Vision CareCheck out the other feature articles in this month's issue: -Where Does Vision Care Fit in 2021? |
Over the last several decades, there has been a dramatic increase in screen time exposure among children. Infants and children up to age five are exposed to more than three hours a day of screen time. Teenagers spend anywhere from five to seven hours per day using screens beyond the demands of school.1-3 When the COVID-19 pandemic struck, many children were forced to leave their physical classrooms to begin to learn remotely from home, adding even more daily screen exposure.
With the increase in screen time possible during the pandemic, many patients may inquire about the negative effects that the screens of their personal devices may have on their eyes and health. This article will highlight how digital screens affect the visual system and pediatric development, and will offer recommendations you can provide for your patients.
As Far as the Light Reaches
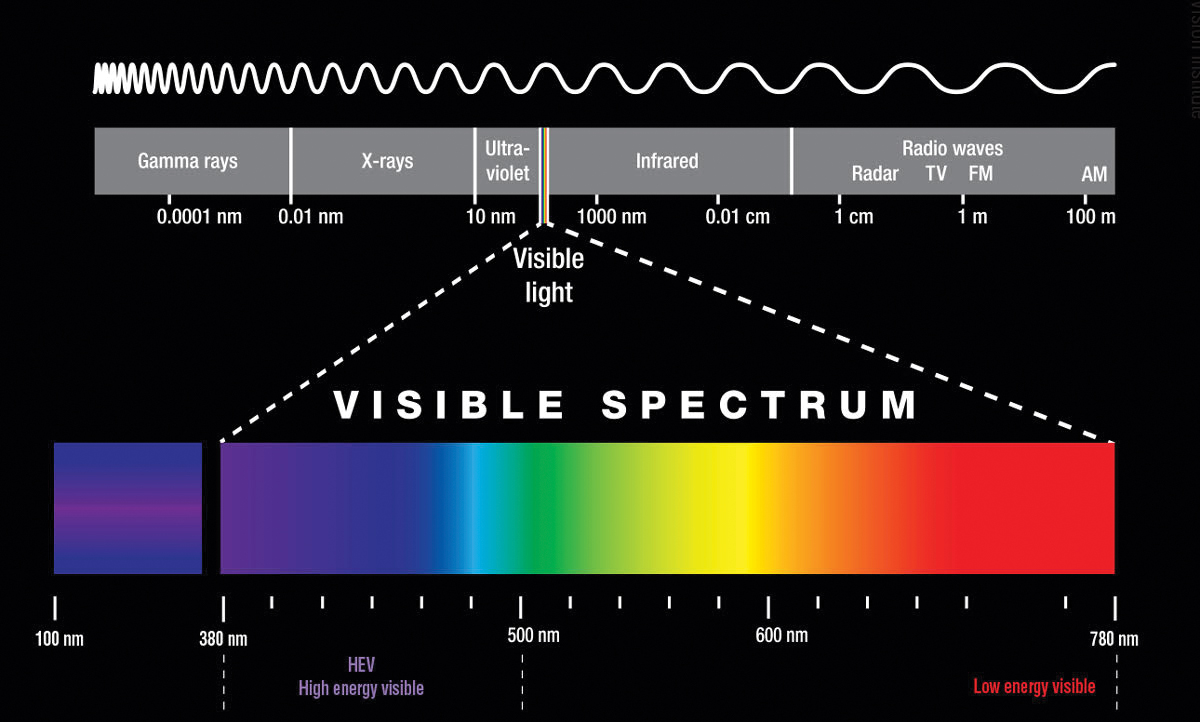
One of patients’ largest concerns is whether the light emitted from screens will physically damage their eyes. Unfortunately, marketing and soft science have muddled our conversations about screen time and blue light exposure. The light emitted from screens contains relatively high amounts of visible blue light, which has a short wavelength and high energy. Unlike even higher energy ultraviolet light, visible blue light can pass through the cornea and the crystalline lens to reach the retina.In vitro studies provide insight into the effects of blue light incident upon the retina. Most of the blue light is absorbed by the retinal pigment epithelium (RPE), causing the release of reactive oxygen species, which damage lipid membranes, denature proteins and alter DNA.4-7 Thus, it is not surprising that many laboratory-based studies on cultured retinal cells have demonstrated that long-duration exposures to bright blue light leads to the death of RPE cells and photoreceptors.8
When interpreted in a vacuum, these results from the bench point toward potentially damaging effects of blue light exposure. Fortunately for patients, results from large epidemiological studies looking at the effect that sunlight has on retinal diseases including age-related macular degeneration (AMD) do not directly parallel the results from laboratory-based studies.9-11 Like the screens of personal electronic devices, sunlight contains high levels of visible blue light. Although some studies suggest a link between sunlight exposure and the development and progression of AMD, the preponderance of evidence suggests that sunlight exposure is not a risk factor for AMD.12-16 Protective elements inherent in the intact eye, such as macular pigment, melanin and the crystalline lens, likely account for this difference by either absorbing high-energy light or by neutralizing reactive oxygen species.17-20
The effect that age has on this protection remains unelucidated. Although the aging lens filters out more short-wavelength light than the relatively young lens, large investigations suggest that recent sunlight exposure is a larger risk than cumulative light exposure for the advancement of AMD. More research is needed to provide a clearer picture.21
If sunlight exposure is not clearly linked to AMD, then light emitted from screens is not likely to damage the retina either. The reason is that light emitted from personal electronic devices is substantially dimmer than sunlight. For example, a dreary, cloudy afternoon is over 10 times brighter than the brightest setting on current personal devices, and a nice, sunny afternoon is over 100 times brighter.22,23
Simply put, the light emitted from screens of personal electronic devices is not bright enough to damage the retina.24 A recent publication investigating the theoretical blue light hazard of using screens concluded that light from screens pose a minimal risk to damage the retina because they are so dim.25
 |
|
Within the visible light spectrum, short wavelengths, such as violet and blue, reach the retina and are higher energy than long wavelengths, such as orange and red. Image: Adapted with permission from Essilor. Click image to enlarge. |
Developmental Concerns
Nevertheless, there is growing evidence that increases in screen time can be harmful to physical, cognitive and social development in children.
As kids spend more time using screens, either for recreation or for school, they spend less time being physically active. A child’s likelihood of being overweight or obese grows as their screen time increases. One study noted the likelihood of being overweight or obese rose as “screen time” increased due to watching TV, playing video games and using a computer as well as that the prevalence of overweight and obesity combined has more than doubled among youth aged 12 to 17 over the last 25 years in Canada.26 Another found watching TV was an independent predictor of the change in the child’s BMI.27 This is a growing concern for pediatricians, as they worry about the secondary effects that obesity will have on the overall health of their patients.
It is important for children to reach developmental milestones appropriately and on time. Reaching milestones as expected gives insight into a child’s developmental health. Evidence suggests that increased use of screen time can be linked to developmental delay. One of the important milestones children are expected to meet is developing expressive speech. It appears that mobile media use in 18-month-old children is linked to expressive language delay. Specifically, each 30-minute increase in daily mobile media device use was associated with an increased odds of parent-reported speech delay.28
A way to assess if a child is meeting a broad range of developmental milestones is to administer the Ages and Stages Questionnaire, a widely used parent-reported screening measure of five domains: communication, gross motor, fine motor, problem solving and personal-social. It has been shown that greater amounts of screen time use is predictive in how a child will perform on the Ages and Stages Questionnaire. For example, more screen time use at 24 months of age was associated with poorer performance on the questionnaire at 36 months, and similarly, more screen time use at 36 months was associated with lower scores on developmental testing at 60 months of age.29 If children demonstrate significant delays, it is important that patients are referred properly to receive proper diagnoses and treatment if necessary.
 |
|
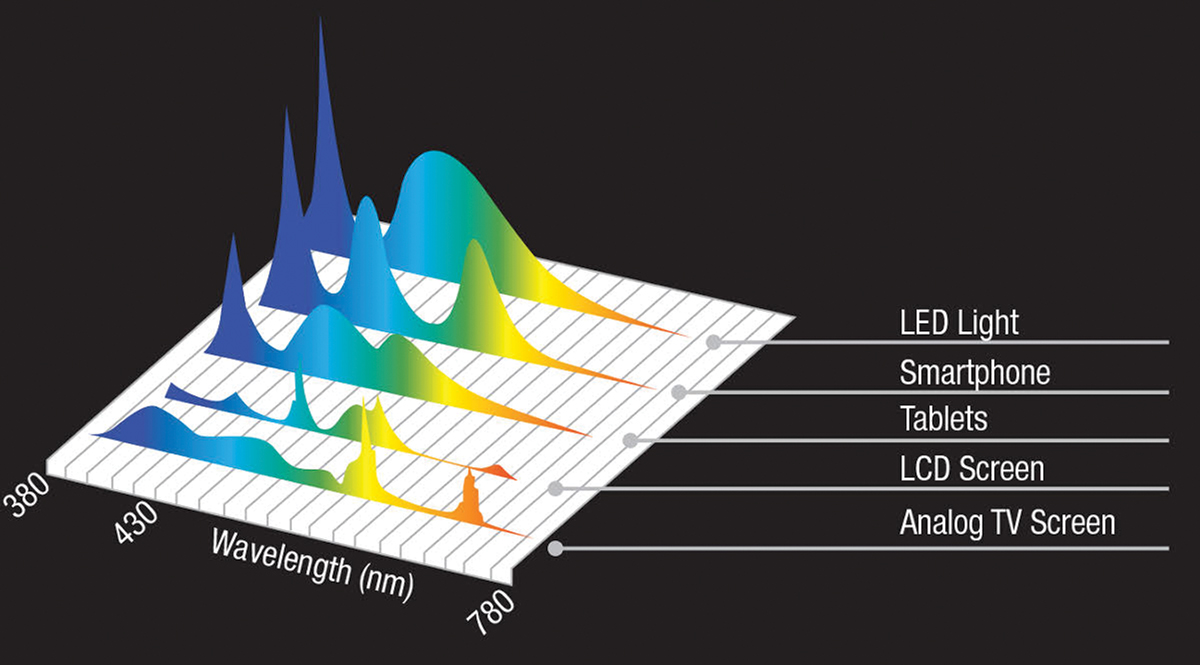
Modern, LED-based screens commonly found on smartphones and tablets contain more short-wavelength light than other wavelengths. Older technologies, such as LCD and analog screens, have less relative blue light than newer technologies. Image: Adapted with permission from Essilor. Click image to enlarge. |
There is growing evidence that screen time use is linked with worse psychological well-being. In fact, 14- to 17-year old adolescents who spend seven or more hours per day using screens are two times more likely to be diagnosed with anxiety or depression and are 1.5 times more likely to be diagnosed with anxiety or depression if they spend at least four hours per day using screens.32
Beyond diagnoses of anxiety and depression, teenagers report having less curiosity, less self-control, more distractibility, more difficulty making friends, less emotional stability and inability to finish tasks.
Oftentimes we hear claims that near work causes myopia, based on studies that found that children who did more near work were more likely to develop nearsightedness. Because of these findings, we often hear parents concerned that near work, computer, phone and tablet use is going to cause their child to become nearsighted. It is important to note that in larger scale, longitudinal studies (which are better for making causative claims), associations between near work and the development of myopia are weak at best.
More importantly, research suggests that time outdoors may play a larger role in the development of myopia. Studies show that children who spend more time outdoors are less likely to become nearsighted.33-36 Specifically, children who spent about 14 hours per week outdoors were the least likely to become nearsighted, which may feel impossible to accomplish while students are required to learn remotely during the COVID-19 pandemic.
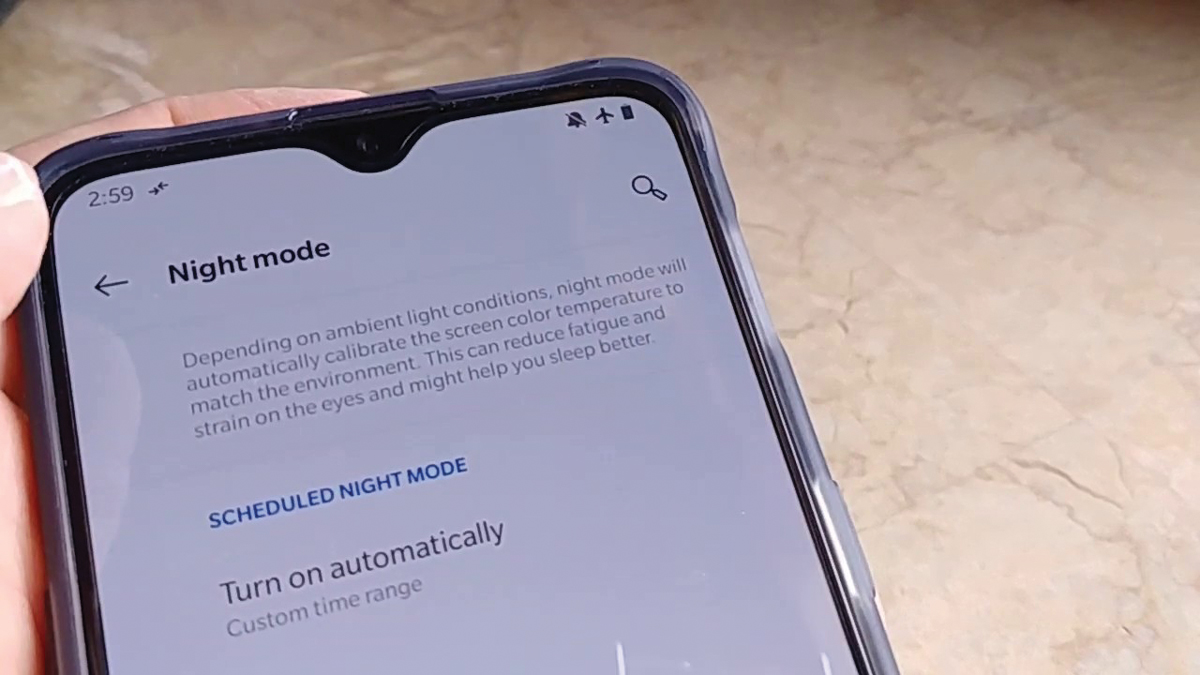 |
Nighttime filters can help patients reduce the overall screen brightness before bed. Click image to enlarge. |
Impact on Sleep and Vision
Just because light emitted from the screens of personal electronic devices likely does not damage the eye, it does not mean that it is innocuous. Every day, human beings must entrain their circadian rhythms to the solar cycle. Light detection by the eyes is the principal method of this alignment. So, using screens before bed has the potential to trick the body’s master clock into acting as if it were still daytime. As a result, the complex mechanism of sleep induction is delayed, total sleep time is reduced and rejuvenating rapid eye movement (REM) sleep is compromised.32,37 These effects on sleep have considerable effects on the well-being of patients. Patients who use personal electronic devices before bed often feel more tired the next day and have decreased brain activity compared to patients who do not use them.36
The mechanisms behind sleep and alertness are complex, but light-mediated melatonin suppression may play a substantial role in these effects.38 During the pandemic, school-aged children who are participating in remote learning, and high schoolers in particular, fall into this vicious cycle. They wake up and soon turn on their computers for class. After, they spend their free time on social media because there are limited options for in-person interaction. Thus, it is important for optometrists to inquire about this behavior so that they may educate their patients on better screen habits.
Finally, it has been our experience that, since the start of the pandemic, complaints about visual discomfort from computer use have skyrocketed. Digital eyestrain, also known as computer vision syndrome, occurs when the visual demands of prolonged screen time cause symptoms of eyestrain, headaches, blurred vision and eye irritation. The etiology of digital eyestrain is complex and can be difficult to isolate, as disorders of binocular vision and dry eye can present with similar symptoms. Convergence insufficiency, accommodative insufficiency or infacility, as well as other problems with near work can certainly be the underlying cause of digital eyestrain—but do not forget about the ocular surface.
Blink rate is known to drop from about 12 blinks per minute during distance viewing to about six blinks per minute during near work.39 This reduction in blinks can cause the tears to evaporate, leading to a dried out, inflamed ocular surface. Making patients aware of this phenomenon helps assure them that their symptoms are normal. Remind patients to make sure they take breaks to relax their visual system. Providing a reason for their symptoms empowers them to take the necessary steps to address it.
In a recent publication, researchers urged using caution when making sweeping assumptions about the negative effects of screen use often published in the literature. Many studies provide highly powered investigations where many variables and observations are justified with a flexible analysis that can create statistically significant findings that may not translate into significant clinical findings.40 Optometrists can educate their patients on the difference between a statistically significant finding in a research paper and a clinically significant one.
Considering the potentially negative effects of screen use is important, but it should be noted that there are benefits to screen time. In young children, programming often viewed on screens can help improve literacy skills, numeracy skills and social skills. In older children, programming can improve problem solving and critical thinking skills as well as provide educational, social, and creative benefits.32 For teenagers, screen use can improve reading, writing, social connections, and political and social awareness, help instill personal values, create new creative forms, and promote self-expression.32
Recommendations for Safe Use of Digital Screens in KidsFrom the World Health Organization: One year and younger: no screen time One to two years old: sedentary screen time not recommended Two to four years old: no more than one hour of sedentary screen time From the American Academy of Pediatrics Younger than 18-24 months: avoid digital media other than video chat 18-24 months: watch digital media with children because they learn from watching and talking with you Ages 2-5: limit screen use to one hour per day Ages 6+: establish consistent limits on time spent and types of media |
How ODs Can Intervene
Optometrists are in a unique position to recommend mitigation strategies for patients who struggle with digital eyestrain or other screen-related ailments. The first step of any intervention plan is to ensure that the patient has accurate, up-to-date spectacle and contact lens prescriptions. It is important to remember to complete a cycloplegic refraction in young patients, as latent hyperopia can often be missed, especially if the patient has accommodative spasm. If patients have asthenopic complaints that are exacerbated with near work, it is important to ensure that there is no underlying binocular vision disorder.
A sensorimotor examination that assesses accommodation, vergence and saccadic function will aide in determining if any underlying binocular vision disorders require treatment. Refractive error correction and a properly functioning binocular vision system are the bedrock of clear and comfortable vision while on electronic devices. If these components of the visual system are disordered, then any additional recommendations are likely to be ineffective.
Appropriate refractive error correction and good binocular vision may not mitigate all symptoms of digital eyestrain. In these instances, consider addressing the patient’s ocular surface, even if the common signs of dry eye disease are not present, as ocular surface inflammation can be subclinical.
A good place to start is recommending the “20-20-20 rule,” which instructs patients to take a 20-second break to view something 20 feet away every 20 minutes. This approach gives the patient a chance to periodically blink and to relax the binocular vision system. Adding a high-quality artificial tear drop with a lipid component to the 20-20-20 rule may provide addition relief by fortifying the eye’s natural tears to stave off evaporation. Instruct the patient to instill the drop before the start of a long computer session, as they may work better to prevent symptoms than to eliminate them once they have started. Keep in mind, people spent less time in front of screens when this rule was first implemented in the 1990s than they do today. If you feel that a child cannot take structured breaks as rigid as the 20-20-20 rule, ensure that they take regular breaks from screens, especially if they also incorporate outdoor time or physical activity.
Some doctors may be inclined to manage the negative effects of screens by eliminating blue light. There is little evidence, however, that blocking blue light with spectacles, especially ones with anti-reflective coatings designed for that purpose, provides much benefit to the patient.41 A recent study found that eliminating blue light from a computer screen does no more to reduce strain and fatigue than simply dimming the screen.42 Although blue light is the most effective part of the visible light spectrum at altering sleep patterns, blocking it with ophthalmic products has not been shown to consistently improve sleep quality. This finding is likely due to the fact that all bright light before bedtime, not just blue light, is capable of negatively impacting sleep, both in duration and quality.43
Although blue-blocking anti-reflective coatings likely provide little benefit, it does not mean that optometrists cannot suggest simple approaches to managing the light emitted from screens.42 Many newer personal electronic devices feature filters for nighttime use that reduce the amount of blue light created by their screens. But all bright visible blue light is able to affect sleep, violet through red. So, more importantly, these filters also cut light from the middle and long wavelengths and reduce the overall brightness of the screen—the main culprit. As a result, these filters are likely more effective at promoting sleep and improving viewing comfort than anti-reflective coatings.44,45 Of course, the best option might be reducing overall screen time and finding other sources of entertainment, especially before bedtime. We frequently recommend to our patients that the bedroom be a “no electronics zone.” If patients absolutely must use screens before bedtime, we stress the need to dim their screens, either manually or through a filter.
When it comes to screen time management, the AAP and World Health Organization (WHO) have provided recommendations for infants and young children. While the WHO places more emphasis on non sedentary screen time, both groups suggest avoiding digital media for children two years and younger unless it is used for video chatting or is high quality programming. In children age two to five, screen time should be limited to one hour per day. In children age six and older, there should be consistent limits on time spent and type of media exposure. The AAP recognizes that the COVID-19 pandemic has forced everyone to use screens at much higher rates and recommends that parents try their best to preserve offline experiences with their children, ensure that their children’s media use is positive and helpful and interact with their children as much as possible when they are enjoying screen media.46 The AAP’s website (www.aap.org) has resources available to set up a family media use plan, which can take into account the health, education and entertainment needs of each child in the household, as well as the family as a whole.
To Sum Up
With the growing use of screens in all walks of life, a balanced approach is of utmost importance. We cannot get rid of our dependence on screens and technology, especially as the COVID-19 pandemic continues. We should advise our patients to counter screen time with activities that minimize screen time use. Spending more time outdoors could help prevent the onset of myopia and encourage non sedentary behavior. Taking breaks from screens could combat anxiety, depression and distracted behavior. Stopping screen time use before bed may help with sleep and possibly improve attention and learning.
It may feel unusual to provide advice for patients that does not immediately appear to be ocular or visual health-related; however, eye care providers are often the first to have discussions with patients regarding the effects of screen time. Having a broad understanding of the effects of screen time may help providers develop a more holistic approach to healthcare while improving the quality of life for our patients.
Dr. Morrison is an instructor at The Ohio State University College of Optometry in Columbus, OH. She is currently working towards a PhD in Vision Science. Her clinical focus is in pediatrics, binocular vision disorders, brain injuries and vision therapy. Dr. Morrison is a consultant for HillRom Vision Screening Board.
Dr. Yuhas is an assistant professor at The Ohio State University College of Optometry. He also practices at Northwest EyeCare Professionals in Upper Arlington, OH. He has no financial disclosures.
1. Chen W, Adler J. Assessment of Screen exposure in young children, 1997 to 2014. 2. The Common Sense Census: Media Use by Tweens and Teens. Common Sense Media,2015. 3. Anderson M, Jiang J. Teens, social media & technology 2018. Pew Research Center. www.pewresearch.org/internet/2018/05/31/teens-social-media-technology-2018/.May 31, 2018. Accessed November 23, 2020. 4. Wiegand RD, Giusto NM, Rapp LM, Anderson RE. Evidence for rod outer segment lipid peroxidation following constant illumination of the rat retina. Invest Ophthalmol Vis Sci. 1983;24(10):1433-5. 5. Beatty S, Koh H, Phil M, Henson D, Boulton M. The role of oxidative stress in the pathogenesis of age-related macular degeneration. Surv Ophthalmol. 2000;45(2):115-34. 6. Youn HY, Chou BR, Cullen AP, Sivak JG. Effects of 400 nm, 420 nm, and 435.8 nm radiations on cultured human retinal pigment epithelial cells. J Photochem Photobiol B, Biol. 2009;95(1):64-70. 7. Zareba M, Skumatz CM, Sarna TJ, Burke JM. Photic injury to cultured RPE varies among individual cells in proportion to their endogenous lipofuscin content as modulated by their melanosome content. Invest Ophthalmol Vis Sci. 2014;55(8):4982-90. 8. Ratnayake K, Payton JL, Lakmal OH, Karunarathne A. Blue light excited retinal intercepts cellular signaling. Sci Rep. 2018;8(1):10207. 9. Taylor HR, West S, Muñoz B, Rosenthal FS, Bressler SB, Bressler NM. The long-term effects of visible light on the eye. Arch Ophthalmol. 1992;110(1):99-104. 10. Cruickshanks KJ, Klein R, Klein BE, Nondahl DM. Sunlight and the 5-year incidence of early age-related maculopathy: the beaver dam eye study. Arch Ophthalmol. 2001;119(2):246-50. 11. Tomany SC, Cruickshanks KJ, Klein R, Klein BE, Knudtson MD. Sunlight and the 10-year incidence of age-related maculopathy: the Beaver Dam Eye Study. Arch Ophthalmol. 2004;122(5):750-7. 12. Delacourt C, Carrière I, Ponton-Sanchez A, et al. Light exposure and the risk of age-related macular degeneration. Arch Opthalmol. 2001;119(10):1463-8. 13 Hirvelä H, Luukinen H, Läärä E, Sc L, Laatikainen L. Risk factors of age-related maculopathy in a Pppulation 70 years of age or older. Ophthalmology. 1996;103(6):871-7. 14. Clemons TE, Milton RC, Klein R, et al. Risk factors for the incidence of advanced age-related macular degeneration in the AREDS Report No. 19. Ophthamology. 2005;112(4):533-9. 15. McCarty CA, Mukesh BN, Fu CL, et al. Risk factors for age-related maculopathy: the visual impairment project. Arch Ophthalmol. 2001:119(10):1455-62. 16. The Eye Disease Case-Control Study Group. Risk factors for neovascular age-related macular degeneration. Arch Ophthalmol. 1992:110(12):1701-8. 17. Duane TD, Tasman W, Jaeger EA.. Ed. Baum, JL. Duane’s Ophthalmology. Philadelphia: Lippincott Williams & Wilkins; 2006 18. Zareba M, Skumatz CM, Sarna TJ, Burke JM. Photic injury to cultured RPE varies among individual cells in proportion to their endogenous lipofuscin content as modulated by their melanosome content. Invest Ophthalmol Vis Sci. 2014;55(8):4982-90. 19. Snodderly DM, Brown PK, Delori FC, Auran JD. The macular pigment. I. Absorbance spectra, localization, and discrimination from other yellow pigments in primate retinas. Invest Ophthalmol Vis Sci. 1984;25(6):660-73. 20. Bone RA, Landrum JT, Mayne ST, Gomez CM, Tibor SE, Twaroska EE. Macular pigment in donor eyes with and without AMD: a case-control study. Invest Ophthalmol Vis Sci. 2001;42(1):235-40. 21. Mainster MA. Violet and blue light blocking intraocular lenses: photoprotection versus photoreception. Br J Ophthalmol. 2006;90(6):784-92. 22. Hartwick, A. Vision Science 613: Monocular Sensory Processes. The Ohio State University College of Optometry; Spring 2011. 23. Keenan WT, Rupp AC, Ross RA, et al. A visual circuit uses complementary mechanisms to support transient and sustained pupil constriction. Elife. 2016;5 24. Gringras P, Middleton B, Skene DJ, Revell VL. Bigger, Brighter, Bluer-Better? Current Light-Emitting Devices - Adverse Sleep Properties and Preventative Strategies. Front Public Health. 2015;3:233. 25. O‘Hagan JB, Khazova M, Price LL. Low-energy light bulbs, computers, tablets and the blue light hazard. Eye (Lond). 2016;30(2):230-3. 26. Shields M. Overweight and obesity among children and youth. Health Rep. 2006;17(3):27-42. 27. Proctor MH, Moore LL, Cupples LA, et al. Television viewing and change in body fat from preschool to early adolescence: The Framingham Children’s Study. Int J Obes Relat Metab Disord. 2003;27(7):827-33. 28. van den Heuvel M, Ma J, Borkoff CM, et al. Mobile media device use is associated with expressive language delay in 18-month-old children. J Dev Behav Pediatrics. 2019; 40(2):99-104. 29. Madigan S, Browne D, Racine N, et al. Association between screen time and children’s performance on a developmental screening test. JAMA Pediatr. 2019;173(3):244-50. 30. Swing EL, Gentile DA, Anderson CA, Walsh DA. Television and video game exposure and the development of attention problems. Pediatrics. 2010; 126(2):214-21. 31. Montagni I ,Guichard E, Kurth T. Association of screen time with self-perceived attention problems and hyperactivity levels in French students: a cross-sectional study. BMJ Open. 2016;6:e009089. 32. Twenge JM and Campbell WK. Associations between screen time and lower psychological well-being among children and adolescents: evidence from a population-based study. Prev Med Rep. 2018;12:271-83. 33. Xiong S, Sankaridurg P, Naduvilath T, Zang J, et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol. 2017;95(6):551-66. 34. Jones LA, Sinnott LT, Mutti DO, et al. Parental history of myopia, sports and outdoor activities, and future myopia. 2007;48(8):3524-32. 35. Zadnik K, Mutti Do. Outdoor activity protects against childhood myopia-let the sun shine in. JAMA Pediatr. 2019;173(5):415-6. 36. Chang AM, Aeschbach D, Duffy JF, Czeisler CA. Evening use of light-emitting eReaders negatively affects sleep, circadian timing, and next-morning alertness. Proc Natl Acad Sci USA. 2015;112(4):1232-7. 37. Oh JH, Yoo H, Park HK, Do YR. Analysis of circadian properties and healthy levels of blue light from smartphones at night. Sci Rep. 2015;5:11325. 38. Taylor HR, West S, Muñoz B, Rosenthal FS, Bressler SB, Bressler NM. The long-term effects of visible light on the eye. Arch Ophthalmol. 1992;110(1):99-104. 39. Freudenthaler N, Neuf H, Kadner G, Schlote T. Characteristics of spontaneous eyeblink activity during video display terminal use in healthy volunteers. Graefes Arch Clin Exp Ophthalmol. 2003;241(11):914-20. 40. Orben A, Przbylski AK. The association between adolescent well-being and digital technology use. Nat Hum Behav. 2019;3(2):173-82. 41. Palavets T, Rosenfield M. Blue-blocking Filters and Digital Eyestrain. Optom Vis Sci. 2019;96(1):48-54. 42. Lawrenson JG. Hull CC, Downie LE. The effect of blue-light blocking spectacle lenses on visual performance, macular health and the sleep-wake cycle: a systematic review of the literature. Ophthalmic Physiol Opt. 2017;37(6):644-54. 43. Chang A-M, Aeschbach D, Duffy JF, Czeisler CA. Evening use of light-emitting eReaders negatively affects sleep, circadian timing and next-morning alertness. Proc Natl Acad Sci USA. 2015;112(4):1232-37. 44. Teran E, Yee-rendon CM, Ortega-salazar J, De gracia P, Garcia-romo E, Woods RL. Evaluation of Two Strategies for Alleviating the Impact on the Circadian Cycle of Smartphone Screens. Optom Vis Sci. 2020;97(3):207-217. 45. Nagare R, Plitnick B, Figueiro MG. Does the iPad Night Shift mode reduce melatonin suppression?. Light Res Technol. 2019;51(3):373-383. 46. AAP: finding ways to keep children occupied during these challenging times. American Academy of Pediatrics. services.aap.org/en/news-room/news-releases/aap/2020/aap-finding-ways-to-keep-children-occupied-during-these-challenging-times/. March 17, 2020. Accessed November 23, 2020. |

