 |
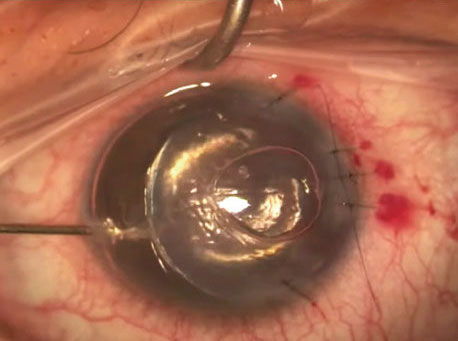
| The nonogram used in this study could adequately predict graft survival probability. Photo: James Lewis, MD. Click image to enlarge. |
Descemet’s stripping endothelial keratoplasty (DSEK) produces excellent results in patients with corneal endothelial dysfunction, but like any transplant procedure, it may be complicated by graft rejection or failure. Much research has gone into identifying the effects of recipient characteristics on DSEK outcomes, but a recently published study in Cornea points out that there haven’t been any studies quantifying the risk of graft failure based on risk factors. The authors developed a nomogram after analyzing DSEK outcomes that would compute the probability of graft survival after three and five years. They say it may be a useful tool for patient education and counseling.
The study took place at a tertiary care center, where the researchers retrospectively analyzed 794 DSEK outcomes from procedures between January 2008 and August 2019. They identified 37 variables. Additionally, they evaluated the data for the presence of graft failure, which they defined as irreversible visually significant graft edema, haze or scarring.
The authors reported that graft failure occurred in 80 of the transplant patients (10.1%). The strongest risk factors for graft failure were graft detachment, prior glaucoma surgery and glaucoma. They also noted that a preoperative diagnosis of Fuch’s dystrophy was associated with a decreased risk of graft failure when compared with secondary corneal edema. Graft rejection occurred in 39 cases (4.9%), and the most significant risk factor for this complication was prior glaucoma surgery.
The risk factors they identified in the study aligned with those reported in previous studies. Graft detachment has been a commonly reported postoperative complication in several studies, as has increased tissue manipulation (e.g., repositioning and rebubbling), which contributes to endothelial cell loss after DSEK. The authors say their nomogram assigns substantial weight to graft detachment when quantifying the risk of graft failure in DSEK.
“This finding highlights the importance of patient positioning and avoidance of risk factors for detachment, such as hypotony and eye rubbing after DSEK surgery,” they noted. They also wrote that the “structural changes in glaucomatous eyes, such as narrow angles and shallow anterior chambers, may contribute to the increased risk of graft failure by placing the donor endothelium in closer proximity to blood vessels and increasing the risk of direct trauma to the corneal endothelium.
“Even more strongly associated with poor DSEK outcomes is prior glaucoma surgery, such as trabeculectomy and shunt placement,” they continued. “According to multiple studies, these procedures can lead to either a breach in the blood-aqueous barrier or endothelial damage, which leads to an influx of oxidative and inflammatory proteins that causes additional corneal endothelial damage and contributes to worse graft outcomes. Our findings underscore the deleterious impact that glaucoma and glaucoma surgery can have on DSEK grafts and the importance of considering these factors when counseling patients before DSEK.”
The authors say their nomogram has a concordance index of 0.75, which means it can predict graft survival probability with “reasonable accuracy.” “Nomograms are a powerful tool with the potential to determine the probability of a given clinical outcome occurring based on a patient’s demographic and clinical characteristics,” they explained in their paper.
“Despite the extensive use of nomograms in [ophthalmology], this is the first nomogram developed that uses pooled patient data to predict the probability of graft survival after DSEK surgery, given various risk factors,” they wrote. “Given its wide-reaching prognostic value and potential utility to clinicians and patients alike, external validation of our nomogram is necessary before more generalized application.”
Cherkas E, Cinar Y, Zhang Q, et al. Development of a nomogram to predict graft survival after Descemet stripping endothelial keratoplasty. Cornea. 2021;00:1-7. |

