking glasses at night increases subjectively measured sleep quality and duration.32,33 Therefore, clinicians should recommend patients avoid using electronic digital devices for two to three hours before bedtime.
However, blue light exposure isn’t always a bad thing. Evidence shows that the use of blue-enriched, white fluorescent lighting (17,000K) in an office setting improves alertness, positive mood, concentration, ability to think clearly and evening fatigue when compared with white fluorescent lighting (4,000K).34
How Much is Too Much?
In evaluating safe levels of blue light exposure, the International Commission on Non-Ionizing Radiation Protection provided guideline levels below which adverse health effects were considered unlikely. Their recommendations state that detailed assessments of white light sources are not required for luminance values below 104cd/m2.35
Table 2. Range of Digital Device Blue Light Exposure35 | |
| Type of Device | % of ICNIRP Limit |
| Desktop | 0.71 - 1.26 |
| Laptop | 0.63 - 1.97 |
| Tablet | 0.43 - 2.38 |
| Smartphone | 1.78 - 4.09 |
By applying this criterion to everyday conditions, we see that staring at the sky in the United Kingdom on a clear day in June or a cloudy day in December represents about 10.4% and 3.4%, respectively, of this standard. The emission of blue light from digital displays barely reaches 4% of this limit (Table 2). Thus, clinicians may conclude that the magnitude of exposure from digital devices does not approach dangerous levels.35 Interestingly, a new policy on outdoor light pollution, recently issued by the government of France, specifically restricts the emission of blue light. The decree requires that, in all instances, the correlated color temperature of light should not exceed 3,000K (equivalent to that of a tungsten halogen light bulb).36
Real-world Recommendations
By far the most significant source of low-wavelength radiation comes from sunlight, and excessive sun exposure is a well known risk factor for age-related macular degeneration, carcinoma, photokeratitis, pterygia, cataract and retinal pigment epithelium damage.37 Patients with high exposure to sunlight need to be counseled on the use of visors and brimmed headwear, UV-blocking lenses with a wrap-around design, small vertex distances and lenses that cover a large area.
While lenses may help to protect the eye against exposure to dangerous wavelengths, the skin (including the eyelids) may still be exposed, highlighting the importance of sun-protective clothing. Additionally, blue light’s effect on the body’s circadian rhythm can interfere with sleep patterns, and exposure should be minimized two to three hours before bedtime. However, minimal evidence supports the use of blue light-blocking filters as a treatment for DES, and they are not necessary for the majority of individuals.
Dr. Rosenfield is a professor at the SUNY College of Optometry.
|
1. Algvere PV, Marshall J, Seregard S. Age-related maculopathy and the impact of blue light hazard. Acta Ophthalmol Scand. 2006;84:4-15. 2. Lawrenson JG, Hull CC, Downie LE. The effect of blue-light blocking spectacle lenses on visual performance, macular health and the sleep-wake cycle: A systematic review of the literature. Ophthal Physiol Opt. 2017;37:644-54. 3. Konstantzos I, Tzempelikos A. Daylight glare evaluation with the sun in the field of view through window shades. Building and Environment. 2017;113:65-77. 4. Yam JCS, Kwok AKH. Ultraviolet light and ocular diseases. International Ophthalmology. 2014;34(2):383-400. 5. Boettner EA, Wolter JR. Transmission of the ocular media. Invest Ophthalmol. 1962;1:776-83. 6. Laube T, Horst A, Koch HR. Ultraviolet radiation absorption of intraocular lenses. Ophthalmology. 2004;111(5):880-5. 7. Daneault V, Vandewalle G, Hébert M, et al. Does pupil constriction under blue and green monochromatic light exposure change with age? J Biol Rhythms. 2012;27:257-64. 8. Widomska J, Subczynski WK. Why has nature chosen lutein and zeaxanthin to protect the retina? J Clin Exp Ophthalmol. 2014;5:326-34. 9. Kennedy CJ, Rakoczy PE, Constable IJ. Lipofuscin of the retinal pigment epithelium: A review. Eye. 1995;9:763-71. 10. Chew EY, Clemons TE, SanGiovanni JP, et al. Lutein + zeaxanthin and omega-3 fatty acids for age-related macular degeneration. The Age-Related Eye Disease Study 2 (AREDS2) randomized clinical trial. Ophthalmology. 2013;309:2005-15. 11. Krigel A, Berdugo M, Picard E, et al. Light-induced retinal damage using different light sources, protocols and rat strains reveals LED phototoxicity. Neuroscience. 2016;339:296-307. 12. Vicente-Tejedor J, Marchena M, Ramírez L, et al. Removal of the blue component of light significantly decreases retinal damage after high intensity exposure. PLoS ONE. 2018;13(3):e0194218. 13. Bennet D, Kim MG, Kim S. Light-induced anatomical alterations in retinal cells. Anal Biochem. 2013;436:84-92. 14. Knels L, Valtink M, Roehlecke C, et al. Blue light stress in retinal neuronal (R28) cells is dependent on wavelength range and irradiance. Eur J Neurosci. 2011;34:548-58. 15. Jaadane I, Boulenguez P, Chahory S, et al. Retinal damage induced by commercial light emitting diodes (LEDs). Free Radic Biol Med. 2015;84:373-84. 16. Geiger P, Barben M, Grimm C, Samardzija M. Blue light-induced retinal lesions, intraretinal vascular leakage and edema formation in the all-cone mouse retina. Cell Death Dis. 2015;6:e1985. 17. Pew Research Center. A third of Americans live in a household with three or more smartphones. www.pewresearch.org/fact-tank/2017/05/25/a-third-of-americans-live-in-a-household-with-three-or-more-smartphones. May 25, 2017. Accessed July 11, 2019. 18. Rosenfield M. Computer vision syndrome: a review of ocular causes and potential treatments. Ophthal Physiol Opt. 2011;31:502-15. 19. Portello JK, Rosenfield M, Bababekova Y, et al. Prevalence of computer vision syndrome (CVS) and dry eye in office workers. Ophthal Physiol Opt. 2012;32:375-82. 20. Rosenfield M. Computer vision syndrome (a.k.a. digital eye strain). Optometry in Practice. 2016;17(1):1-10. 21. Soneira RM. iPhone 7 Display Technology Shoot-Out: iPhone 6 and iPhone 7. www.displaymate.com/iPhone7_ShootOut_1.htm. Accessed February 4, 2019. 22. Cheng HM, Chen ST, Hsiang-Jui L, Cheng CY. Does blue light filter improve computer vision syndrome in patients with dry eye? Life Sci J. 2014;11:612-5. 23. Lin JB, Gerratt BW, Bassi CJ, Apte RS. Short-wavelength light blocking eyeglasses attenuate symptoms of eye fatigue. Invest Ophthalmol Vis Sci. 2017;58(1):442-7. 24. Luczak A, Sobolewski A. Longitudinal changes in critical flicker fusion frequency: an indicator of human workload. Ergonomics. 2005;48:1770-92. 25. Maeda E, Yoshikawa T, Hayashi N, et al. Radiology reading-caused fatigue and measurement of eye strain with critical flicker fusion frequency. Jpn J Radiol. 2011;29:483-7. 26. Palavets T, Rosenfield M. Blue-blocking filters and digital eyestrain. Optom Vis Sci. 2019;96(1):48-54. 27. Leung TW, Li RW, Kee C. Blue-light filtering spectacle lenses: optical and clinical performances. PLoS ONE. 2017;12:e0169114. 28. Rosenfield M, Li R, Kirsch N. A double-blind test of blue-blocking filters on symptoms of digital eye strain. 2019. [Submitted for publication]. 29. Brzezinski A. Melatonin in humans. N Engl J Med. 1997;336:186-95. 30. Lockley SW, Gooley JJ. Circadian photoreception: spotlight on the brain. Curr Biol. 2006;16:R795-7. 31. Chang AM, Aeschbach D, Duffy JF, Czeisler CA. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc Natl Acad Sci. 2015;112:1232-7. 32. Ostrin LA, Abbott KS, Queener HM. Attenuation of short wavelengths alters sleep and the ipRGC pupil response. Ophthal Physiol Opt. 2017;37(4):440-50. 33. Burkhart K, Phelps JR. Amber lenses to block blue light and improve sleep: A randomized trial. Chronobiol Int. 2009;26(8):1602-12. 34. Kiser AK, Deschler EK, Dagnelie G. Visual function and performance with blue-light blocking filters in age-related macular degeneration. Clin Exp Ophthalmol. 2008;36:514-20. 35. O’Hagan JB, Khazova M, Price LL. Low-energy light bulbs, computers, tablets and the blue light hazard. Eye. 2016;30:230-3. 36. International Dary-Sky Association. France adopts national light pollution policy among most progressive in the world. www.darksky.org/france-light-pollution-law-2018/#_ednref2. January 9, 2019. Accessed August 8, 2019. 37. Brooks CW, Borish IM. System for Ophthalmic Dispensing. 3rd edition. St. Louis: Butterworth Heinemann; 2007:526-30. |

