For a structure only half a millimeter thick, there are a wide variety of problems that can arise in the cornea. Most of these pathologies can be grouped into one of six categories: injury, inflammation, infection, dysplasia, degeneration or deposition.
KMK Optometry has helped 98% of optometry students nationwide prepare for their board exams since 2010, and this month we’re going to fine-tune your cornea differential diagnosis skills in particular. Below are some of our favorite cases with photos from our Instagram page that represent a few of the pathology groups mentioned above for you to test your knowledge. Have fun and good luck! Answers to all questions appear at the conclusion of this article.
Case One
A 55-year-old woman was referred from the emergency room with gradually worsening vision over the previous week in her left eye with increasing light sensitivity and a headache. Her history included cataracts, LASIK surgery in 2006 and herpes zoster ophthalmicus in 2019. She noted she had experienced recent stress due to being furloughed. Her vision was 20/50 in the left eye. Her exam findings were notable for 1+ anterior chamber cell and the corneal findings seen in the photo.
Corneal Findings1. What is your tentative diagnosis?
a. Corneal hydrops from post-LASIK ectasia.
b. Recurrent zoster keratitis.
c. Salzmann’s nodular degeneration.
d. Diffuse lamellar keratitis.
2. Which treatment is most appropriate?
a. Corneal crosslinking.
b. Superficial keratectomy.
c. Oral valacyclovir and topical prednisolone.
d. Flap lift with irrigation.
e. Topical gancyclovir.
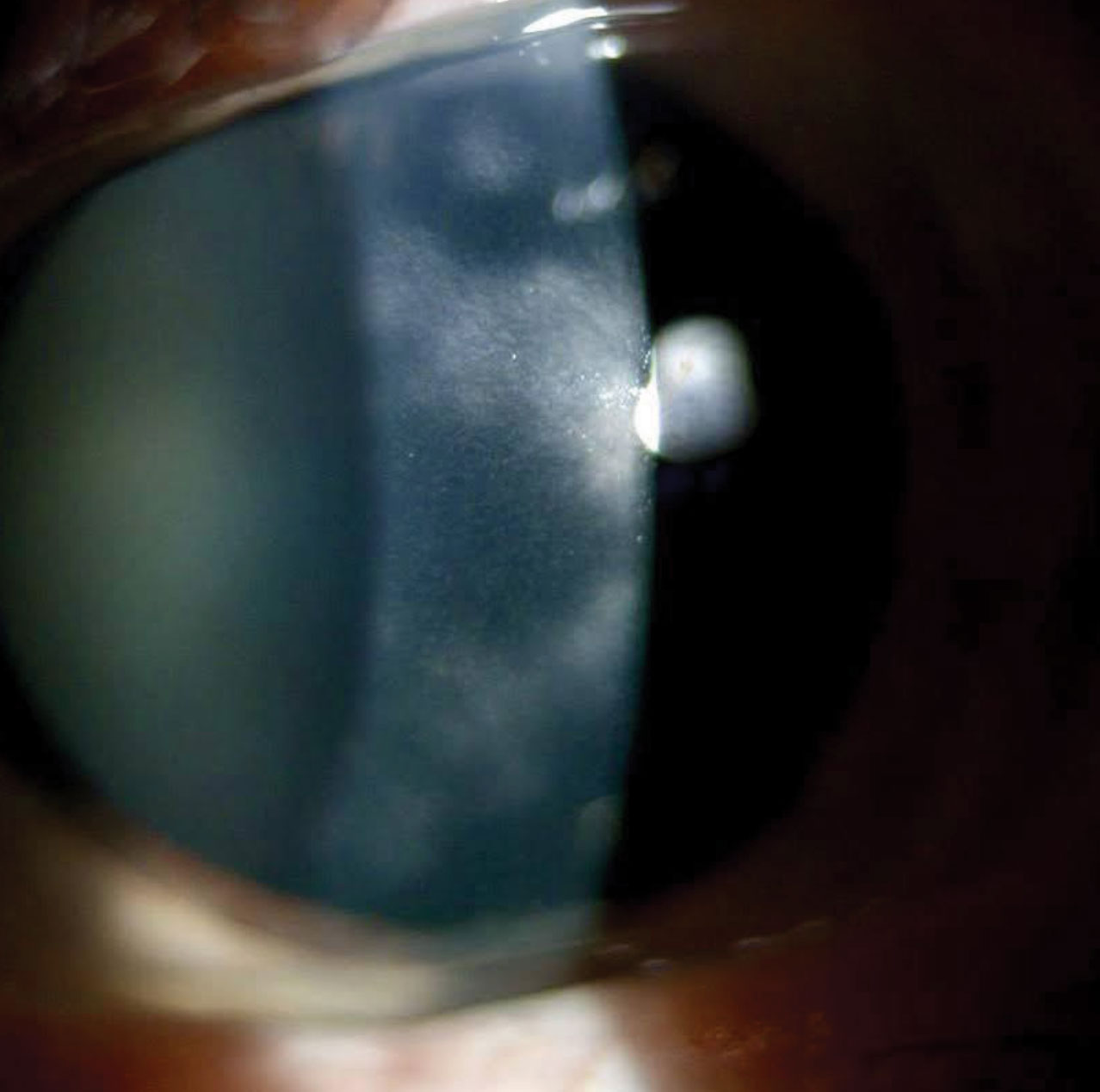 |
Case 1. This patient’s cornea showed diffuse patches of intrastromal haze. Click image to enlarge. |
Discussion
Interstitial keratitis is an infectious condition that affects the stromal layer of the cornea and most commonly arises from the herpes simplex virus or the varicella zoster virus, sometimes triggered by stress or fatigue. The treatment is similar for both viruses, involving oral antivirals to inhibit viral replication and topical steroid eye drops to reduce the inflammatory response to the viral antigens. Recurrence can be common as seen with this patient, as well as visually debilitating; herpetic keratitis is one of the leading causes of corneal scarring.
Case Two
Referred from a local optometrist for “corneal thinning,” this patient thought her eyes were perfectly healthy other than having a higher than average amount of astigmatism. She had no pain, redness or tearing, and best-corrected visual acuity (BCVA) was 20/20 OD and 20/25 OS with against-the-rule 1.5D of cylinder OD and 3.5D of cylinder OS. On slit lamp exam, there was paralimbal corneal thinning with neovascularization and lipid deposits bilaterally, most prominent superiorly and inferiorly, and the epithelium was intact.
Corneal Findings
3. What is your tentative diagnosis?
a. Pellucid marginal degeneration.
b. Peripheral ulcerative keratitis.
c. Terrien’s marginal degeneration.
d. Furrow degeneration.
4. Which treatment is most appropriate?
a. Corneal crosslinking.
b. Bandage contact lens, topical moxifloxacin and oral vitamin C.
c. Culture.
d. Observation.
e. Amniotic membrane graft.
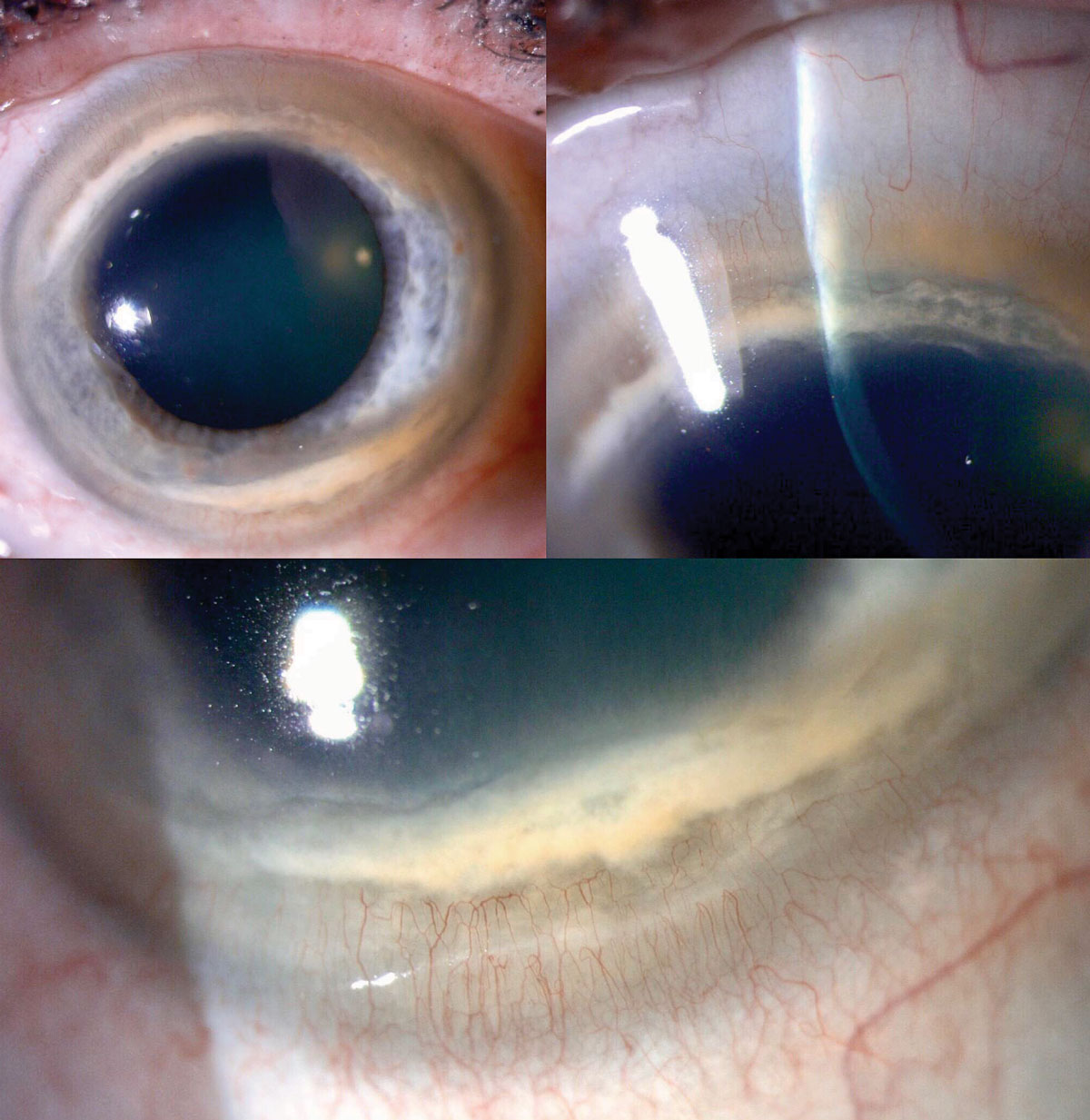 |
Case 2. Slit lamp exam showed paralimbal corneal thinning with neovascularization and lipid deposits bilaterally. Click image to enlarge. |
Discussion
Given the lack of inflammation in this case, the presence of peripheral thinning greatest superiorly and inferiorly accompanied by lipid and neovascularization, the diagnosis of Terrien’s marginal degeneration was made. This condition is slowly progressive, causing high levels of against-the-rule astigmatism—usually bilaterally—resulting in normal to mildly reduced visual acuity depending. Vision is usually well-corrected with glasses or scleral contact lenses, and serious complications like spontaneous perforation are quite rare, usually associated with ocular trauma.
This patient was content with her glasses, deferred a scleral lens consult and was referred back to her OD for yearly monitoring.
Case Three
This female patient had a history of severe trauma 20 years prior, necessitating vitrectomy, scleral buckle, scleral-fixated IOL and a trabeculectomy, which had scarred down. She was currently taking four different glaucoma drops and had no pain, but vision had gradually declining over the last year along with slight progression of her arcuate (non-central) visual field defects. BCVA was 20/100 with an IOP of 25. There was a diffuse whorling keratitis that picked up NaFl stain, no stromal edema and no inflammation in the anterior chamber.
Corneal Findings
5. What is your tentative diagnosis?
a. Microcystic corneal edema.
b. Rhopressa-associated verticillata.
c. Anterior basement membrane dystrophy.
d. Limbal stem cell deficiency.
6. Which treatment is most appropriate?
a. Tube shunt and discontinue Rhopressa (netarsudil, Aerie).
b. Phototherapeutic keratectomy with Prokera (Bio-Tissue).
c. Descemet’s membrane endothelial keratoplasty (DMEK) and Xen implant (Allergan).
d. Micropulse cyclophotocoagulation and platelet-rich plasma eye drops.
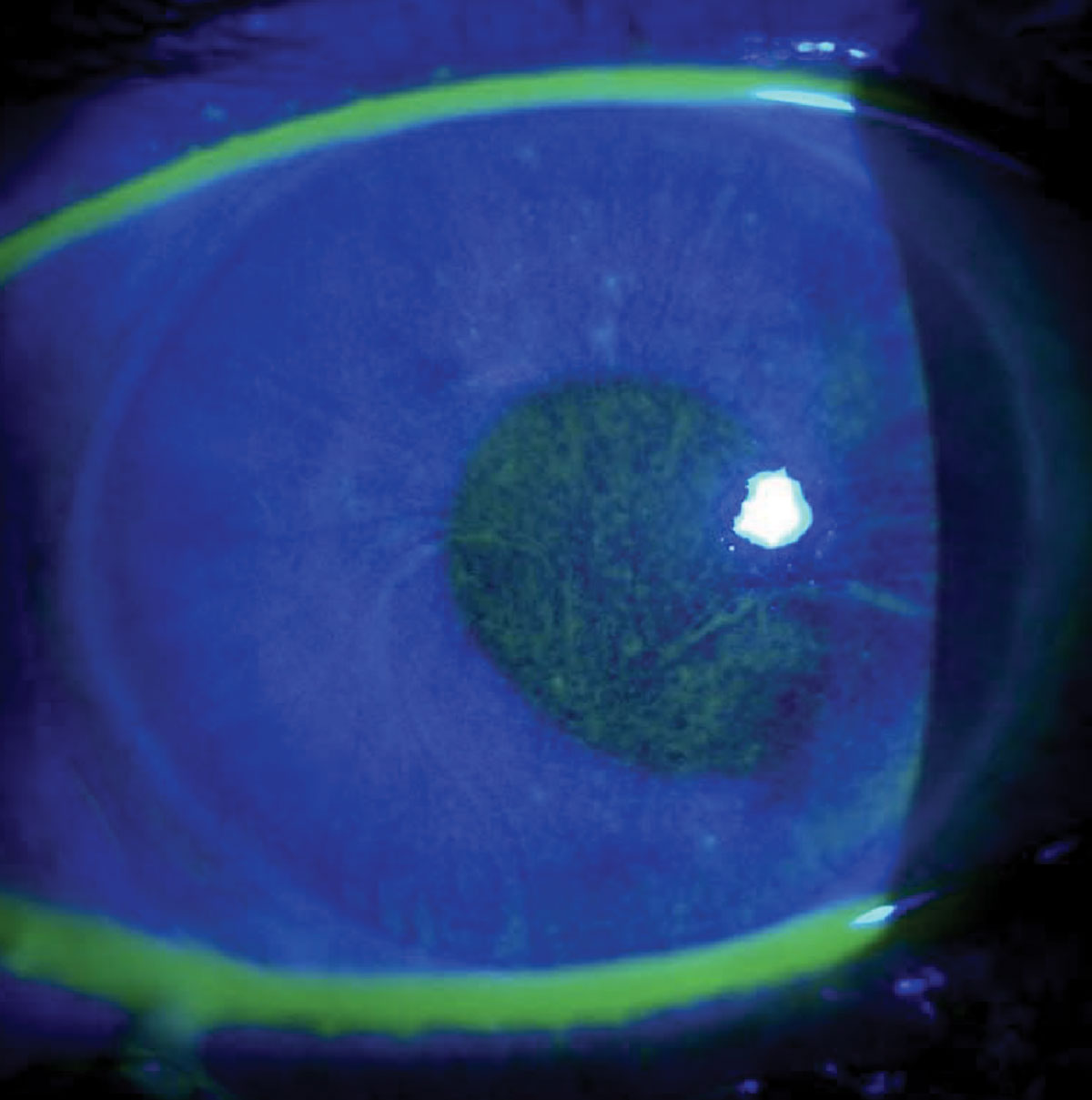 |
Case 3. This patient had uncontrolled IOP and a swirling pattern of NaFl staining. Click image to enlarge. |
Discussion
This patient is in a difficult predicament, with uncontrolled IOP on maximal medical therapy and limbal stem cell deficiency (LSCD) from glaucoma drop toxicity. The swirling pattern is reminiscent of verticillata, but that does not stain with NaFl and rarely affects visual acuity. This LSCD pattern arises from the centrifugal nature of epithelial replication from the palisades of Vogt at the limbus as the cells migrate centrally.
For IOP reduction, it was decided to perform micropulse cyclophotocoagulation to avoid incisional surgery that may further damage the cornea. She was also switched to preservative-free Tim-Brim-Dorz Qam and Tim-Brim-Dorz-Lat eye drops Qhs (Imprimis). Platelet-rich plasma eye drops were formulated at 40% for maximum efficacy and used six times a day.
Fortunately, vision recovered to 20/50 after two months of treatment and IOP improved to the upper teens.
Case Four
This 61-year-old male had not had an eye exam in over 10 years and reported that his vision was not as good as it used to be. His eyes were occasionally dry, but otherwise comfortable. He worked as a roofer and reported smoking a pack of cigarettes per day. He had no history of any ocular surgery or injury. His exam was remarkable for 2+ nuclear cataracts on exam and visual acuity was 20/30. The left cornea had an irregular swath of hazy epithelium without vascularization or ulceration, as documented in the photo.
Corneal Findings
7. What is your tentative diagnosis?
a. Ocular surface squamous neoplasia (OSSN).
b. Atypical pterygium.
c. Salzmann’s nodular degeneration.
d. Limbal dermoid.
8. Which treatment is most appropriate?
a. Topical chemotherapy eye drops.
b. Surgical resection with amniotic membrane graft and mitomycin-C.
c. Superficial keratectomy with amniotic membrane graft.
d. Diamond burr polishing plus bandage contact lens.
 |
Case 4. This patient had an irregular swath of hazy epithelium without vascularization or ulceration in his left cornea. Click image to enlarge. |
Discussion
Sun exposure is a strong risk factor for developing OSSN and this patient was no different. The photograph shows hazy epithelium in an irregular pattern unlike a pterygium or Salzmann’s degeneration. In recent years, topical chemotherapeutic agents such as interferon alpha-2b, mitomycin-C and 5-fluorouracil have gained popularity in their ability to clear OSSN from the conjunctiva and cornea without surgery, and they show superiority in clearing microscopic disease that can be missed with traditional excisional biopsy.
Fortunately, this patient regained a perfectly clear cornea after several rounds of topical interferon drops and is now doing well without signs of recurrence.
Case Five
A 49-year-old female reported a history of recurrent redness in her left eye the last three years, as well as light sensitivity and mild blur as of this spring. She had a history of chalazion removal two years prior, did not wear contact lenses and was already taking ciprofloxacin eye drops from her PCP, which were not helping.
Slit lamp exam showed significant telangiectatic blepharitis, a corneal infiltrate with a leash of superficial neovascularization from the nasal limbus and a smaller-sized epithelial defect overlying the infiltrate. She denied recent travel out of the country and new sexual partners.
Corneal Findings
9. What is your tentative diagnosis?
a. Interstitial keratitis.
b. Phlyctenular keratoconjunctivitis.
c. Vernal keratoconjunctivitis.
d. Recurrent corneal erosion.
10. Which treatment is most appropriate?
a. Laboratory workup and penicillin.
b. Oral cetirizine, topical olopatadine and loteprednol.
c. Debridement, diamond burr polish and bandage contact lens.
d. Oral doxycycline and tobramycin-dexamethasone eye drops.
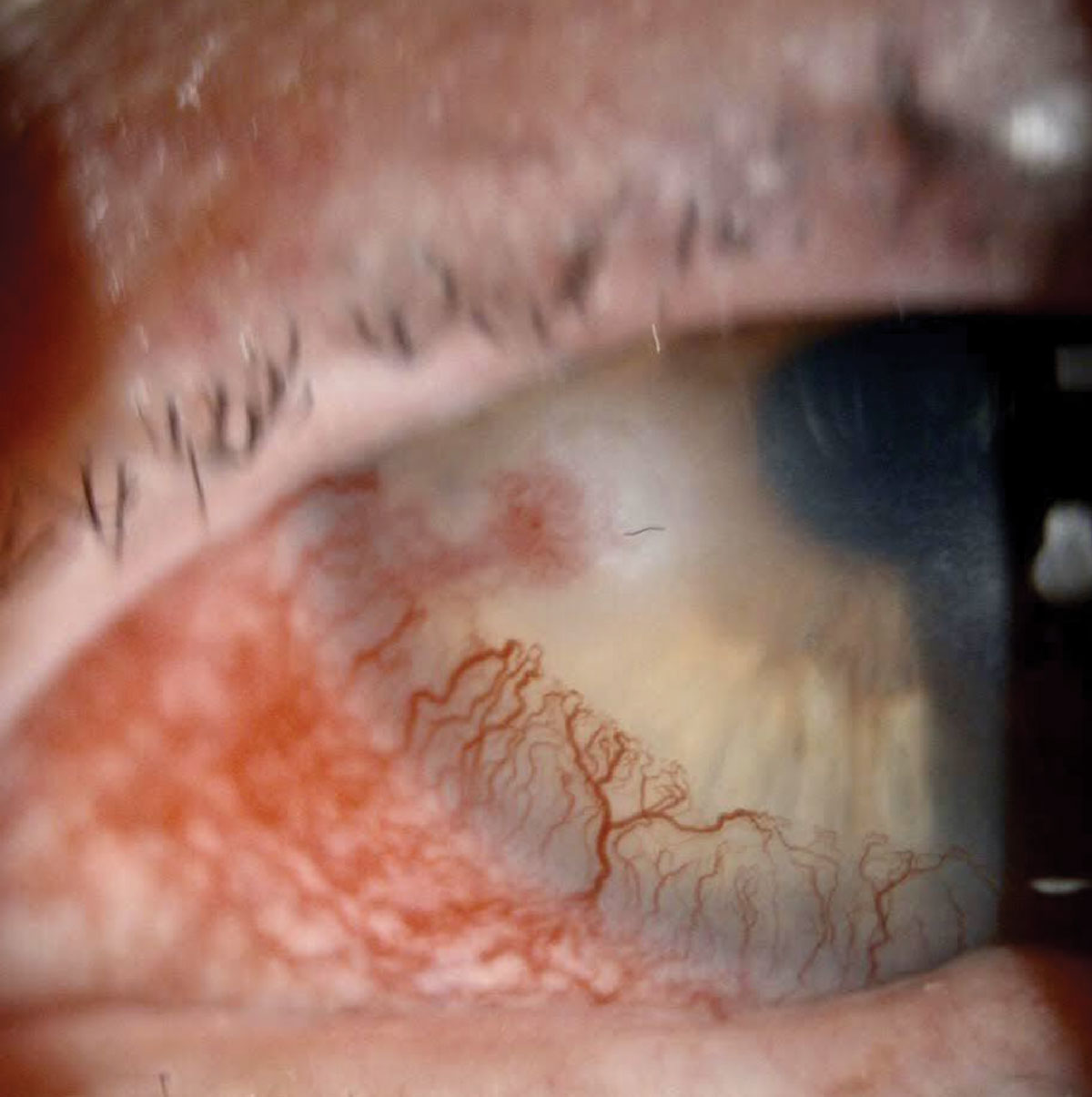 |
Case 5. Slit lamp exam in this patient showed significant telangiectatic blepharitis, a corneal infiltrate with a leash of superficial neovascularization from the nasal limbus and a smaller-sized epithelial defect overlying the infiltrate. Click image to enlarge. |
Discussion
The recurrent nature of the condition, concurrent rosacea blepharitis and classic corneal appearance led to a diagnosis of phlyctenular keratoconjunctivitis. The ciprofloxacin from the PCP was not helpful, as this condition is primarily due to a hypersensitivity reaction, which is inflammatory in nature. Staphylococcal and tuberculosis antigens are the most common causes, and there is often concomitant ocular rosacea noted as well. The recurrent inflammation creates a nodule that can progress centrally across the cornea as what is termed a “marching phlyctenule,” trailed by a leash of superficial neovascularization.
Fortunately, this patient responded very well to treatment with 50% improvement in symptoms in 48 hours and is currently quiescent on prophylactic therapy of cyclosporine 0.05% eye drops and hypochlorous acid 0.02% lid spray.
Case Six
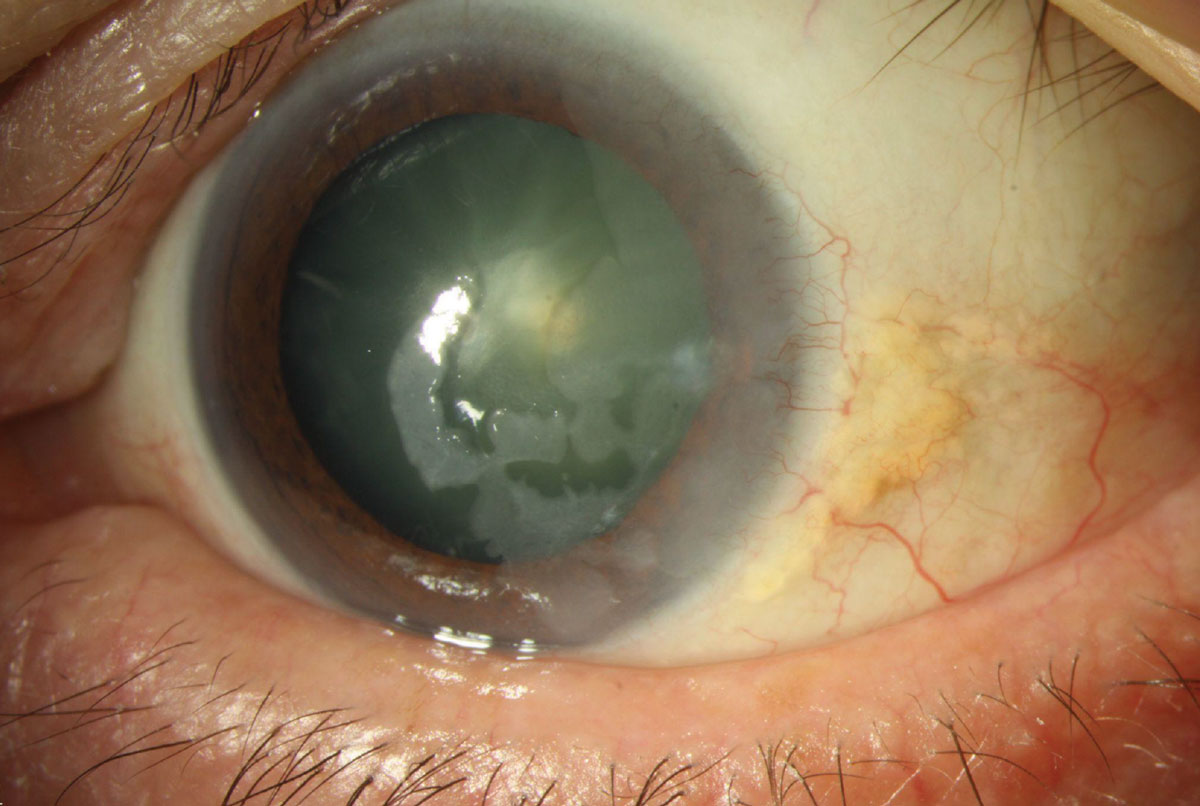
A 59-year-old female came to our clinic reporting recurrent sharp eye pain in the morning in the right eye over the past month. She had penetrating keratoplasty (PKP) in the left eye that was doing well and had not seen an eye doctor for quite some time. Her vision was 20/50 in the right eye and 20/25 in the left eye. She mentioned decreased vision along with worsening glare at night over the last six months in the right eye. There was no inflammation in either cornea, no arcus, no sutures remaining in the transplant and the slit lamp exam revealed the findings in the photograph in the right eye only.
Corneal Findings
11. What is your tentative diagnosis?
a. Schnyder’s dystrophy with recurrent corneal erosions.
b. Infectious crystalline keratopathy.
c. Anterior basement membrane dystrophy.
d. Lattice dystrophy with recurrent corneal erosions.
12. Which treatment is most appropriate?
a. Superficial keratectomy and amniotic membrane.
b. Descemet’s membrane endothelial keratoplasty.
c. Phototherapeutic keratectomy (PTK).
d. Culture and fortified antibiotics.
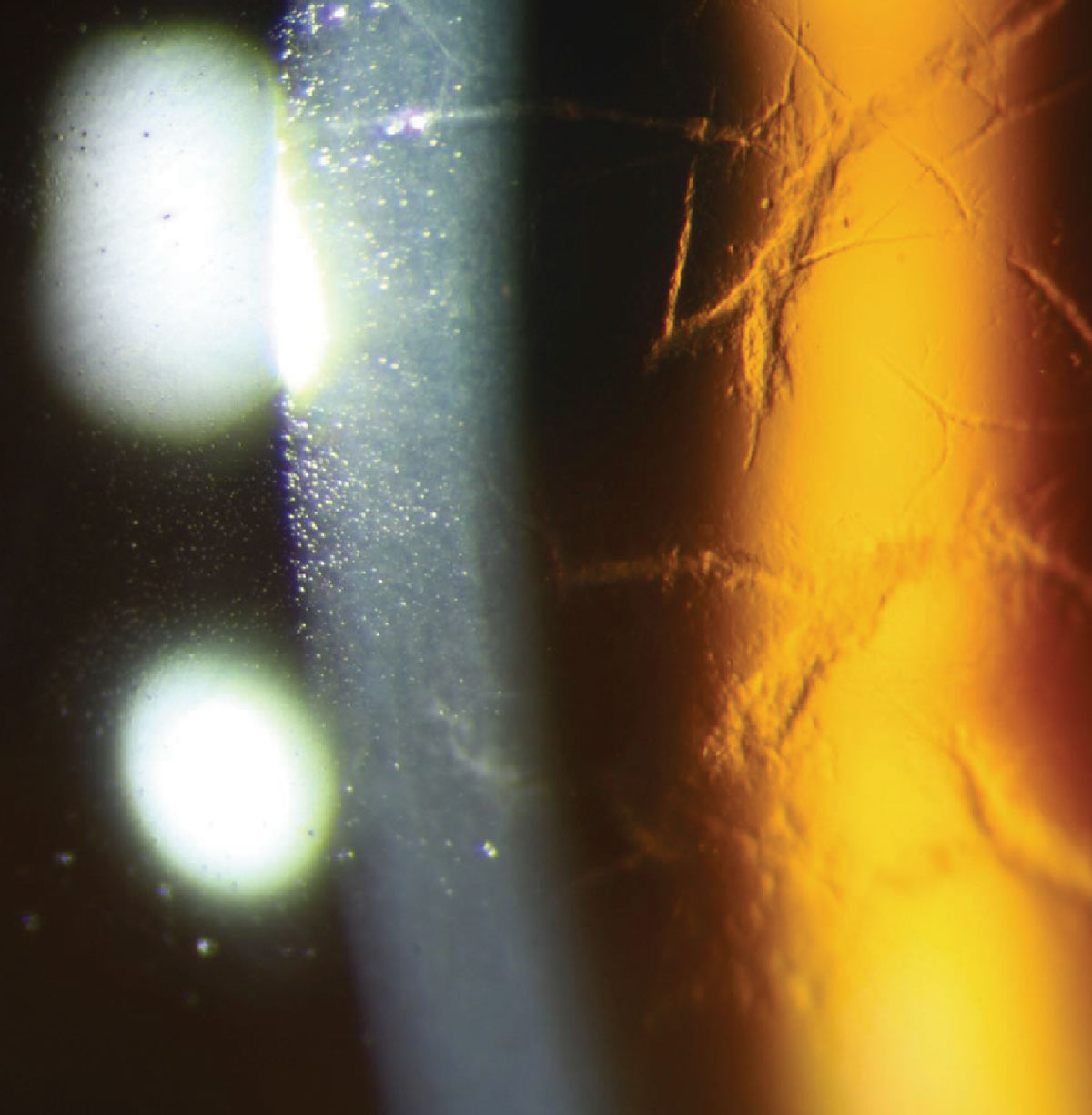 |
Case 6. Notice the glass-like branching lines in the anterior stroma in this patient. Click image to enlarge. |
Discussion
Corneal dystrophies can be difficult to differentiate, but this appearance of glass-like branching lines in the anterior stroma is classic for lattice corneal dystrophy, the most common of the stromal dystrophies. These patients suffer from recurrent corneal erosions, which can be managed medically to start, but often end up undergoing PTK to reduce symptoms and improve vision. The opacities tend to coalesce with age and can impact visual acuity as the central cornea becomes more involved.
Historically, PKP was the surgery of choice to restore vision, but now deep anterior lamellar keratoplasty and PTK are excellent options as well and have gained popularity, given their lower risk profiles. The amyloid deposits can recur both after PTK and in corneal grafts after five to 10 years.
This patient opted for PTK and was educated on the likelihood of family members being affected with an autosomal-dominant inheritance pattern.
Answers1. b2. c 3. c 4. d 5. d 6. d 7. a 8. a 9. b 10. d 11. d 12. c |
Thanks for Playing!
We hope you not only fine-tuned your corneal diagnostic skills but had fun learning about these cases, which we believe can help you assess patients with similar conditions that may make their way to your office.
Check out our Instagram page, @kmkoptometrypro, to see more interesting cases and continue testing your knowledge, and let us know your thoughts!
Dr. Hammond specializes in glaucoma and corneal disease at Twin Cities Eye Consultants in Minneapolis, MN. He is also the co-editor of KMKOptometryPro on Instagram. He is a consultant for Allergan.

