 |
| Click image to enlarge. |
After refractive error, dry eye is almost certainly the most common ocular issue you encounter at your practice. Just consider: 16 million Americans have been diagnosed with dry eye disease (DED) and as many as six million symptomatic individuals may go undiagnosed.1 With an ever-expanding roster of exam techniques and treatment options to consider, formulating a plan to manage such a heavy caseload can be a challenge. How is this pervasive problem addressed in optometric offices across the country? We surveyed our readers to get a glimpse.
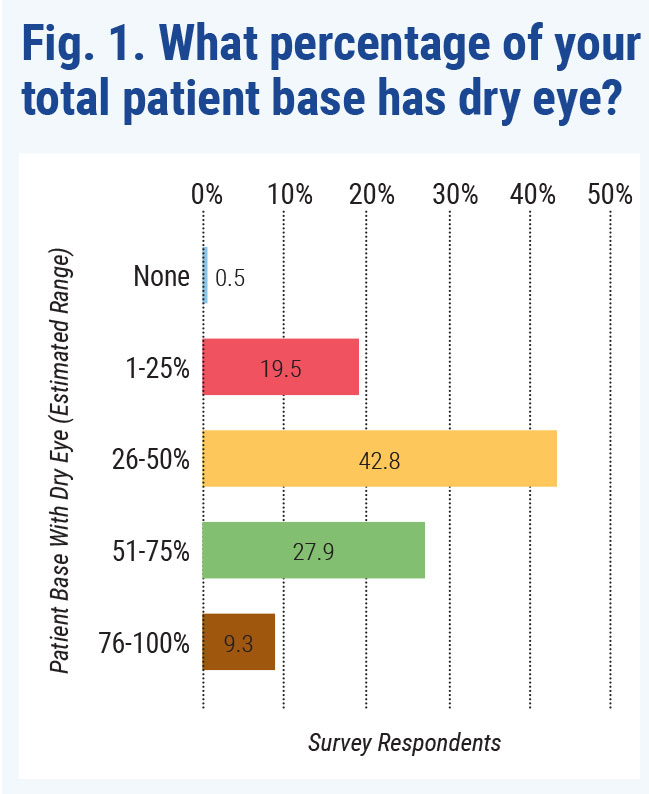
The 215 US optometrists who responded shared their impressions of DED prevalence, diagnostic testing, treatment habits and challenges they encounter managing this condition. Not surprisingly, dry eye is pervasive in their practices, with 70.7% telling us that anywhere from one to three quarters of their patients have symptoms (Figure 1). On the high end, 9.3% of optometrists reported the vast majority of their patients have DED or are suspects.
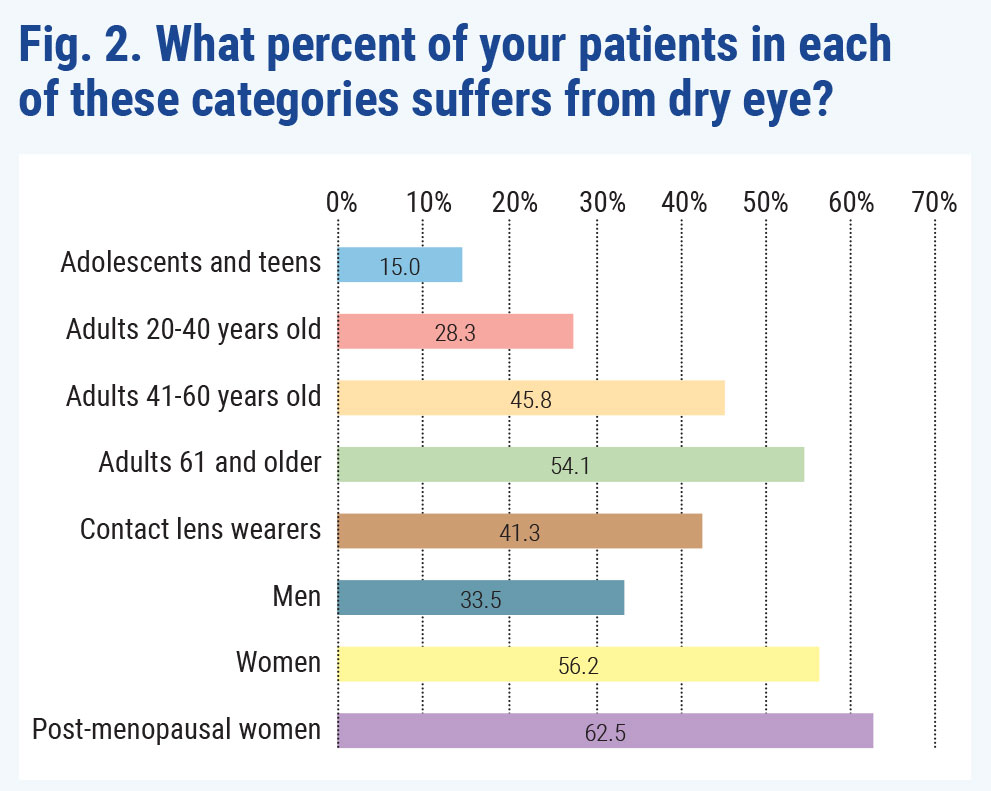
Looking at individual cohorts of patients, there’s clearly an age-related increase in prevalence (Figure 2). Just 15% of teens and kids experience DED, according to our survey respondents; going up in 20-year increments, the footprint of dry eye grows and grows, topping out at 54.1% of adults in the 61-and-older bracket.
 |
| Click image to enlarge. |
Our results also validate studies and anecdotal evidence that women (56.2% ) are more affected than men (33.5%), and post-menopausal women most of all (62.5%).
“Every eye doctor should be screening for signs and symptoms of dry eye disease. It is significantly under-diagnosed,” says one doctor who responded to the survey.
DED is ubiquitous and should no longer be an afterthought, adds Chandra Mickles, OD, associate professor and director of the Dry Eye Care Center at Nova Southeastern University’s College of Optometry.
“Dry eye is one of the most common reasons patients visit eye care professionals, and yet, unfortunately, it is under-diagnosed and untreated. Many patients are suffering from it overtly or in silence,” Dr. Mickles says. “Like other ocular conditions, such as glaucoma and macular degeneration, I believe at least basic competency in this area is our duty and well worth the investment.”
 |
|
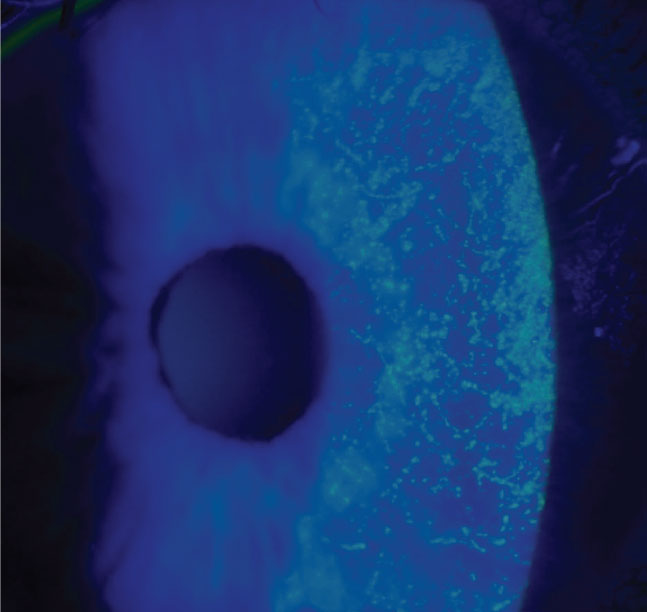
Pervasive use of digital screens, and the reduced blink rates they induce, was often noted as a cause for recent growth in DED. Image courtesy of Katherine Sanford, OD. Click image to enlarge. |
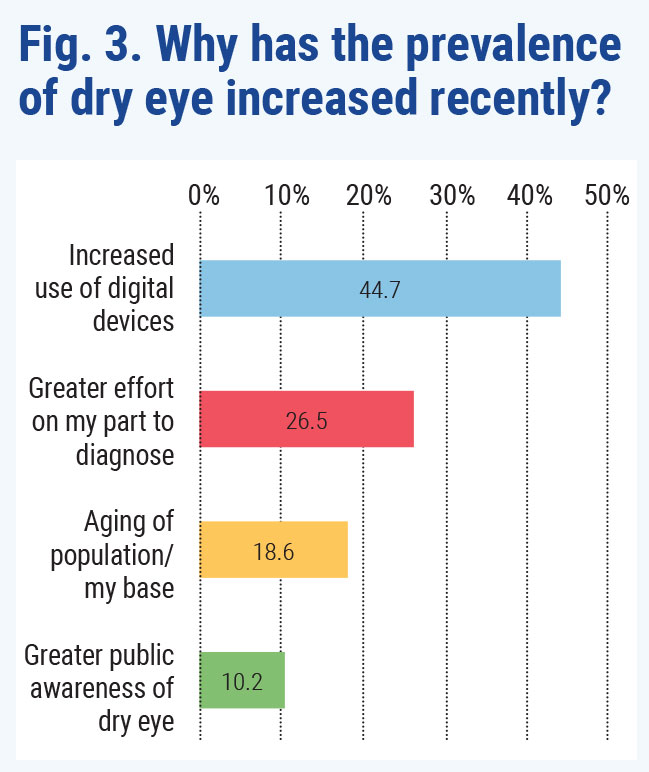
Still, our survey respondents say they’re on the case: 85% said they’ve been seeing and addressing dry eye more in the last five to 10 years. Digital screen use tops the list of reasons for the increase, followed by greater effort on the OD’s part, aging of the population and greater public awareness of dry eye (Figure 3).
A Growing Trend
Echoing the survey’s findings on DED prevalence, Katherine Sanford, OD, of the VA Medical Center in Memphis, estimates almost 45% of patients seen at her clinic last year were diagnosed with dry eye or meibomian gland dysfunction (MGD). She attributes this in part to patients spending more time on computers, which has been heightened with COVID-19.
Mask wear is also adding to the proliferation of DED, says Mile Brujic, OD, of Bowling Green, OH. “We were already trending upward in dry eye cases, but COVID has taken it to the next level.”
Additionally, clinicians now have a greater understanding of dry eye and its various etiologies and treatments, Dr. Sanford suggests.
“I’ve become more proactive about probing for symptoms during case history as well as screening for anterior segment signs of dry eye, even in the absence of complaints,” Dr. Sanford explains. “The addition of diagnostic equipment to our clinic also expanded my ability to more objectively identify tear film and meibomian dysfunction in our patients.”
 |
| Click image to enlarge. |
The increase in DED cases may also be due to perception. Individuals with dry eye are typically seen more often—between two to six times a year—so doctors may think they have an influx of new dry eye patients when they are simply experiencing more encounters, says Dr. Brujic.
When to Discuss DED
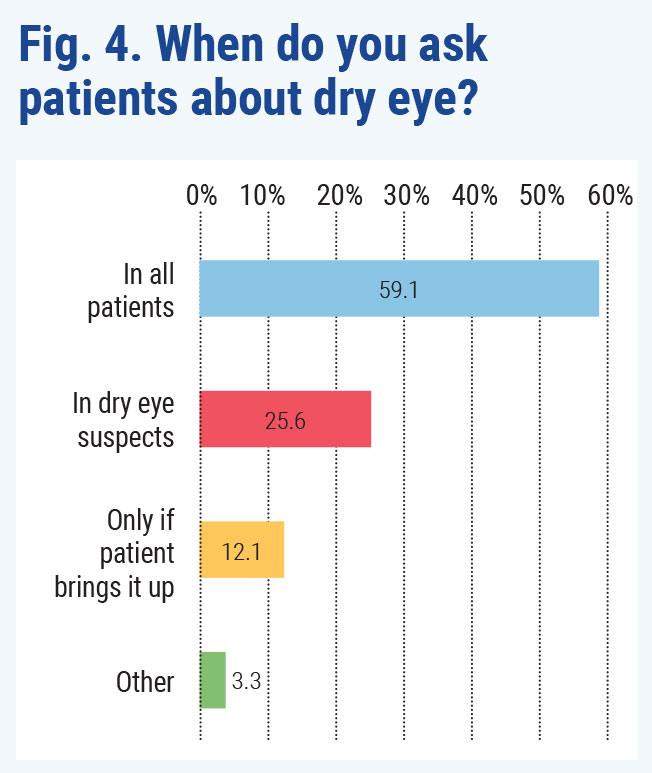
Even though the majority of respondents said a significant portion of their patients have DED or are symptomatic, just 59% discuss dry eye symptoms with every patient (Figure 4). About 26% of responders said they discuss dry eye in suspected cases, and approximately 12% talk about it only if a patient brings it up.
Candice Tolud, OD, of Moorestown, NJ, believes most patients experience some form of dry eye but may dismiss it as a symptom of something else, such as an allergy. The Tear Film and Ocular Surface Society’s DEWS II study recommends observation for patients without symptoms, so if Dr. Tolud recognizes signs of DED in a patient who is asymptomatic, she makes them aware of her findings and recommends an OTC artificial tear should symptoms arise before their next visit. In patients who are experiencing symptoms, she immediately addresses this and recommends follow-up for a dry eye evaluation to determine what treatment options would work best.
|
| Click image to enlarge. |
With this approach, Dr. Tolud brings up dry eye at multiple points during the exam, when applicable: during the history if complaints are suggestive of dry eye, during refraction if the individual has fluctuating vision or inconsistent responses and again during the slit lamp exam if she sees signs of tear film instability or corneal/conjunctival staining. She then brings the points together during her final assessment and plan for treatment.
“By linking dry eye to various patient complaints and findings throughout the exam, it helps to enforce the point of dry eye as an underlying cause of patient complaints, and makes the patient more comfortable with the diagnosis and cooperative with the treatment plan,” she says.
Testing Trends
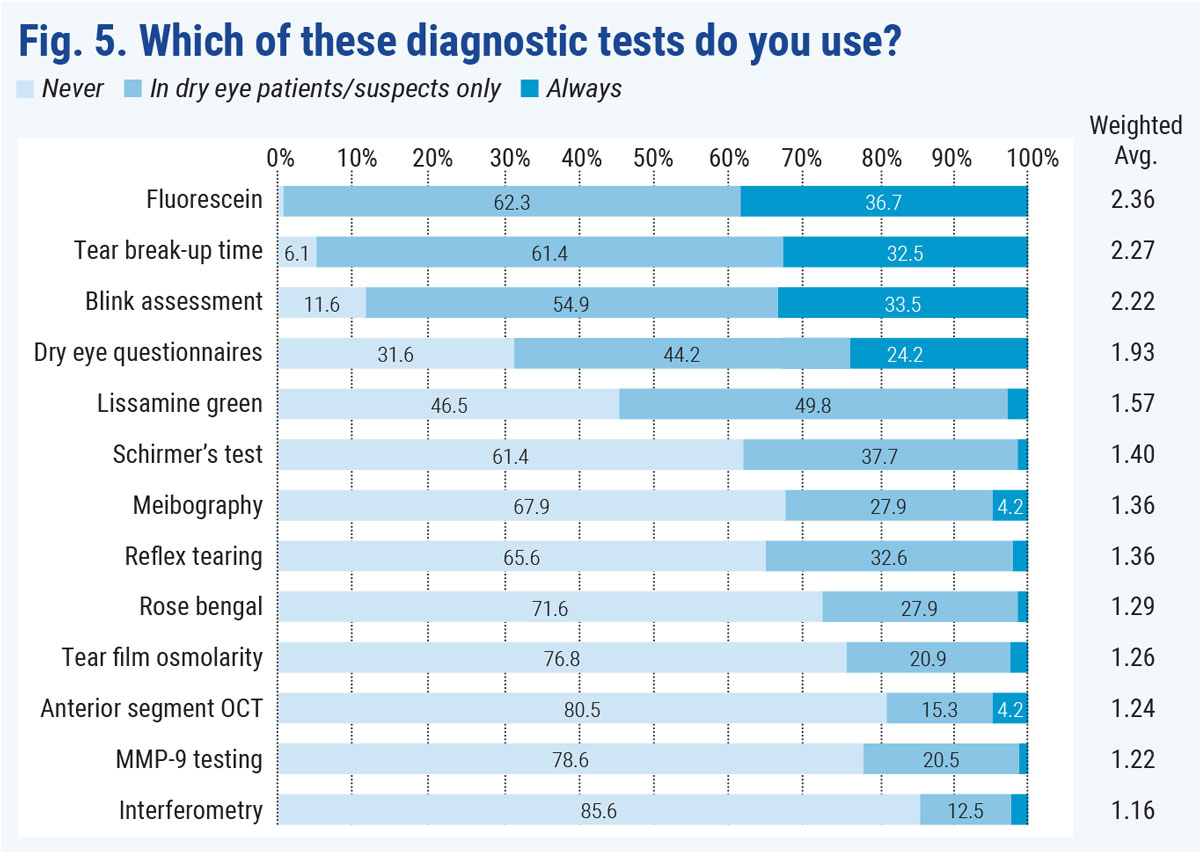
There’s no shortage of ways to assess prospective dry eye patients, with options ranging from simple slit lamp assessment to sophisticated diagnostic technology. Among our respondents, the most popular choices were cost-effective and simple ones. The #1 testing method in the survey was fluorescein staining, with about 37% saying this was always their first choice in their dry eye diagnostic toolbox (Figure 5). Approximately 62% of ODs said they administer fluorescein only in dry eye suspects or in previously diagnosed DED patients.
 |
| Click image to enlarge. |
Ranking second in popularity was tear break-up time (TBUT). Roughly 33% of optometrists responded they always use TBUT, and 61% cited they administer it only in dry eye or suspect patients.
Coming in third in popularity was blink assessment, with about 34% of responders always using this testing method, and 55% commenting they turn to TBUT only in DED patients and suspects.
Though high-tech tools are often lauded for their accuracy, none cracked the top five in our survey. Meibography ranked #7 in popularity and tear osmolarity came in at #10. Other tests doctors said they use less frequently include anterior segment OCT, MMP-9 and interferometry.
 |
| Click image to enlarge. |
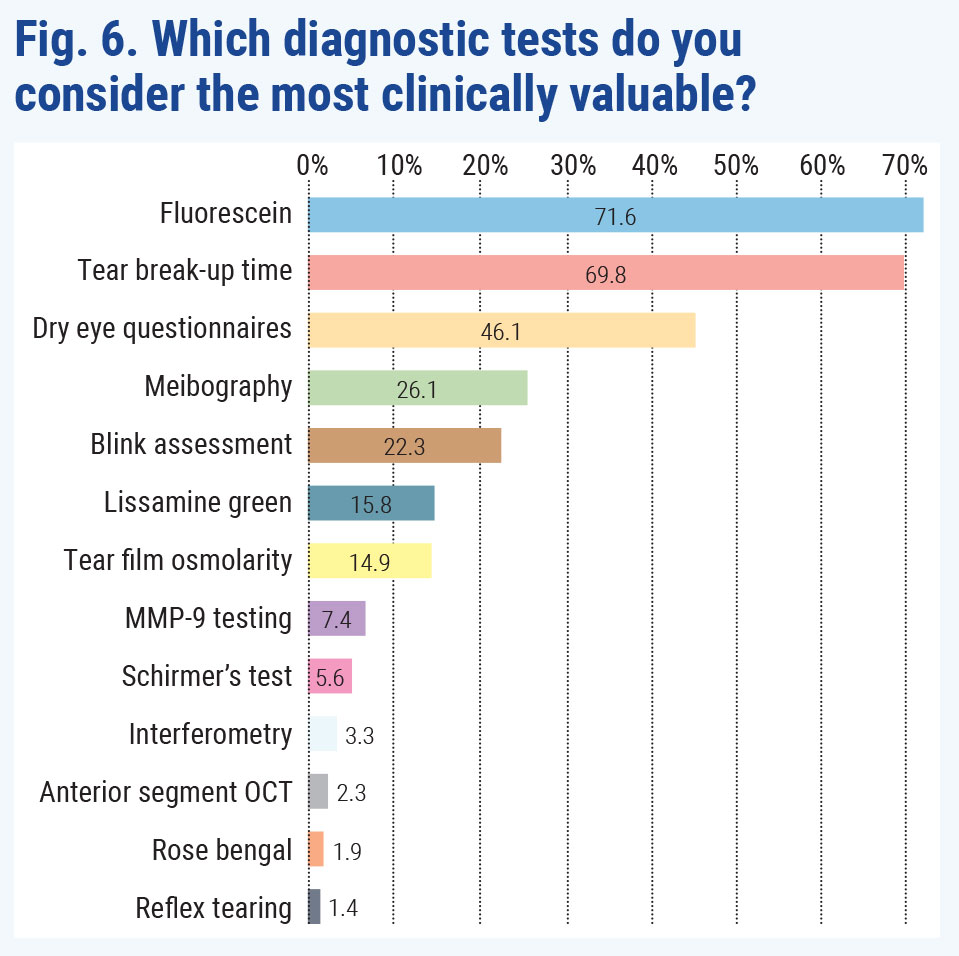
When asked which tests provide the greatest clinical value, respondents again favored low-tech options. The majority of doctors ranked fluorescein staining as #1, followed by TBUT and dry eye questionnaires (Figure 6). Interestingly, meibography and osmolarity both did better in this ranking, coming in fourth and seventh, respectively, suggesting pent-up demand for these tools among ODs if only they could make the numbers work. By contrast, although blink assessment ranked third among the most popular tests optometrists said they use, this method came in fifth in the survey as having the greatest clinical value.
Even though doctors have their preferred diagnostic approach, it’s not enough to assess just one aspect of dry eye, Dr. Mickles cautions. Instead, it should be a multi-pronged approach and include methods of assessing tear quantity, tear quality, ocular surface integrity and meibomian gland function. Advanced technology, such as meibography, is especially advantageous in a specialty practice.
 |
|
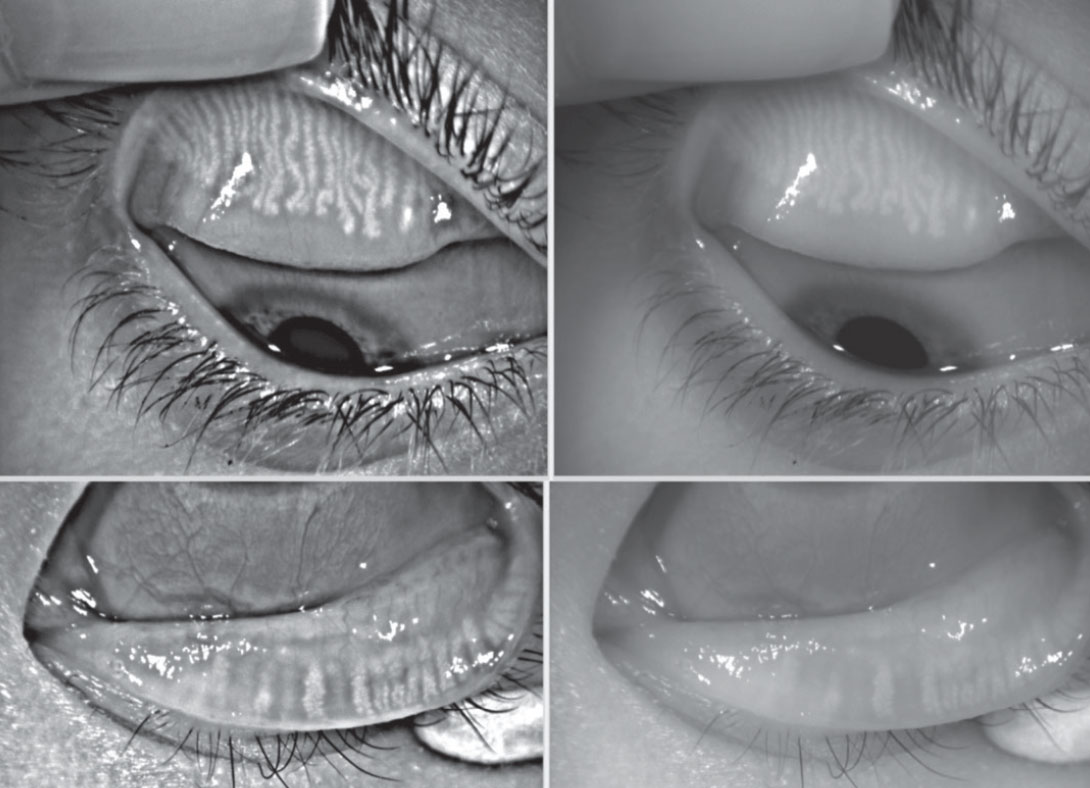
Meibography is high on the list of diagnostic procedures ODs would like to add to their practices—ranking fourth overall in clinical value and first among newer devices—but cost concerns limit adoption. Image courtesy of Dan Fuller, OD. Click image to enlarge. |
As part of every exam Dr. Brujic performs, each patient undergoes lid margin assessment at high magnification, meibomian gland assessment with eyelid transillumination and fluorescein staining of the ocular surface. Once a dry eye suspect is identified, individuals will also receive meibography with infrared imaging and InflammaDry (Quidel) to assess inflammation levels.
 |
| Click image to enlarge. |
Dr. Tolud uses fluorescein, TBUT, blink assessment and dry eye questionnaires at the initial exam. During a patient’s dry eye follow-up visit, she does further testing, including tear osmolarity, MMP-9, meibography, Schirmer’s and lissamine or rose bengal staining. “I find these diagnostic tests are great ways to monitor patient progress, and it’s a wonderful educational tool as well to show patients over time how their tear quality has improved during the course of their treatment.”
Questionnaire OptionsIf you’re looking to incorporate a dry eye questionnaire in your practice, here are some of the most popular. Ocular Surface Disease Index Standard Patient Evaluation of Eye Dryness Five-item Dry Eye Questionnaire Dry Eye-Related Quality-of-Life Score |
Questions About Questionnaires
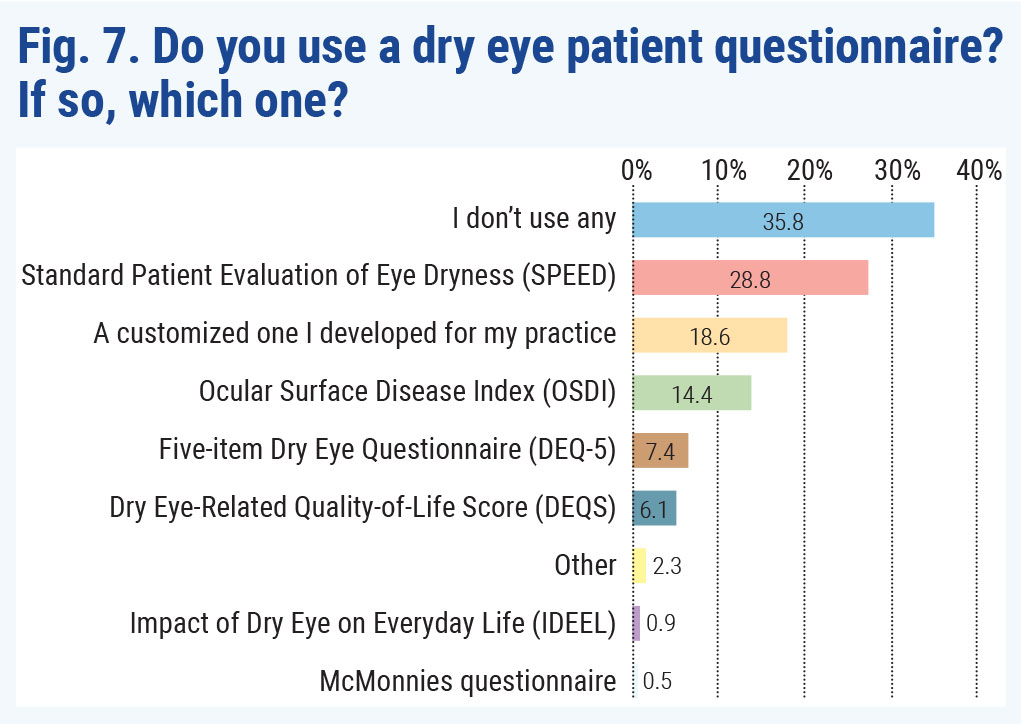
Even though dry eye questionnaires ranked as one of the top three tests doctors found to be the most clinically relevant, about 36% of responders said they don’t use one at their practice (Figure 7).
For those ODs who include this screening tool in their testing protocol, the most popular option was the Standard Patient Evaluation of Eye Dryness (SPEED) questionnaire designed by Don Korb, OD, and Caroline Blackie, OD. Next most popular was a homegrown option—the practice’s own custom questionnaire.
The third most popular questionnaire was the Ocular Surface Disease Index (OSDI), followed by the Five-item Dry Eye Questionnaire (DEQ-5) and the Dry Eye-Related Quality-of-Life Score (DEQS).
While there are several questionnaires available to clinicians, DEWS II recommends either the OSDI due to its strong establishment in the field or the DEQ-5 due to its short length and discriminative ability.2
Dry eye questionnaires are very beneficial in monitoring therapeutic response and quantitatively documenting improvement, Dr. Sanford says. Although her clinic offers several questionnaires, she prefers the OSDI. “It screens for key symptoms associated with dry eye and their impact on vision-related function.” Dr. Sanford administers the questionnaire at the initial workup to determine the severity of the patient’s dry eye, and repeats it following the start of treatment to quantify improvement.
In-Office Procedures
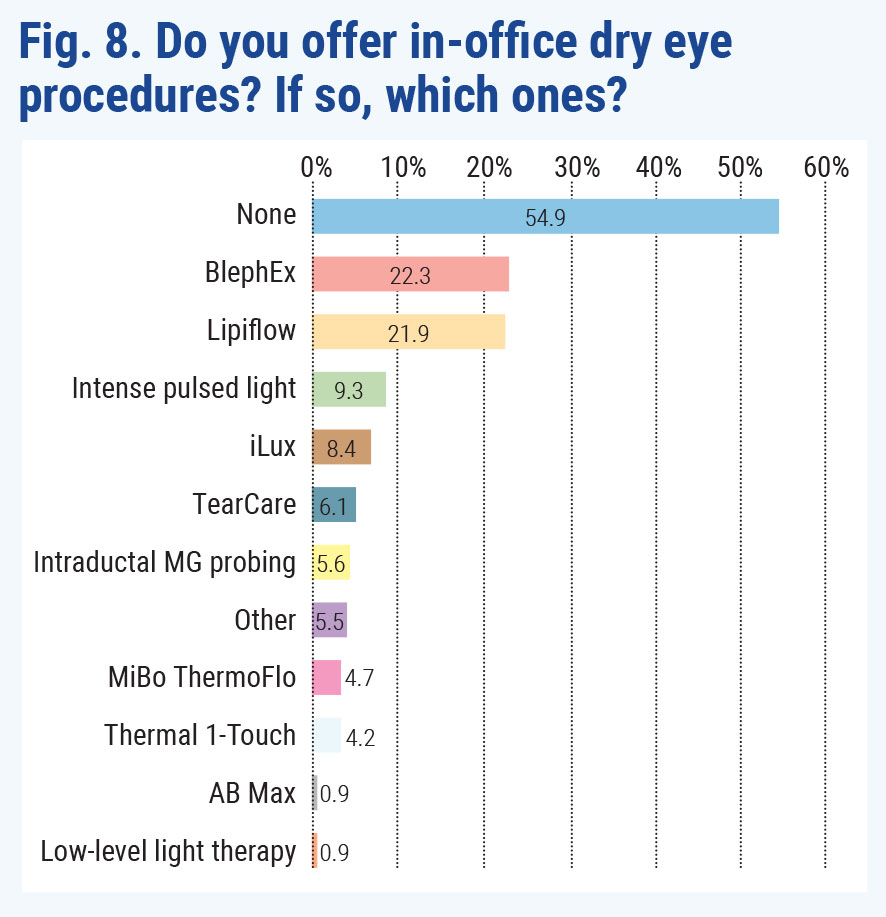
While new technologies have recently entered the market to manage dry eye and MGD, over half of the doctors who responded to the survey indicated they don’t offer in-house treatments (Figure 8).
For respondents who do provide in-house services, the top technologies were BlephEx (22.3%) and Johnson & Johnson’s Lipiflow (21.9%).
 |
| Click image to enlarge. |
Dr. Tolud offers Lipiflow, which uses thermal pulsation to heat the meibomian glands to liquefy the meibum and massages the glands at different intensities to expel blockages and stagnant material from the glands. One treatment lasts for 12 minutes, and both eyes are done simultaneously. Effects can be seen for over a year in many patients, she says. “I’ve had great success with this device in my practice and adjunct therapy, along with topical treatment and warm compresses, for patients where MGD is a contributing factor in their dry eye disease.”
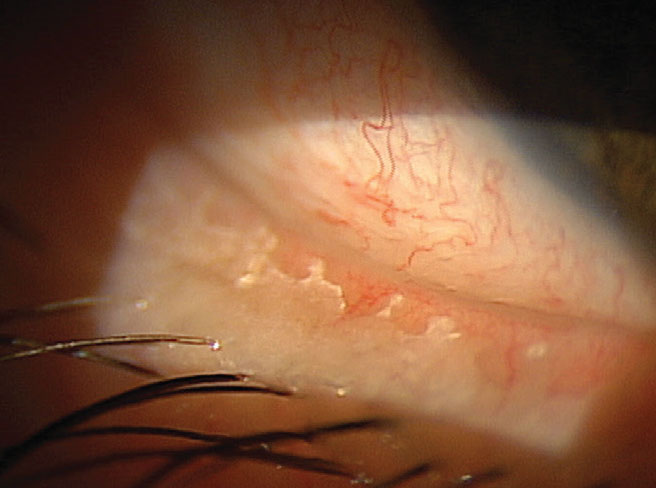
BlephEx involves a rotating sponge the practitioner uses to clean and exfoliate the eyelid margins to remove bacterial biofilm and debris that can clog meibomian gland orifices. The process takes approximately seven minutes and is performed on each individual eyelid. Results are optimal if the procedure is repeated every four to six months.
 |
| Click image to enlarge. |
In addition to Lipiflow and BlephEx, Dr. Mickles also uses MiBo ThermoFlo, which provides pressure and heat; unlike Lipiflow, the technology is more user-dependent, as the doctor massages the eyelids during the procedure. Although there is not as much research evidence supporting MiBo ThermoFlo, it can be a more cost-effective approach, she says.
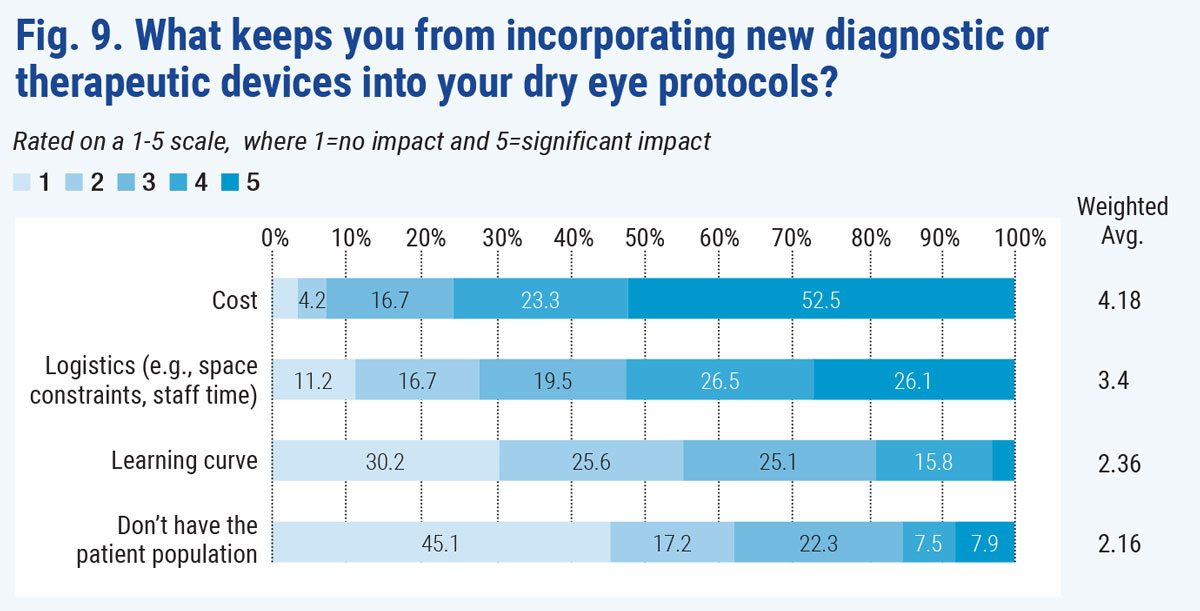
Despite the purported benefits of the new technologies for diagnosis and treatment, sticker shock keeps most optometrists from adding them to their practices. For the majority of doctors surveyed, cost was the most significant prohibitive factor for not incorporating new in-house technologies, with 52.5% calling out price as a significant deterrent (Figure 9). Logistics, learning curve and patient need all ranked lower than financial factors.
 |
|
Bacterial biofilm on the lid margin contributes to MGD and, hence, dry eye. BlephEx treatment—the top choice for office procedures in our survey—removes it. Image courtesy of Paul Karpecki, OD. Click image to enlarge. |
Trouble with Treatments
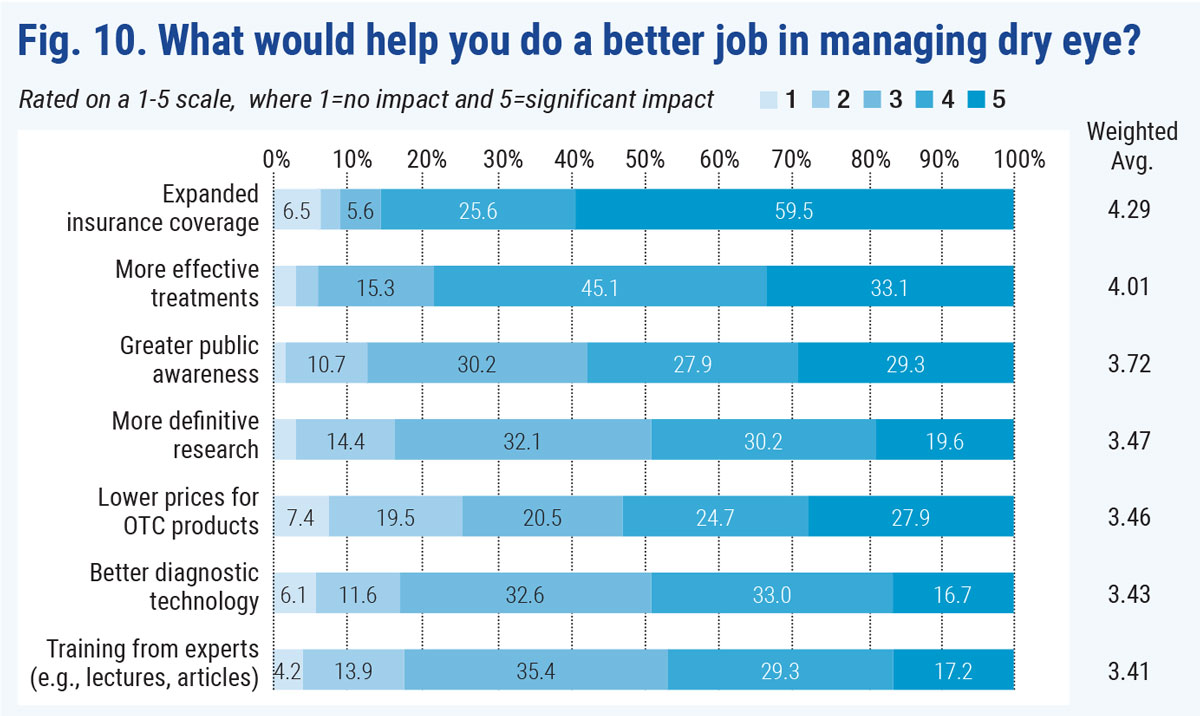
Even though several new dry eye treatments have become available over the past decade, some doctors felt the field of options was still limited. In fact, over 33% of responders said more effective treatments would significantly help them do a better job in managing dry eye and another 45% ranked it 4 out of 5 in importance (Figure 10). “We need new approaches to treatment,” one optometrist commented. “Yes, I am so happy we have more treatments available, but we need more in our arsenal.”
But the biggest deterrent to success is clear: insurance hassles. Nearly 60% of respondents said expanded insurance coverage was the most significant factor that would help them do a better job with dry eye, and another 26% rated this 4 out of 5 in impact.
Despite these setbacks, optometrists are fortunate that this once unappreciated condition is garnering more attention by pharmaceutical companies and device manufacturers, Dr. Mickles says. “While we do face some challenges with current therapies, they are effective when prescribed properly. Enacting customized treatment plans that target the primary cause of patients’ DED, along with thorough education, has provided more-than-sufficient dry eye relief for many of my patients.”
 |
| Click image to enlarge. |
Dr. Mickles believes the current dry eye treatments are effective, but doctors need to be proactive in educating patients on how to mitigate potential drug side effects and setting realistic expectations on the timing of symptom relief. Additionally, it is imperative to tell patients that DED is a chronic condition, similar to other diseases such as diabetes, that requires regular monitoring and maintenance.
Top Treatments, Ranked
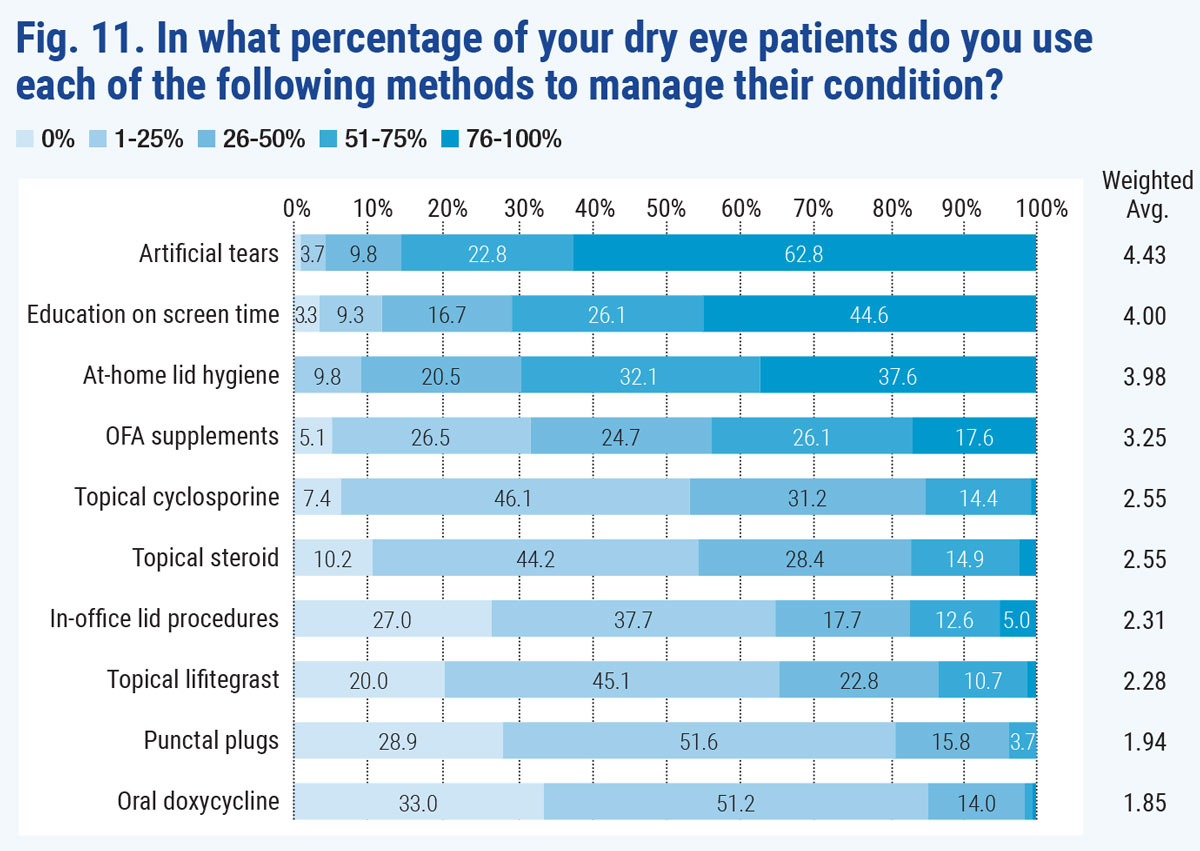
Considering the current options, most survey participants ranked artificial tears as their most popular treatment choice (Figure 11, below).
Despite their popularity, Dr. Brujic refers to artificial tears as the “Tylenol of dry eye management,” since this option makes the patient feel better temporarily but does nothing to improve the ocular physiology. Artificial tears can be recommended as supplemental therapy but not a first-line approach, he suggests. Also, most patients have already tried artificial tears by the time they reach his office, so these individuals usually need another treatment option, such as environmental modifications along with lid debridement and cleaning, meibomian gland warming and evacuation or a topical anti-inflammatory, Dr. Brujic explains.
 |
| Click image to enlarge. |
Following artificial tears as the most popular treatment, survey responders ranked education on blink rates/screen time second followed by instruction on lid hygiene. Landing at #4 four in popularity was omega-3 supplements, despite reported controversy over fish oil’s effectiveness in treating DED, as the DREAM study reported omega-3 fatty acids offered no benefit over an olive oil placebo.3
Topical cyclosporines and steroids lagged behind the previously mentioned treatments, which could be in part due to some ODs’ concerns about reimbursement from insurance companies, a common gripe noted in our survey and elsewhere.
Paying Your DEWSThe Tear Film and Ocular Surface Society’s 2017 DEWS II report, which encapsulated a decade’s worth of new research, was the impetus for 62% of respondents to change their approach to DED, they told us. The remaining 38% said the report didn’t impact what they do. Those favorable to DEWS II said it caused them to treat dry eye earlier in the disease course and assess all patients, even children. Detractors often said the report was too complex. For fans and holdouts alike, here’s a nuts and bolts summary of DEWS II: New definition: The definition of DED expands on dry eye as a disease with multiple etiologies, but with the common aspect of a loss of tear film homeostasis due to tear instability, hyperosmolarity, ocular surface inflammation and damage, or a combination of all three. Prioritizing symptoms: DEWS II offers a step-by-step decision-making process focused on the presence or absence of symptoms and whether symptoms correspond with signs. Overlap of evaporative and aqueous-deficient DED: Previously, the common consensus was that these two types of dry eye were distinct from one another. DEWS II did away with this philosophy by stating that evaporative and aqueous-deficient dry eye often coincide. Rethought tear film dynamics: DEWS II replaced the initial three-layer tear film concept with a two-phase model with the lipid layer overlying a mucoaqueous phase, and the entire tear film involved in limiting evaporation. DED’s vicious circle: DEWS II states that the etiology of DED isn’t linear, but rather a self-perpetuating circle. For example, tear hyperosmolarity is shown to be the hallmark of DED, working as both a catalyst and consequence of various steps along the circular process. The report affirms there are many entrances into that circle, all of which can result in DED. Iatrogenic causes: DEWS II raises awareness of DED caused by ophthalmic surgery and medication use. Also noted: the concentration of preservatives in glaucoma medications, specifically benzalkonium chloride, has the potential to cause inflammation and proptosis. A new approach to diagnosis: DEWS II suggests using triaging questions to help differentiate DED from other ocular surface issues prior to your traditional work-up. Individualized treatment: Although DEWS II offers many management and treatment recommendations, it advises practitioners to tailor their approach based on individual patients. In other words, there’s no one-size-fits-all way to manage and treat DED. |
A Dry Eye in the House
Dry eye is a large and growing problem faced by many, a doctor who responded to the survey said. “This is a great opportunity for optometry to get into the minds of our patients and change the culture of obtaining routine eye care.”
1. Farrand KF, Fridman M, Stillman IO, Schaumberg DA. Prevalence of diagnosed dry eye disease in the United States among adults aged 18 years and older. Am J Ophthalmol. 2017;182:90-8. 2. Wolffsohn JS, Arita R, Chalmers R, et al. TFOS DEWS II Diagnostic Methodology report. Ocul Surf. 2017;15(3):545-8. 3. Asbell PA, Maguire MG, Pistilli M. n-3 fatty acid supplementation for the treatment of dry eye disease. N Engl J Med. 2018;378(18):1681-90. |

