 |
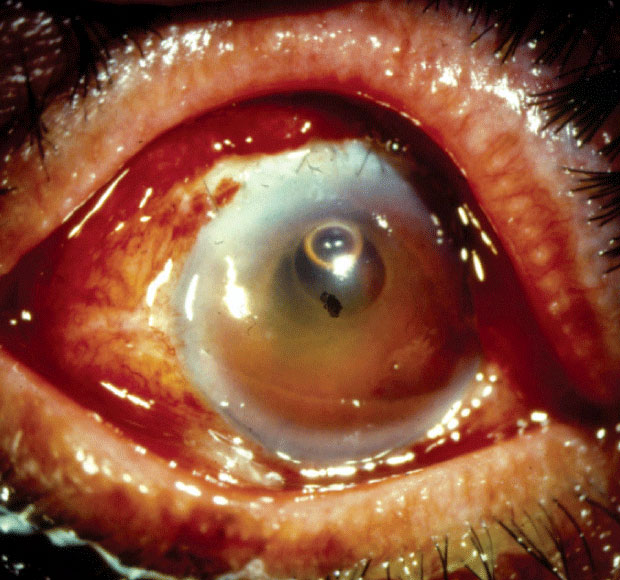
| Patients of older age, male gender or those of Black or Native American race seemed to be at an increased risk for endophthalmitis. Click image to enlarge. |
The potentially devastating surgical complication of endophthalmitis requires immediate treatment in order to save the eye. A recently published retrospective cross-sectional analysis on endophthalmitis rates among Medicare beneficiaries undergoing cataract surgery in the United States reported an incidence rate of 1.36 per 1,000 cataract surgeries over a nine-year period.
The study included 14.4 million cataract surgeries performed on Medicare beneficiaries between 2011 and 2019, obtained from Medicare fee-for-service claims (patients 65 and older). The researchers identified endophthalmitis cases within 90 days of surgery using diagnostic codes. Any patient with a history of endophthalmitis 12 months prior to cataract surgery was excluded from the analysis.
The researchers reported an overall 90-day postoperative endophthalmitis rate of 1.36 per 1,000 surgeries for stand-alone cataract procedures. They also noted a decreasing trend for post-op endophthalmitis rates during the nine-year period.
Patient age, gender and race were influential factors. Surgeries performed on patients 75 years and older had increased risk compared with surgeries on those under 75. Black and Native American patients had increased risk as well, compared with white people. Other increased risk factors for developing endophthalmitis postoperatively included prior history of invasive glaucoma surgery, combined cataract and retinal surgery, and various systemic comorbidities. The risk was also higher among males.
The researchers say they believe the decreased endophthalmitis rate may reflect ongoing improvements in wound construction or the increasing use of intracameral antibiotics. “One of the limitations of an administrative database such as ours is the lack of clinical information that would allow an analysis of such potential factors,” they noted, pointing out that the increase of intracameral antibiotic use was likely tied to the growing body of evidence in favor of it, including a 2013 study in California that supported the multicenter ESCRS trial.
“It’s also possible that a decline in observed endophthalmitis rates reflects changes in billing and/or coding practices and not a true reduction in actual infections,” they said. “Beginning October 2015, the ICD coding system in the United States underwent a complete overhaul.” ICD-10 codes are more detailed and numerous than ICD-9 codes. “The increased number of codes as well as the decreased familiarization with the new coding system may have resulted in some change in case ascertainment in the analysis. For example, we found endophthalmitis rates decreased from 1.7 in September 2015 to 1.3 in October 2015, the beginning of the transition to ICD-10.”
While the study also noted decreasing rates of endophthalmitis among minorities over time, they emphasized the persistence of racial and ethnic disparities in healthcare outcomes. “Black patients have been shown to have higher mortality rates, greater morbidity burden and higher rates of in-hospital complications than white patients,” they said, citing reasons such as lack of access to care, insurance status, socioeconomic status and treatment by low volume or low-quality surgeons. “Further studies exploring racial disparities and surgeon-related characteristics are warranted,” they said.
The researchers noted four published case reports on postoperative endophthalmitis following MIGS, three associated with the Xen implant (Allergan) and one with iStent (Glaukos). “We found 90-day postoperative endophthalmitis rates were higher for cataract cases combined with MIGS than stand-alone cataract procedures (1.76 vs. 1.3 per 1,000 cataract surgeries),” they said. Interestingly, they added, “Although procedures combined with MIGS had a higher postoperative endophthalmitis risk on univariable analysis, the association was reversed on multivariable analysis.”
They attribute this to either a too-small sample size or Simpson’s paradox, a statistical phenomenon when the relationship between two categorical variables is reversed after a third variable is introduced. “Simpson’s paradox has broad implications for epidemiological research since it indicates that making causal inference from a nonrandomized study can be difficult,” they explained. “While it’s possible to control for differences between cases and controls, there will always be the possibility that an unobserved and therefore unadjusted cofounder might attenuate the association (or even reverse its direction) between exposure and outcome, due to the difference in the mean values or the distribution of confounders between the case or control group.”
Though the study was based on billing rather than medical records, the researchers say that age, sex, race and ethnicity continue to be risk factors for endophthalmitis. “Additional studies are warranted to understand disparities in endophthalmitis rates and surgeon factors which may contribute to decreasing endophthalmitis rates,” they concluded.
Zafar S, Dun C, Srikumaran D, et al. Endophthalmitis rates among Medicare beneficiaries undergoing cataract surgery between 2011-2019. Ophthalmology. September 16, 2021. [Epub ahead of print]. |

