 |
A 53-year-old Caucasian female was referred for a suspicious retinal lesion in her right eye. Her ocular history was significant for a radial keratotomy (RK) performed in her right eye more than 20 years earlier with an excellent visual result. The left eye has always been worse.
She reports being in good health, though her medical history is significant for allergies. She takes Flonase (fluticasone, GlaxoSmithKline) nasal spray and over the counter Claritin (loratadine, Bayer).
 |
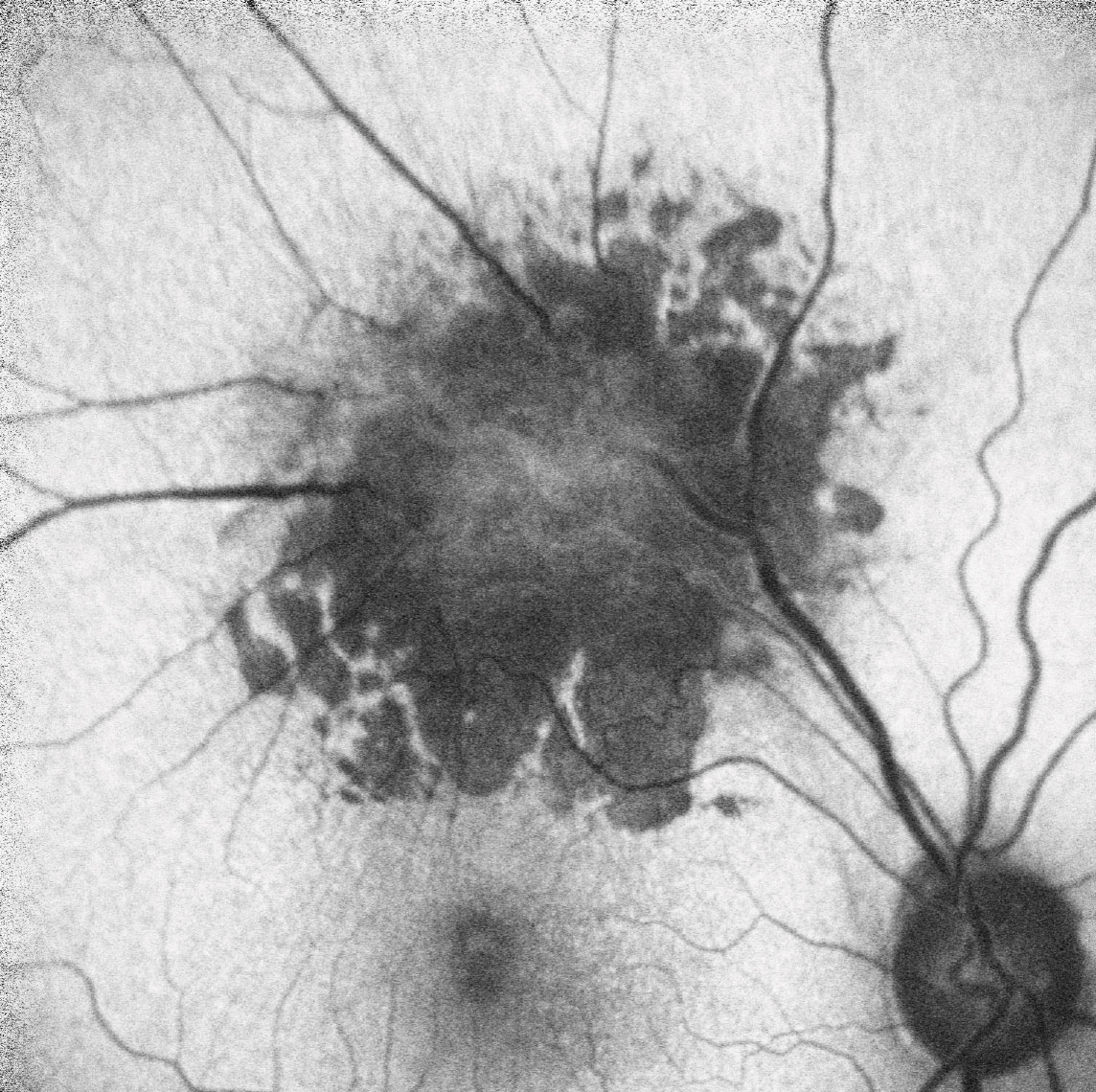 |
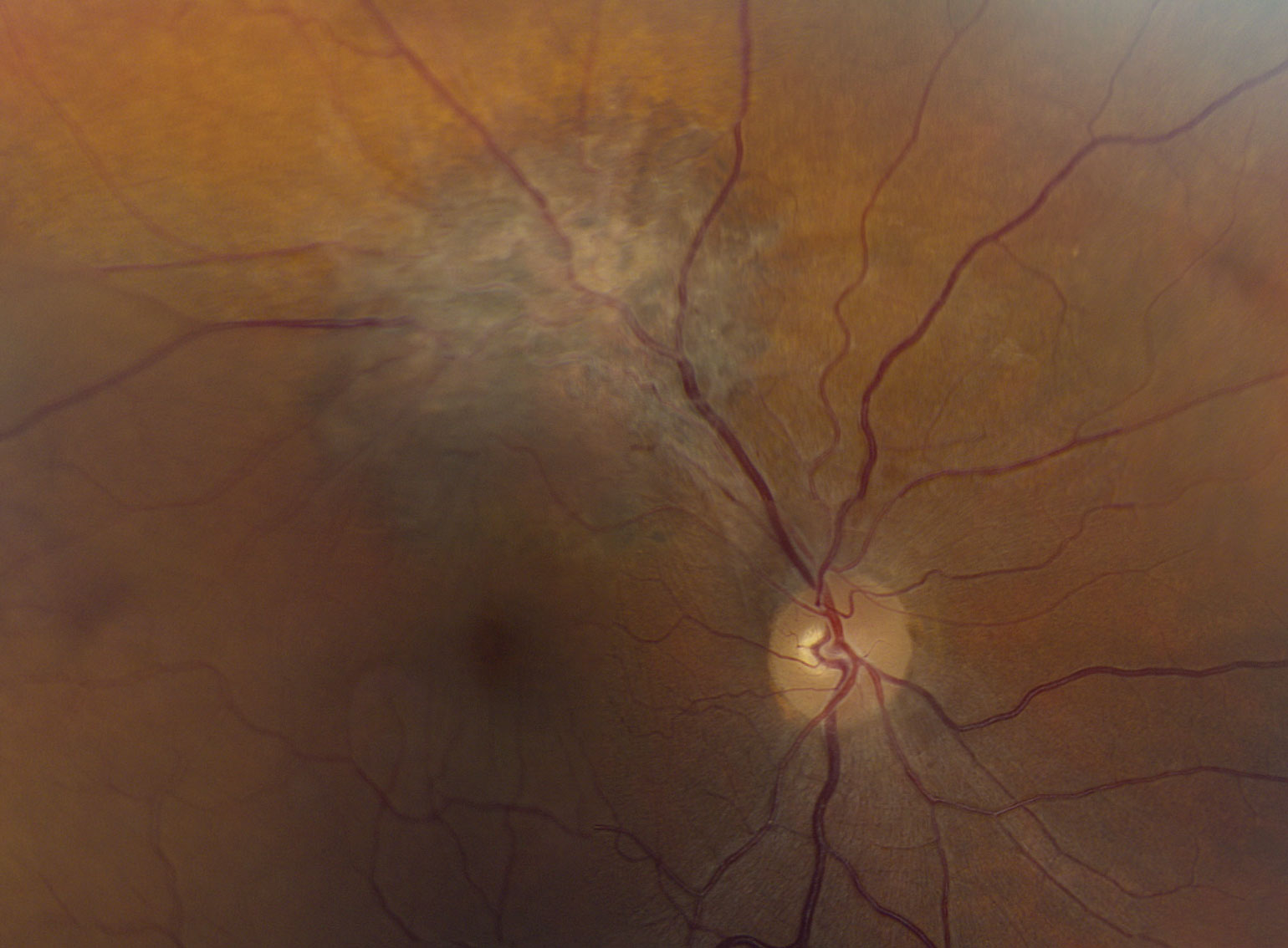
| Figs. 1 and 2. A widefield (above) and close up view (below) of the right eye of our patient. Click images to enlarge. |
Evaluation
On examination, her uncorrected visual acuity measured 20/20 OD and 20/100 OS. With a hyperopic correction of +3.25 –0.75x090 she corrected to 20/20. Confrontation visual fields were full-to-careful finger counting in both eyes. Her ocular motility testing was normal and her pupils were equally round and reactive without an afferent papillary defect. Her right anterior segment was significant for multiple radial corneal scars consistent with her RK. Her tensions measured 16mm Hg OD and 14mm Hg OS.
On dilated fundus exam, her optic nerves appeared heathy with a small cup and good rim coloration and perfusion OU. Obvious retinal changes were seen in the right eye along the superior temporal arcade (Figure 1). Fundus autofluoresence (FAF) and spectral-domain OCT and OCT angiography (OCT-A) were also performed (Figures 2 and 3).
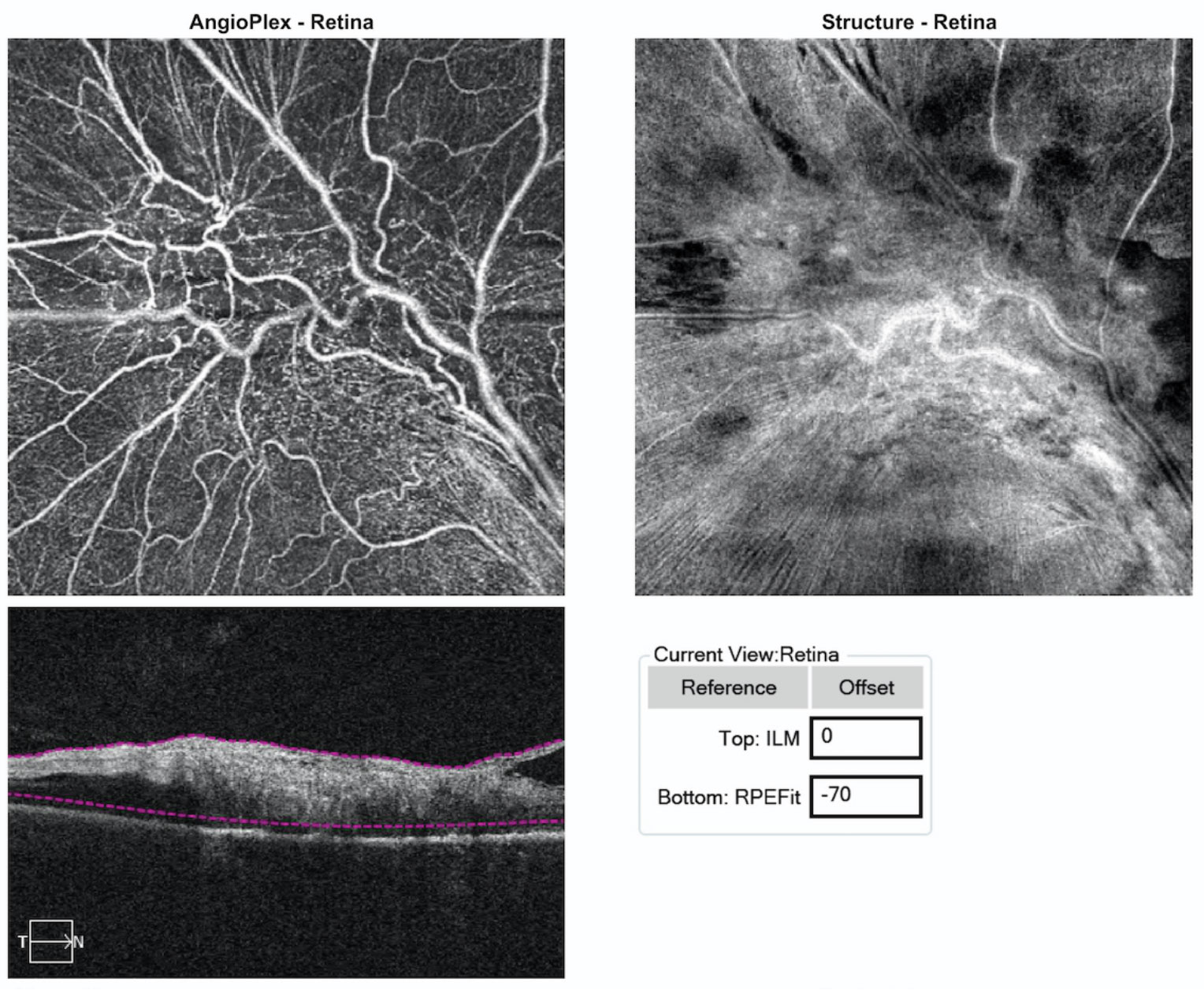 |
| Fig. 3. These images represent 6x6mm OCT-A of the lesion. Note the findings within the sensory retina. Click image to enlarge. |
Take the Retina Quiz
1. What is the most likely diagnosis?
a. Eccentric epiretinal membrane.
b. Choroidal melanoma.
c. Combined hamartoma of the retina and retinal pigment epithelial.
d. Astrocytic hamartoma.
2. What are the essential findings on SD-OCT?
a. Epiretinal membrane.
b. Choroidal neovascularization.
c. Complete disorganization of the retinal anatomy.
d. Both a and c.
3. How should this patient be managed?
a. Close observation.
b. Plaque brachytherapy.
c. Enucleation.
d. Pars plana vitrectomy.
4. What is the prognosis?
a. Stability with no effect on visual function.
b. Slow, steady progression and loss of visual function.
c. Will likely develop macular chorioretinal scaring.
d. Will develop cystoid macular edmea or choroidal neovascularization, or both, over time.
Diagnosis
Along the superior temporal arcade in the right eye there is a mildly elevated charcoal gray lesion with an overlying epiretinal membrane (ERM). There is clear tortuosity of the retinal vessels, and retinal striae can be seen extending inferior close to the macula. No exudate or fluid was associated with this lesion. So, what does this represent? The color, thickness and the presence of the ERM suggest that this is a combined hamartoma of the retina and retinal pigment epithelium (CHR-RPE), a rare benign tumor.1
Discussion
These rare benign tumors are congenital and most commonly diagnosed in childhood. They are most often located adjacent to the optic nerve but can be seen almost anywhere in the retina, posterior, mid-periphery or periphery. Up to 40% may have reduced acuity and 28% may have strabismus.1,2 These tumors represent a disorganized amalgamation of glial tissue in addition to retinal and retinal pigment epithelium RPE cells.2 Variations in the proportions of these components contribute to the variations in clinical appearance.
CHR-RPE are similar to congenital hypertrophy of the RPE (CHRPE), but CHRPE tend to be darker, flatter and have more defined borders. Other differential diagnoses include choroidal melanoma, choroidal hemangioma, osteoma and astrocytic hamartoma. For the most part, the diagnosis is based on the clinical presentation, but ancillary testing such as standardized ultrasound, OCT, fluorescein angiography and FAF may be helpful in establishing a diagnosis.
One of the most characteristic features of CHR-RPE is the presence of fibrous tissues and epiretinal membrane on the surface of the tumor. The OCT may be helpful in visualizing the ERM. In a study of 11 patients with CHR-RPE, a distinct ERM was present in 10 patients.3 Nine of these patients displayed clearly evident retinal folds and striae, and three had significant vitreoretinal traction. All of the patients showed complete retinal anatomic disorganization with an inability to identify the retinal layers.3
The SD-OCT and OCT-A images of our patient had very similar features. We saw thickening of the sensory retina and an ERM as well as anatomic disorganization within the sensory retina. It is important to note the clear delineation of the boundary between the RPE and choroid. This is helpful in identifying the anatomic location of this lesion (sensory retina), and it helps rule out choroidal tumors, such as a melanoma or hemangioma. The OCT-A brilliantly highlights the tortuosity of the retinal vessels as well as the clearly visible microvasculature.
An ultrasound confirmed the absence of a choroidal mass, and the FAF showed dramatic hypofluoresence in the area where the hamartoma was located with distinct borders. All of these tests confirmed the diagnosis of CHR-RPE.
The findings were explained to our patient, and she was relieved to learn that it was benign and not likely to have any effect on her visual function, especially considering she functions monocularly. We discussed options for correcting the left eye, including using contact lenses, but she was content to leave it as it is and only wear a prescription for near work. She will continue to be closely followed to make sure it does not change.
1. Gass JD. An unusual hamartoma of the pigment epithelium and retina simulating choroidal melanoma and retinoblastoma. Trans Am Ophthalmol Soc. 1973;71:171,83; discussions 184-5. 2. Schachat A, Shields J, Fine S. The Macula Society Research Committee. Combined hamartomas of the retina and retinal pigment epithelium. Ophthalmol. 1984;91(12):1609–14. 3. Shields C, Mashayekhi A, Dai V, et al. Optical coherence tomographic findings of combined hamartoma of the retina and retinal pigment epithelium in 11 patients. Arch Ophthalmol. 2005;123(12):1746-50. |
Retina Quiz Answers:
1) c; 2) c; 3) a; 4) a

