 As we all know, health care costs are skyrocketing across the globe. Medication prices are no exception. Due to these high medication costs, patient compliance can often suffer, especially for patients with chronic conditions such as hypertension or glaucoma. For example, patients may be willing to skip a drop here or there to save themselves the hundreds of dollars for doing without one or two bottles of a prostaglandin analogue per year.
As we all know, health care costs are skyrocketing across the globe. Medication prices are no exception. Due to these high medication costs, patient compliance can often suffer, especially for patients with chronic conditions such as hypertension or glaucoma. For example, patients may be willing to skip a drop here or there to save themselves the hundreds of dollars for doing without one or two bottles of a prostaglandin analogue per year.
In the long term, lower medication compliance has the potential to worsen a patient’s condition—whether it is ocular or systemic—and increase the mortality and/or morbidity associated with that progression.
As prescribing clinicians, we must remember that cost is a major factor in drug usage and compliance, and our prescribing decisions have financial consequences—not only for our patients, but also for our health care system.
To that point, how can we find and prescribe the most appropriate drug for the best price?
Talk to the Pharmacist
There is no better way to become better informed about prescription drugs and their price points than talking to the experts themselves, the pharmacists. Developing a trusting relationship with your local pharmacists will not only improve your expertise and confidence, but give you assurance that they have your patient’s best interest at heart.
This relationship comes in handy in an all-too-familiar scenario: The patient takes your newly written prescription to the drug store, only to be told that the medication is not covered under their insurance plan. Unless the pharmacist makes a point to call and let you know the drug is not on the patient’s formulary, the patient could leave the pharmacy without getting the prescription filled.
Other times, the patient doesn’t learn or understand that there are other, similar medications that are covered on their insurance formulary. So, unless the pharmacist proactively provides a substitution, the patient pays out-of-pocket for the expensive prescribed medication instead of a much lower co-pay for a similar medication of the same drug class.
Cultivate a mutual professional relationship with your local pharmacists to help avoid these unfortunate situations—or to fix them with a quick phone call if they should occur.
Go Generic When Necessary
The debate over prescribing generic vs. brand-name meds is nothing new to practitioners across all fields of medicine. Numerous articles in Review have looked at both sides of this topic in the past.1-4 As the doctor, it’s our job to prescribe the most effective medication to treat each patient’s particular condition. But, it is also our job to consider costs when choosing a medication for the patient. At least one in 10 Americans cite cost as a barrier to medication compliance.5 Even worse, nearly half of glaucoma patients discontinue their drops within six months due to a variety of reasons—not the least of which is cost.6
Therefore, we need to prescribe thoughtfully, and that decision-making process should include cost for the patient and our health care system.
Ideally, generic medications lower or remove the cost barrier and improve management and patient compliance. For example, now that a more affordable generic prostaglandin analogue is available, patients who were previously on generic timolol BID or generic dorzolamide TID, or those who had refused treatment, can take generic latanoprost. This kind of switch between classes of glaucoma medications should lead to significantly greater compliance due to the prostaglandin’s once-daily dosage schedule.
Likewise, you may have had patients, without your knowledge or approval, use their brand-name Xalatan every other night to try and stretch that expensive one-month bottle to two months. I actually had one patient tell me that she was alternating her glaucoma medications and heart medications on a month-by-month basis because she could not afford both at the same time! A cheaper, generic option prevents a scenario that could have resulted in significant morbidity and/or mortality consequences for this patient.
The potential cost savings of generics not only apply to the patient, but to our health care system as well. Doctors and health policy analysts largely agree that generic medications bring significant savings to health care costs. A 2005 report estimated that for every 1% increase in generic drug use, overall spending on prescription drugs would be reduced between $1.3 to $4 billion annually.7
More recently, the Affordable Care Act (ACA) closes the Medicare Part D doughnut hole—the gap in drug coverage during which people with Medicare must pay the full cost of their prescriptions out of pocket. Over the next few years, the ACA will gradually phase out the doughnut hole coverage gap by decreasing the Medicare beneficiary’s share of drug costs for both brand-name and generics, until the doughnut hole closes in 2020.
While generics have a cost advantage, keep in mind their potential limitations. For instance, while the initial brand-name company must submit to rigorous drug testing and lengthy clinical trials when applying to the Food and Drug Administration, companies that produce generic medications merely submit an abbreviated form for approval. Safety and efficacy do not have to be proven or established with generics because thorough testing on the branded medication has presumably already been conducted. Companies merely have to show the FDA that their drugs have the same active ingredients and are bioequivalent to the brand-name medication.8
Ophthalmic topical drugs, because they have such a sensitive and particular route of administration, are held to a different standard than systemic drugs. Currently, generic ophthalmic solutions, such as latanoprost, are expected to have both the same active and inactive ingredients in the same concentrations (both active and inactive). If they are not the same, then a study comparing the clinical bioequivalence has to be performed.9
By the same token, suspensions, ointments and emulsions—in which the distribution of particles can make a difference—are also required to have comparative studies prior to approval of a generic product.9
Our patient demographics and strict hospital formulary at the Oklahoma College of Optometry make generics a major player in our prescribing. Anecdotally, we have years of success managing both acute and chronic cases with generics, and can attest to the patient satisfaction that comes with healing and/or managing a condition at the best possible price for that patient. Glaucoma, non-vision threatening corneal ulcers and various forms of ocular surface inflammation have been well handled with generics. However, for more severe corneal ulcers, advanced glaucoma and especially iritis, we lean toward the newer, brand-name antibiotics, hypotensives and steroid medications, respectively.
Use Sites and Apps
Online websites such as GoodRx.com and LowestMed.com have become major resources for patients and practitioners alike when deciding where to send and fill medication scripts.
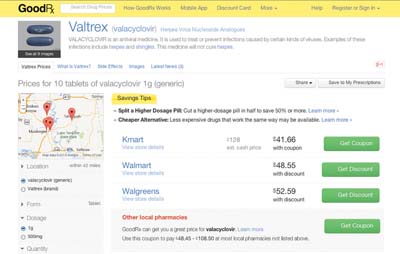 GoodRx, founded in 2011, pitches itself as a resource for the millions of uninsured Americans who have to pay full price for medicine, as well as people with insurance who may not realize that they can often find generic meds for less than the cost of their typical co-pay. Patients and doctors can visit the GoodRx.com website or download the free app to their smartphone or tablet. Simply type in the name of the medication and your city or zip code and—voila!—you’ll get a list of pharmacies in your area that carry the drug, plus the price of that medication at each pharmacy with a coupon that can be printed, emailed or texted directly to the patient. Additionally, you can narrow your search based on how far you want to travel to the various pharmacies, what form the medication comes in, the dosage and quantity, as well as the pharmacy type.
GoodRx, founded in 2011, pitches itself as a resource for the millions of uninsured Americans who have to pay full price for medicine, as well as people with insurance who may not realize that they can often find generic meds for less than the cost of their typical co-pay. Patients and doctors can visit the GoodRx.com website or download the free app to their smartphone or tablet. Simply type in the name of the medication and your city or zip code and—voila!—you’ll get a list of pharmacies in your area that carry the drug, plus the price of that medication at each pharmacy with a coupon that can be printed, emailed or texted directly to the patient. Additionally, you can narrow your search based on how far you want to travel to the various pharmacies, what form the medication comes in, the dosage and quantity, as well as the pharmacy type.
This service has proved invaluable numerous times right in the exam lane when I’m deciding which medication to prescribe for my patient. Recently, I had a patient with herpes zoster ophthalmicus who presented beyond the classic 72-hour treatment window. Due to recent studies pointing toward a possible increased efficacy when using Valtrex (valacyclovir, GlaxoSmithKline) or Famvir (famciclovir, Novartis) compared with acyclovir when initiating treatment after 72 hours, the treatment of choice in this case really needed to be one of the newer antivirals.10-12 However, neither was on our hospital formulary and the patient did not have insurance.
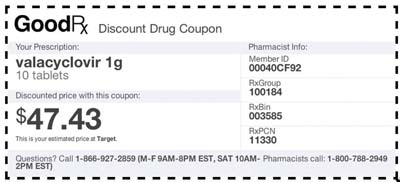 I pulled out my iPhone, opened the GoodRx app, typed in Valtrex and our zip code. I narrowed the search to 1g dosage and 30 tablets (enough for 10 days). GoodRx showed price results for both the brand-name Valtrex and the generic valacyclovir. (One of the many helpful features of GoodRx is that it defaults to the generic if one is available.) According to the app, the lowest price available for the brand-name drug was $376 at Walmart, and the lowest price for the generic was $52, also at Walmart. The next cheapest generic was $84 at HealthWarehouse, a mail order.
I pulled out my iPhone, opened the GoodRx app, typed in Valtrex and our zip code. I narrowed the search to 1g dosage and 30 tablets (enough for 10 days). GoodRx showed price results for both the brand-name Valtrex and the generic valacyclovir. (One of the many helpful features of GoodRx is that it defaults to the generic if one is available.) According to the app, the lowest price available for the brand-name drug was $376 at Walmart, and the lowest price for the generic was $52, also at Walmart. The next cheapest generic was $84 at HealthWarehouse, a mail order.
After I discussed with the patient the importance, need and affordability of the newer antiviral, he decided to fill the script at Walmart. Over the course of a two-week period, his ocular shingles outbreak resolved without sequelae or development of post-herpetic neuralgia.
This is just one of the many positive results that online tools can provide to both doctors and patients. Other useful features on GoodRx include a pill identifier, which identifies the medication via the imprint on the tablet or capsule, and lets patients know where to find the cheapest cost for a medication whose name they don’t know.
Patient Assistance Programs
Obviously, there is no better price than free. For patients with economic hardship, patient assistant programs offer the prescriber and patient one last possible avenue for access to necessary medications, both generic or brand name. Fortunately, most of the larger drug companies offer assistance programs to help low-income patients meet the soaring costs of therapy.
RxHope.com provides a central clearinghouse for most major patient assistance programs, including those of ocular drug companies such as Alcon, Allergan, Bausch + Lomb, Genentech, Merck, Ocusoft and Pfizer.
After entering your contact and licensure information, as well as some basic facts about the patient, RxHope can create and complete an online form for each individual company and drug request; this, in turn, can be printed, signed and sent to the company for processing. Be aware that each pharmaceutical company establishes its own guidelines and manages its own assistance program, so the requirements, ease of use and processing time can vary substantially.
Of course, most companies require that the patient be a US citizen, have no other prescription coverage including Medicaid or Medicare Part D, and have an annual household income at or below 200% of the current Federal Poverty Level.13 (For an individual in 2014, this translates to less than $23,340 per year.14) Most plans also require patients to submit supporting documentation.
Despite its limitations, RxHope provides a relatively quick and easy method for determining which drugs are available through patient assistance programs and helps to facilitate these requests for our patients.
There is clearly a need for greater transparency in health care costs, and prescription drugs are an obvious candidate for sunlight. Even if your patient is well-insured and may not need to comparison shop for meds, it’s enlightening for doctors and patients alike to understand the wide price disparity that exists among competing pharmacy chains. This is particularly true for generic medications, as my patient on valacyclovir demonstrated.
Knowing where to direct your patients to fill a script can save them money, gain you loyalty and, most importantly, give you peace of mind in knowing that you prescribed the most effective medication at the best price.
Dr. Lighthizer is an assistant professor and the chief of both specialty care clinics and electrodiagnostics clinic at the Oklahoma College of Optometry.
1. Chu E, Hamp A. Generic vs. brand drugs: Which is better? Rev Optom. 2012 Feb;149(2):68-75.
2. Kabat A, Sowka J. Pharmaceuticals for all budgets. Rev Optom. 2010 Oct;147(10):103-6.
3. Murphy J. Switching meds when the formulary says ‘no.’ Rev Optom. 2010 Feb;147(2)73-80.
4. Bowling E. Generics: friend or foe? Rev Optom. 2011 Feb;148(2):82-6.
5. Kennedy J, Morgan S. A cross-national study of prescription nonadherence due to cost: data from the Joint Canada-United States Survey of Health. Clin Ther. 2006 Aug;28(8):1217-24.
6. Nordstrom BL, Friedman DS, Mozaffari E, et al. Persistence and adherence with topical glaucoma therapy. Am J Ophthalmol. 2005 Oct;140(4):598-606.
7. Subcommittee on Health of the Committee on Energy and Commerce Hearing, House of Representatives, 109th Congress. Increasing Generic Drug Utilization: Saving Money for Patients. May 18, 2005. Available at: www.gpo.gov/fdsys/pkg/CHRG-109hhrg21639/pdf/CHRG-109hhrg21639.pdf. Accessed December 10, 2013.
8. Cantor LB. Ophthalmic generic drug approval process: implications for efficacy and safety. J Glaucoma. 1997 Oct;6(5):344-9.
9. American Academy of Ophthalmology/ONE Network website. Questions About Generic Ophthalmic Medications. September 2011. Available at: http://one.aao.org/asset.axd?id=bd41e411-cedc-4992-9ed5-4b3f60dafc18. Accessed January 13, 2014.
10. Wood MJ, Shukla S, Fiddian AP, Crooks RJ. Treatment of acute herpes zoster: effect of early (<48 h) versus late (48-72 h) therapy with acyclovir and valaciclovir on prolonged pain. J Infect Dis 1998;178:Suppl 1:S81-S84.
11. Decroix J, Partsch H, Gonzalez R, et al. Factors influencing pain outcome in herpes zoster: an observational study with valaciclovir. Valaciclovir International Zoster Assessment Group (VIZA). J Eur Acad Dermatol Venereol. 2000 Jan;14(1):23-33.
12. Ormrod D, Goa K, et al. Valaciclovir: a review of its use in the management of herpes zoster. Drugs. 2000;Jun;59(6):1317-40.
13. Patient Assistance Programs. RxHope. Available at: www.rxhope.com. Accessed December 3, 2013.
14. US Department of Health & Human Services. 2014 Federal Poverty Guidelines. Available at: http://aspe.hhs.gov/poverty/14poverty.cfm. Accessed January 23, 2014.

