 |
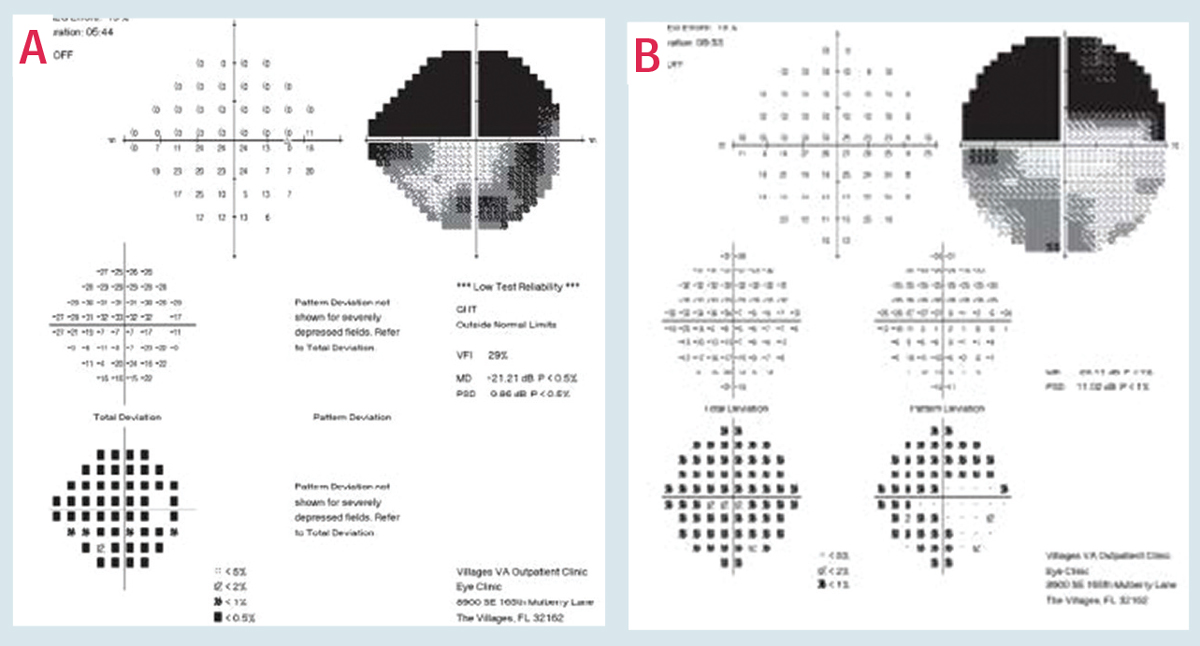
| BCVA, beta-peripapillary atrophy area/disc area ratio and antihypertensive drug usage are among the risk factors for glaucomatous central visual field loss, study shows. Photo: Austin Lifferth, OD. Click image to enlarge. |
Researchers recently identified several risk factors for further central visual function deterioration in eyes with advanced glaucoma. The prospective, observational five-year study included 175 patients with advanced glaucoma and well-controlled IOP (mean age 64.1, baseline IOP 13.2mm Hg). All patients had a mean deviation of HFA 24-2 that was ≤ -20dB and BCVA ≥20/40.
The researchers performed HFA 10-2 testing and BCVA exams every six months and HFA 24-2 every 12 months for five years. They defined deterioration on HFA 10-2 as the presence of the same ≥3 points with negative total deviation slope ≤-1dB/year at p<0.01 in ≥3 consecutive tests. Deterioration on HFA 24-2 results was defined as an increase of ≥2 consecutive tests. BCVA deterioration was defined as an increase of ≥2 logMAR in ≥2 consecutive tests.
The researchers reported a mean IOP of 13mm Hg during the follow-up period. They calculated the probabilities of deterioration in HFA 10-2 and 24-2 as 0.269±0.043 and 0.173±0.031, respectively, and in BCVA as 0.194±0.033 at five years. They noted that lower BCVA at baseline was significantly associated with further deterioration of HFA 10-2 results. Additionally, better mean deviation of HFA 24-2 results and systemic antihypertensive agent use were significantly associated with further deterioration of HFA 24-2 results. Greater beta-peripapillary atrophy area/disc area ratio, systemic antihypertensive agent use and lower BCVA were significantly associated with further BCVA deterioration.
“The main goal of treatment of patients with advanced glaucoma is the maintenance of vision-related quality of life over the course of a lifetime,” the authors wrote. “In glaucoma, the central VF is generally maintained until late in life, and the VF within 5° of the center and the central VA is thought to be especially important for vision-related quality of life in glaucoma patients.” They reported that over the course of five years, 26.9% of eyes showed deterioration of VF within the central 10° and 19.4% of eyes had visual acuity deterioration due to glaucoma progression. This resulted in blindness in 4.6% of eyes.
“A lower visual acuity indicates that the most central VF was already severely damaged,” they noted in their paper. “The low visual acuity in advanced glaucoma may be used as a simple indicator for further deterioration of the severely damaged central 10° VF in clinical practice.”
They pointed out that the existing literature on HFA 24-2 mean deviation value at baseline as a risk factor for further deterioration of the disease shows conflicting results. “A higher baseline HFA 24-2 mean deviation may simply have made detection of further worsening of the HFA 24-2 visual field possible,” they wrote. “Such worsening may not be detectable in eyes with nearly extinguished HFA 24-2 visual fields at baseline, resulting [in] poor sensitivity for detecting further change.”
Additionally, the researchers noted that their well-controlled glaucoma study population (mean IOP 13mm Hg) showed HFA 10-2 deterioration if associated with lower diastolic blood pressure, which they said is compatible with reports that low diastolic blood pressure—especially during the nighttime—is a risk factor for normal tension glaucoma progression.
They concluded that BCVA, beta-peripapillary atrophy area/disc area ratio and use of systemic antihypertensive agents were significant predictors for further central visual function deterioration in patients with advanced glaucoma and well-controlled IOP. They recommend considering medical history of hypertension when managing advanced glaucoma.
Sugisaki K, Inoue T, Yoshikawa K, et al. Factors threatening central visual function of advanced glaucoma patients: a prospective longitudinal observational study. Ophthalmology. December 7, 2021. [Epub ahead of print]. |

