 |
An 80-year-old Hispanic female presented complaining of blurry vision—in the right eye more than the left—at distance and near over the last year. Her ocular history was remarkable for cataract surgery in both eyes and her medical history was significant for hypertension, hyperlipidemia and asthma.
Examination
Her best-corrected visual acuity was 20/70 in the right eye and 20/40 in the left eye. Pupils were equal, round and reactive to light without afferent pupillary defect. Ocular motility was full in both eyes. Confrontation visual fields were full to finger count in each eye. Her intraocular pressures were 12mm Hg OD and 13mm Hg OS.
Anterior segment examination revealed mild meibomian gland dysfunction and dry eye, but was otherwise unremarkable. There was a posterior chamber intraocular lens in each eye with no posterior capsular opacification. Dilated fundus examination of the right eye revealed clear vitreous and a healthy optic nerve.
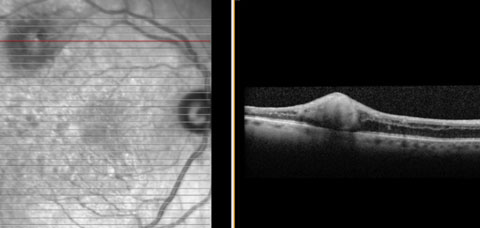
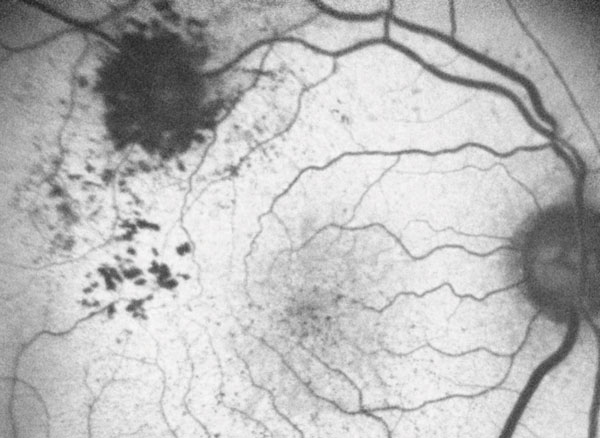
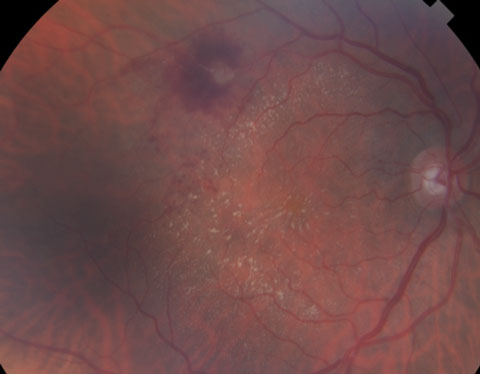
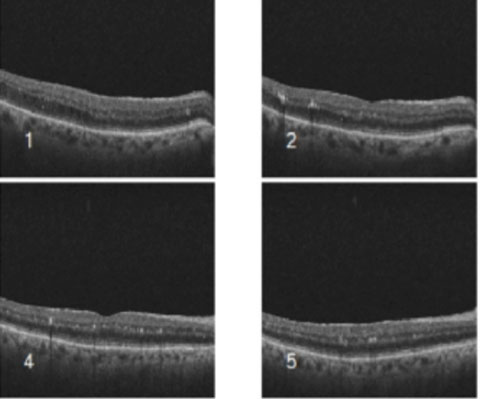
There were some notable findings within the macula and along the superior temporal arcade (Figure 1). There was mild attenuation of the retinal vasculature. An optical coherence tomography (OCT) of the macula was taken (Figure 2) as well as a fundus autofluorescence photo (Figure 3). Dilated fundus examination of the left eye was significant for macular drusen and mild attenuation of the retinal vasculature.
 |
| Fig. 1. Fundus photo of the right eye showing areas of intraretinal and subretinal hemorrhages along the superotemporal arcade surrounding a macroaneurysm. |
Take the Retina Quiz
1. What additional test would be helpful to confirm the diagnosis?
a. Fluorescein angiography.
b. Fundus autofluorescence.
c. SD-OCT.
d. All of the above.
2. How could this patient be managed?
a. Observation.
b. Anti-VEGF injection.
c. Focal laser photocoagulation.
d. Both b and c.
3. What is the most common systemic condition associated with this ocular condition?
a. Diabetes mellitus.
b. Hypertension.
c. Hyperlipidemia.
d. Thyroid disease.
4. What other ocular conditions are commonly associated with this diagnosis?
a. Retinal artery occlusion.
b. Retinal detachment.
c. Retinal vein occlusion.
d. Both a and c.
5. In which patients does this condition typically occur?
a. Young males.
b. Elderly males.
c. Young females.
d. Elderly females.
 |
| Fig. 2. OCT of the right eye showing a hyperreflective wall in the area of the marcoaneurysm as well as intraretinal edema with no choroidal abnormality. |
Diagnosis
Based on the clinical appearance, as well as the medical history, we diagnosed the patient with retinal artery macroaneurysm (RAM). As you follow the superior temporal artery, a large aneurysmal dilation of the artery can be seen with surrounding retinal hemorrhage and exudate. Spectral domain OCT (SD-OCT) showed an adequate amount of intraretinal fluid and a small pocket of subretinal fluid. The patient was educated on the importance of strict blood pressure control and a referral was made to her primary care doctor for further blood pressure management. The patient was scheduled for a retina consultation within one week.
RAMs result from a focal weakness in the arterial wall, which is believed to be the combined result of aging and atherosclerosis. It is thought that arteriosclerosis leads to vessel wall fibrosis. The resulting decrease in wall elasticity, combined with elevated luminal pressure results in aneurysmal dilation.1 Because the arteries are high flow vessels, when the aneurysm ruptures, it does so under significant pressure, pushing blood into many retinal layers.1 Often the macroaneurysm can have spontaneous pulsations.
 |
| Fig. 3. Fundus autofluorescence reveals hypofluorescence corresponding to the areas of the hemorrhage seen clinically. |
RAMs typically occur in women after the sixth decade of life. They are usually unilateral and most commonly associated with systemic hypertension. They may remain unchanged for a period of time, but most will spontaneously resolve.
On fundus examination, there will be aneurysmal dilation of an arteriole, usually superotemporally, at an arteriovenous crossing. The presence of blood at multiple layers, including the preretinal, intraretinal, subretinal and sub-ILM spaces and the vitreous, is a classic finding. Exudation may also be present, usually seen in a circinate pattern surrounding the aneurysm. However, exudation may also be found in the macular region. Macroaneurysms are frequently associated with other ocular conditions including retinal vascular occlusions and retinal emboli.2
 |
| Fig. 4. Fundus photo of the right eye showing improvement in retinal hemorrhaging but increased exudation. |
Fluorescein angiography can help visualize macroaneurysms, which typically fill in the early arterial phase, and staining of the vessel walls with possible leakage may be found in later phases. In cases where hemorrhage blocks visualization of the aneurysm and imaging with fluorescein angiography is inconclusive, indocyanine green (ICG) may be more useful.1 OCT is beneficial to diagnose and monitor associated retinal edema that may be present.
Management
Many treatments exist for RAM, yet no established treatment protocol has been determined. Treatment of this condition is dependent upon macular involvement and threat of vision loss. For the majority of cases, gradual thrombosis, fibrosis and spontaneous involution occurs. For this reason, most patients can safely be observed. In all patients with this diagnosis, a systematic work-up for hypertension and systemic vascular disease should be pursued.
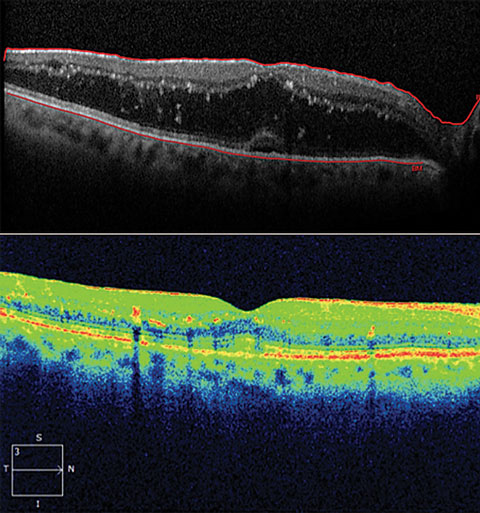 |
| Fig. 5. Above, OCT at presentation showing macular edema. Below, OCT one month after focal laser photocoagulation with improvement in edema. |
Indications for focal laser treatment include vision loss due to chronic macular exudates or edema. Laser photocoagulation directly to, or around, the macroaneurysm can improve vision in some patients.3 Laser photocoagulation may be performed directly to the macroaneurysm with intent to speed involution and decrease leakage. Indirect laser may be applied to the adjacent retina with aim to stop or decrease leakage progression toward the macula. Some complications to focal laser therapy include retinal hemorrhage, laser-induced retinal damage or epiretinal membrane formation.
Recently, investigators have studied intravitreal injections of anti-vascular endothelial growth factor (VEGF) as a treatment option for RAM with macular edema. These injections are used to reduce VEGF-associated increased vascular permeability and dilatation of the retinal artery.4 In patients where a non-clearing vitreous hemorrhage is present, consider a pars plana vitrectomy. This decision is made typically after three months of observation.1
Visual prognosis is favorable in most patients with RAM, and observation alone is typically adequate treatment. However, in cases of macular threat, treatment options are available and referral to a retinal specialist is indicated. Accurate diagnosis and comanagement are crucial to save vision and help prevent complications from uncontrolled hypertension.1
 |
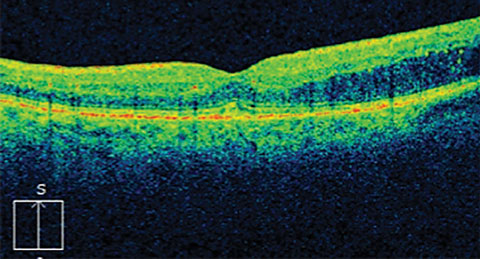 |
| Fig. 6. Above, OCT of the right eye showing exudates with resolution of fluid. Fig. 7. Below, this OCT shows the recurrence of fluid superior to the fovea. |
Our patient was seen by the retina service a few days after the initial presentation. The decision was made to perform focal laser, due to the extent of macular involvement. One month after laser photocoagulation, the patient’s visual acuity improved to 20/40 OD. Fundus photos and OCT were also obtained at that visit (Figures 4 and 5).
The patient returned for a three-month follow-up visit. At this visit, visual acuity was stable at 20/40 OD. Another OCT was performed showing more improvement in the macular edema, although many exudates still present (Figure 6).
Another three months later, the patient presented with a stable visual acuity of 20/40 OD. OCT was performed showing recurrence of fluid superior to the macular threatening the fovea (Figure 7). Another round of focal laser was performed. The patient will continue to be followed approximately every three months until resolution.
Dr. Diamantakos is a resident at Bascom Palmer in Miami.
|
1. Speilburg AM, Klemencic SA. Ruptured retinal arterial macroaneurysm: Diagnosis and management. Journal of Optometry. 2014;7(3):131-7. 2. Pitkanen L, Tommila P, Kaarniranta K, et al. Retinal arterial macroaneurysms. Acta Ophthalmol. 2014;92:101–4. 3. Rabb MF, Gagliano DA, Teske MP. Retinal arterial macroaneurysms. Surv Ophthalmol. 1988 Sep-Oct;33(2):73-96. 4. Golan S, Goldenberg D, Goldstein M. Long-term follow-up of intravitreal bevacizumab in retinal arterial macroaneurysm: a case report. Case Reports in Ophthalmology. 2011;2(3):387-91. |

