Published December 22, 2004
Is This Blur Tied To Glaucoma?
Andrew S. Gurwood, O.D.
History
A 44-year-old black male presented for an eye examination with a chief complaint of blurred near vision over the past two months. His ocular history was noncontributory. His systemic history revealed hypertension, myocardial infarction, and arteriole and atherosclerosis.
Diagnostic Data
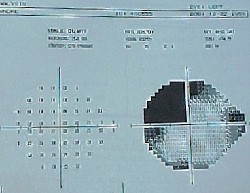
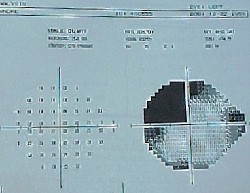
His best-uncorrected visual acuity was 20/20 O.U. at distance and 20/30 O.U. at near. External examination revealed no extraocular muscle restriction, but it did uncover a bilateral, left visual field restriction. The anterior segments of both eyes were normal, with open angles. IOP measured 18mm Hg O.U.
Dilated funduscopy of both peripheries was normal. Both optic nerves had cup-to-disc ratios of 0.55 x 0.60. Results from pertinent additional studies are illustrated in the photographs.
 |
| The patient had this visual field O.D. |
 |
| The patient had this appearance in an MRI study. |
Your Diagnosis
How would you approach this case? Does this patient require any additional tests? What is your diagnosis? How would you manage this patient? What is the likely prognosis?
Discussion
The diagnosis in this issue is left homonymous superior quadrantnopsia, presumably secondary to a cerebrovascular accident (CVA). Additional testing must include a cursory glaucoma work-up, including:1,2
Additional history to inquire about blood tissue abnormalities, blood loss and migraine headache.
Visual fields to uncover functional losses.
Nerve fiber layer analysis to gather an understanding of the retinal and neural structure.
Gonioscopy to establish drainage angle status.
Photographs to document the nerves appearance.
Given that the patients IOP appears to be within a normal range, diurnal pressure measurements should be considered. In a young individual, the diagnosis of normal-tension glaucoma should be one of exclusion and should stimulate some investigation of perfusion. Additional inquirysuch as neuroimaging, neurologic referral and internal medicine referral to rule out issues of vasculopathy or cardiac diseaseis reasonable.3,4
Upon further questioning, the patient indicated that he could no longer write because he could not maintain a grip on a pencil with his left hand. As such, we contacted the internal medicine attending physician and obtained a neurological consult. Neuroimaging uncovered a right temporal lobe CVA. The patients hypertensive medications were titrated to have a more substantial effect.
Even though the neurologic work-up yielded a positive result, this in no way absolves this patient from also having normal tension glaucomatous optic neuropathy. Therefore, the work-up and baseline data collection was completed and the patient continues to be monitored.
1. In: Yanoff M, Duker JS. Ophthalmology. Philadelphia: Mosby, 1999; 8(44): 1-6.
2. Rhee DJ, Pyfer MF. Differential diagnosis of ocular signs. In: Rhee DJ, Pyfer MF. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease, 3rd ed. Philadelphia: Lippincott Williams and Wilkins, 1999: 7-17.
3. Lalle PA. Visual Fields. In: Gurwood AS, Muchnick BG. The Optic Nerve in Clinical Practice. Boston: Butterworth-Heinemann, 1997: 27-66.
4. Gurwood AS. A Smarter Way to Decipher Defects: A Guide for Interpretation of Visual Fields. Dicon Publications, Inc. 1995; 1(1): 17-21.
|
Next Month in the Mag |
|
Cover Story: Optometry at the Crossroads. Some optometrists embrace disease management and clinical care. Others see this as abandoning traditional optometryperforming thorough visual exams and prescribing glasses and contact lenses. Managing Editor Jeff Eisenberg analyzes how the profession is splitting its focus, and whether the two ends can happily coexist.
Are You On Call? A patients emergency may often be resolved or addressed by a brief return phone call. Can your patients reach you easily after hours, or do you direct them elsewhere? Or do they just get your answering machine? Heres how to provide the care when youre not there.
Halting Apoptosis in Glaucoma. Some investigators suggest the possibility that there may be a way to sever the link between programmed cell death and glaucoma. Heres a look at the most promising research.
Also in this issue:
A Look at High Oxygen Contact Lens Materials.
Optometric Study Center: Warning Signs of Systemic Disease.
A Field Guide to SECO.
Feedback
Review of Optometry welcomes questions and comments. Contact Amy Hellem, editor-in-chief, ahellem@jobson.com with Letter to the Editor as the subject line. Or, write to Review of Optometry, 11 Campus Blvd., Suite 100, Newtown Square, PA 19073. |
Vol. No: 141:12Issue:
12/15/04