A 46-year-old Hispanic male with a history of diabetic retinopathy presented for a regular follow-up examination.

The patient has had type 1 diabetes since age 2. Eight years before this visit, he went blind in his left eye due to complications from proliferative diabetic retinopathy and neovascular glaucoma.
Vision in the right eye had stabilized, and the patient achieved excellent acuity after extensive laser photocoagulation and cataract extraction. The patient reported no changes in his vision at a follow-up exam six months post-op.
Best-corrected visual acuity at this visit measured 20/25 O.D. and no light perception O.S. A confrontation visual field in the right eye was full to careful finger counting.
Anterior segment exam of the right eye was unremarkable. There was no evidence of iris or angle neovascularization. The patient had a well-centered posterior chamber intraocular lens.
Anterior segment exam of the left eye was significant for an irregular pupil and dense cataract.
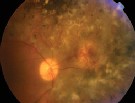
1. Dilated fundus exam of the right eye revealed a suspicious lesion on the nasal side of the optic nerve. Also, note the laser photocoagulation scars in the peripheral retina.
Intraocular pressure measured 15mm Hg in both eyes.
Dilated fundus exam of the right eye showed a healthy optic nerve with a small cup, and good rim coloration and perfusion. The macula appeared flat, and there was no clinically significant macular edema. There was extensive scarring at 360 in the peripheral retina from the laser photocoagulation but no evidence of neovascularization or vitreous hemorrhage.
Of particular interest was a yellow-white elevated lesion that appeared nasal to the optic nerve (figure 1). There appeared to be a localized serous retinal detachment surrounding the lesion. We obtained a fluorescein angiogram (figures 2 and 3).
Take the Retina Quiz
1. How would you classify this patients lesion?
a. Vascular.
b. Malignant.
c. Proliferative.
d. Both a and c.
2. What is the significant finding of the angiogram?
a. Active neovascularization.
b. A malignant mass.
c. An afferent and efferent vascular system.
d. Cicatricial diabetic change.
3. What does the lesion represent?
a. Amelanotic choroidal melanoma.
b. Retinal angioma.
c. Vasoproliferative tumor of the retina.
d. Localized area of neovascularization.
4. What is the correct management option for this patient?
a. Observation.
b. Laser photocoagulation.
c. Photodynamic therapy.
d. All are reasonable options.
For answers, click here.
Discussion
Our patient has a vasoproliferative tumor, a highly vascularized, benign tumor of the retina. These tumors usually occur in the peripheral retina, but they can also be seen in the posterior pole, as with our patient.
Vasoproliferative tumors mostly occur in healthy individuals with no evidence of prior ocular disease. However, they also may occur due to complications from retinal surgery or retinal disease, including uveitis, sickle-cell disease and retinopathy of prematurity. There are no reports of vasoproliferative tumors as a complication of diabetic retinopathy.
Vasoproliferative tumors may resemble the retinal angiomatous masses that are seen with von Hippels disease and may even be confused with amelanotic choroidal melanomas.
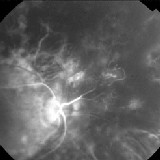
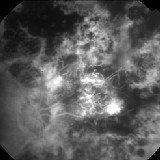
2, 3. Fluorescein angiogram of the lesion at 12 and 20 seconds. Note the filling pattern of the lesion. The afferent feeder vessel lights up very early in the angiogram, followed by the vascular channels within the tumor as the dye begins to fill. The efferent drainage vessel fluoresces last during the venous phase of the angiogram.
Ophthalmologist Jerry Shields first described these lesions in 1983 as presumed acquired retinal hemangiomas.1 He renamed them vasoproliferative tumors in 1995, as their characteristics became better understood.2
Vasoproliferative tumors of the retina typically have both an afferent and efferent vascular system that supplies blood to the tumor. The afferent feeder vessel lights up very early in the angiogram, followed by the vascular channels within the tumor as the dye begins to fill. The efferent drainage vessel fluoresces last during the venous phase of the angiogram.
Reactionary proliferation of glial cells and secondary vasoproliferation within the tumors allow for their potential growth. As they grow, they can develop intraretinal and subretinal exudation with or without retinal detachment. They may also develop subretinal and/or vitreous hemorrhage, and even macular edema depending on the location of the tumors.
Our patients tumor was on the nasal side of the optic nerve, so the macula was spared. However, we are concerned about the small exudative retinal detachment associated with his tumor.
Because this patient has excellent visual acuity in his right eyehis only seeing eyewe initially elected to observe him.
We instructed the patient to return in six weeks (this visit is after Review of Optometrys press time). At that time, we will decide how to manage his condition.
We have several options for treating vasoproliferative tumors of the retina. These include laser photocoagulation, cryotherapy and plaque radiotherapy. Each has proven successful, depending on the location of the tumor.
In a case study, a patient successfully underwent photodynamic therapy. This led to selective closure of the neovascular tissue.3
Well keep you posted on what management option we choose for our patient.
1. Shields JA, Decker WL, Sanborn GE, et al. Presumed acquired retinal hemangiomas. Ophthalmology. 1983 Nov;90(11):1292-300.
2. Shields CL, Shields JA, Barrett J, De Potter P. Vasoproliferative tumors of the ocular fundus. Classification and clinical manifestations in 103 patients. Arch Ophthalmol 1995 May;113(5):615-23.
3. Barbezetto IA, Smith RT. Vasoproliferative tumor of the retina treated with PDT. Retina 2003 Aug;23(4):565-7.

