 |
A 42-year-old black male presented to the eye clinic at the Miami Veterans Affairs Medical Center for his annual eye exam. At his last exam, one year earlier, his ocular history was significant for myopia.
The patient reported an episode of severe head trauma seven months prior to this exam. The head trauma resulted from being badly beaten during a mugging. This left the patient in a coma for two weeks followed by a six-week stay in the hospital.
He was subsequently released to the Miami VA Medical Center for rehabilitation. The patient reported suffering short-term memory loss and was experiencing numbness in his right hand.
Visual acuity was 20/20 O.U. with -1.75D sphere O.D. and -2.00D sphere O.S. Confrontation visual field testing revealed a superior nasal defect in the right eye and a superior temporal and nasal defect in the left. Pupils were equally round and reactive with no relative afferent pupillary defect. Extraocular movements revealed no restrictions in either eye. Cover testing showed orthophoria.
The anterior segment exam was unremarkable. Intraocular pressure measured 18mm Hg O.D. and 17mm Hg O.S.
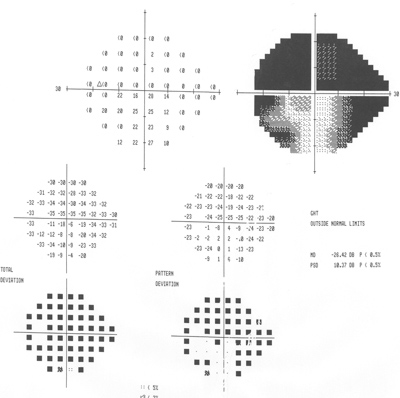
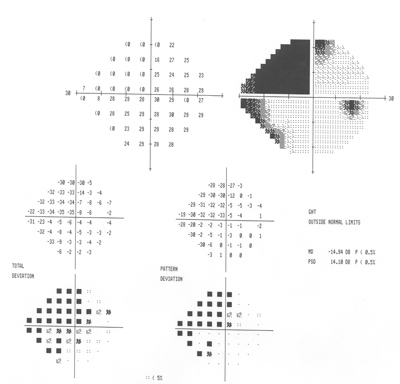
A Humphrey visual field exam showed a dense superior nasal defect in the right eye along with an inferior nasal edge defect. A dense superior altitudinal defect, an inferior temporal edge defect and an inferior nasal step-like defect were present in the left eye. The results are shown in figures 1 and 2.
 |
 |
|
1, 2. Humphrey visual fields (O.D. left, O.S. right) show extensive visual field loss. |
 |
 |
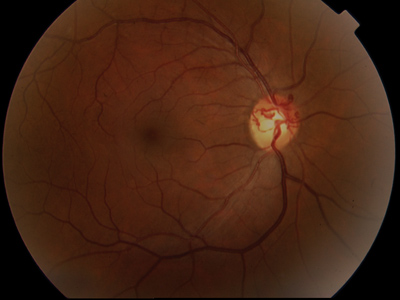
| 3, 4. The optic nerves of our patient (O.D. left, O.S. right). Note the changes seen especially in the right optic nerve. |
1. What do the abnormal vessels seen within the optic nerve of the right eye most likely represent?
a. Neovascularization of the disc.
b. Optociliary shunt vessels.
c. Normal branches of the central retinal artery and central retinal vein.
d. Arteriovenous malformation.
2. What is the most probable etiology of the abnormal vessels within the disc?
a. Diabetes.
b. Glaucoma.
c. Optic nerve sheath meningioma.
d. Resolved papilledema.
3. The visual field defects in the right are most likely the result of:
a. Glaucoma.
b. Brain damage.
c. Ischemic optic neuropathy.
d. Optic neuritis.
4. The visual field defects in the left eye are most likely the result of:
a. Glaucoma.
b. Non-glaucomatous optic nerve atrophy.
c. Brain damage.
d. Both b and c.
For answers, see bottom of page.
Discussion
The anomalous blood vessels on the right optic nerve represent optociliary shunt vessels. Optociliary shunt vessels can be found with glaucoma, optic nerve sheath meningioma, optic nerve drusen and papilledema, or may form after a central retinal vein occlusion. Our patient had no clinical evidence of an old CRVO or optic nerve drusen. He had normal IOP, and his cup-to-disc ratios did not appear exceedingly large. Also, his cup-to-disc ratios were unchanged from his examination of one year prior.
A careful review of the patients medical record revealed that his head trauma resulted in a right subdural hematoma. While in his coma, he underwent surgery for a right frontotemporal craniotomy with evacuation of the subdural hematoma. Following the craniotomy, the patient required a left ventriculotomy due to intraventricular hemorrhage.
A hematoma raises intracranial pressure (ICP), which affects the subarachnoid space around the optic nerve sheath. This, in turn, results in congestion of the venous system and consequent swelling of the optic nerve. Our patient likely developed papilledema as a result of the ICP. Papilledema, by definition, represents bilateral optic disc swelling due to increased ICP, but it occurs in 50% to 75% of patients with chronic subdural hematoma.1
Optociliary vessels are dilated pre-existing capillaries that develop during papilledema to connect the retinal venous system to that of the choroid, thereby bypassing the compromised central venous outflow. Our patient was in a coma during the acute stage of papilledema.
The disc edema subsequently resolved once the hydrocephalus was surgically managed. His optic nerve appearance now represents post-papilledema optic atrophy. Although there is no disc edema, there is temporal disc pallor in each eye, and the optociliary shunt vessels remain in his right optic nerve.
Despite the history of subdural hematoma, we needed to rule out optic nerve sheath meningioma. Optic nerve sheath meningiomas are benign tumors that arise from the meningothelial cap cells of the arachnoid villi.2 The most common feature of optic nerve sheath meningiomas is visual impairment, and the most common signs are disc swelling, disc atrophy, and optociliary shunt vessels. The patient underwent a computed tomography scan and magnetic resonance imaging of the head and orbits with and without contrast. These scans excluded optic nerve sheath meningioma.
The CT scan and MRI of the patients head also revealed brain atrophy in the right temporal and occipital lobes. The left superior quadranopsia on the Humphrey visual field is due to the right temporal lobe atrophy. The bilateral left inferior field defects likely represent the atrophy of the right occipital lobe.
The left eye shows much greater visual field loss than the right. The additional field defects in the left eye are not homonymous (due to a prechiasmal lesion) but are likely a result of the optic atrophy. Even though the right optic nerve has the optociliary shunt vessels, the left eye shows much greater optic nerve head pallor.
I found it odd that the optociliary shunt vessels were present in only one eye, even though papilledema must be bilateral, but this finding is actually not that rare. A study revealed seven patients who developed papilledema for various reasons.3 Four of the seven patients developed optociliary shunt vessels in just one eye, while the other three developed optociliary shunt vessels bilaterally. Considering the extensive field damage and optic atrophy in the left eye as compared to the right, you could argue that the optociliary shunt vessels were protective in this case.
Despite the visual field loss, the patient has done well visually, as he maintains 20/20 central visual acuity in each eye. He is also stable from a neurological standpoint, but he does suffer from reduced function due to extensive temporal lobe atrophy.
Megan Hunter, O.D., of the Miami VA Medical Center, wrote this case.
1. Duke-Elder S, Scott GI. Neuro-ophthalmology. Vol 12. St. Louis: CV Mosby, 1971:39.
2. Saeed P, Rootman J, Nugent RA, et al. Optic nerve sheath meningiomas. Ophthalmology 2003 Oct;110(10):2019-30.
3. Eggers HM, Sanders MD. Acquired optociliary shunt vessels in papilloedema. Br J Ophthalmol 1980 Apr;64(4):267-71.
Answers: 1) b; 2) d; 3) b; 4) d.

