 |
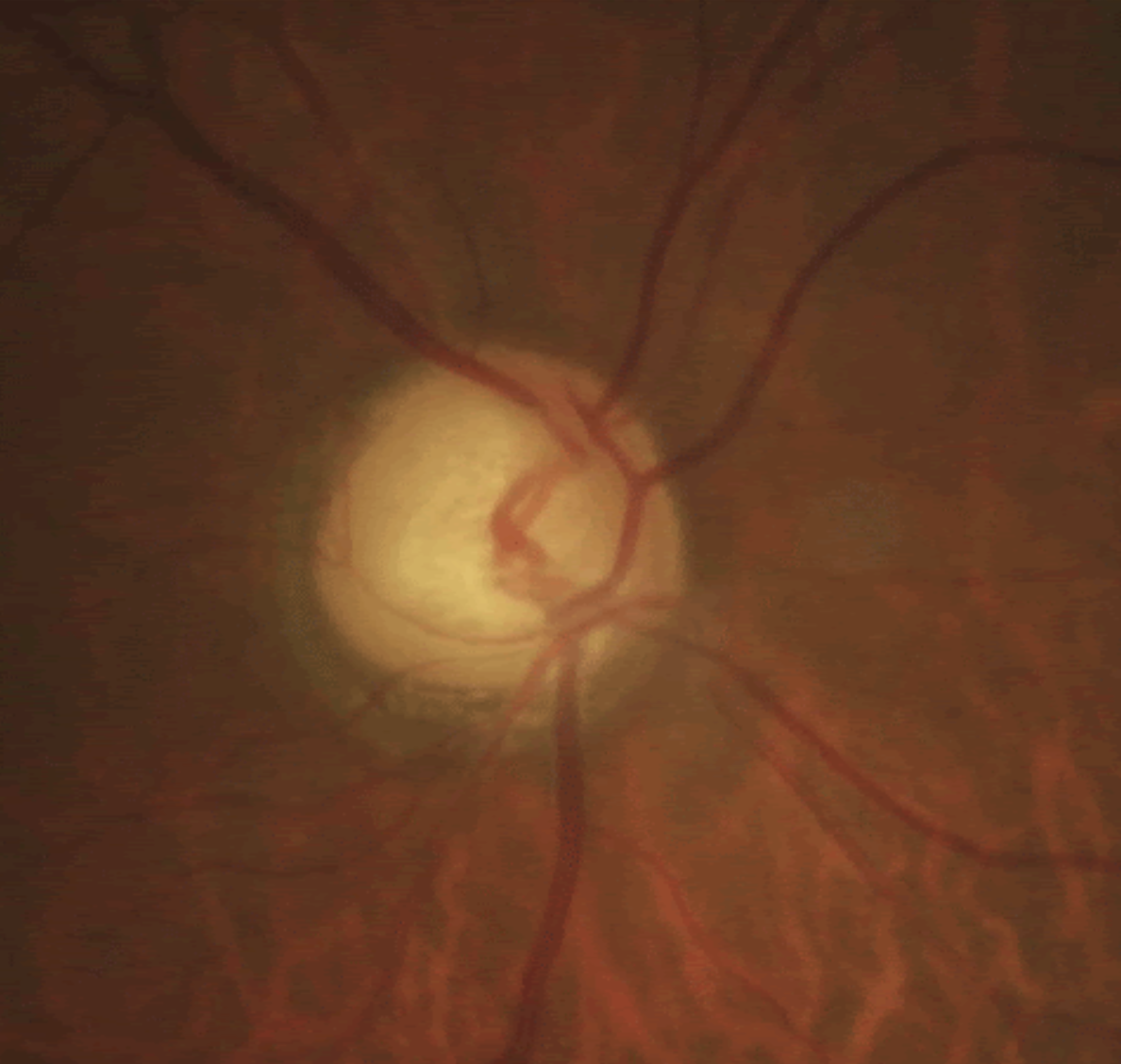
| Glaucoma and Alzheimer's may share more in common than previously thought. Photo: Justin Cole, OD, and Jarett Mazzarella, OD. |
A recent review study of glaucoma and Alzheimer’s disease (AD) imaging biomarkers suggests that the two diseases share a number of pathogenic mechanisms and that glaucoma should be considered a neurodegenerative condition affecting the entire visual system.
“Several studies reported that the selective damage of neuronal populations, as well as the trans-synaptic degeneration and other common mechanisms of cell injury and death characterizing glaucoma, resemble those of other neurodegenerative diseases,” the authors wrote in their paper. MRI has been key for identifying such degeneration.
“Evidence of a possible connection between AD and glaucoma emerged because patients with AD showed a significantly higher rate of glaucoma occurrence,” they wrote. “Despite lower mean IOP, patients with AD showed a five-fold increase in glaucoma compared with matched controls. Relatedly, a significant percentage of patients with AD reports clinical features similar to those found in glaucoma, including ON degeneration and loss of RGCs. Nevertheless, it’s uncertain whether the clinical correlation between these conditions is caused by shared risk factors or if one disorder may have an influence on the other.”
The authors noted connections and possible associations in their review between these two chronic, age-related diseases, including:
Both glaucoma and AD affect ocular and brain tissue of similar embryological origin.
Apolipoprotein metabolism alterations may play a significant role in both diseases.
Both diseases may share an underlying vascular component.
Vascular deposits of A-beta may be a possible common pathway.
Significantly lower levels of A-beta (1-42) and higher levels of tau proteins were found in the vitreous of glaucoma patients compared with non-glaucomatous controls with macular holes.
Both glaucoma and mild AD patients demonstrated impaired cognition compared with healthy controls.
Ocular hypertension may induce A-beta deposition in the retina, leading to progressive synaptic dysfunction and visual impairment.
Ventricular widening was identified as a strong neuroimaging biomarker for AD in the review. The authors also pointed out that automated cortical and subcortical segmentation and volumetric tools are now available and have the advantage of reducing interobserver variability. Additionally, advanced models such as the neurite orientation dispersion and density imaging model have shown important structural changes in AD patients. The authors noted that functional MRI seems to have moderate to high diagnostic power for distinguishing AD from mild cognitive impairment patients.
“So far, the gold standard for the neuroimaging diagnosis of AD is strictly related to MR volumetry and, in particular, to the detection of brain atrophy in the medial temporal lobe (and especially in the hippocampus, amygdala and entorhinal area),” the authors explained in their paper. “However, novel deep learning approaches able to employ T1-w images have been demonstrated to deliver extremely high performance in the diagnosis of AD and also predict mild cognitive impairment-to-AD conversion.”
The authors noted that many of the imaging alterations in glaucoma patients are similar to those in AD patients. “There’s robust evidence that glaucoma patients have microstructural alterations in brain areas not directly linked to the visual pathway,” they wrote. “Specifically, advanced MR imaging methods documented ultrastructural changes in the corticospinal tract, the anterior thalamic radiation and the superior longitudinal fascicle of glaucomatous patients. A whole-brain structural and functional reorganization of both visual and nonvisual areas has been recently suggested. This involves brain areas related to motor control, cognitive and emotive functions. Overall, the results of these studies suggest that the extent of structural and functional alterations extends in areas beyond the visual pathway and are likely connected to abnormalities along white fibers and the brain network.”
“Although an etiopathological connection between glaucoma and AD may exist, as suggested by the commonly involved brain areas and other visual ones (e.g, temporal lobes), the link between AD and glaucoma isn’t yet fully understood and reports are still conflicting,” the authors wrote.
They hypothesized that the thickness reduction of retinal fibers and thinning of optic nerve fibers in glaucoma might result in “a reduction of the cortical thickness and atrophy in specific brain areas involved and not in visual-perceptive functions or in particular areas involved in the emotional processing of images located in the temporal lobes, which are mainly affected by the AD.”
They said that further studies will be key for considering new noninvasive markers, testing the efficacy of neuroprotective molecules and for earlier detection and diagnosis of both diseases.
Martucci A, Picchi E, Di Giuliano F, et al. Imaging biomarkers for Alzheimer’s disease and glaucoma: current and future practices. Curr Opin Pharma 2022;62:137-44. |

