 |
A 59-year-old African-American male presented with blurry vision and a central spot in his right eye for the past four years. He reported seeing floaters that began two years prior; his past ocular history was also significant for a motor vehicle accident that occurred four years earlier. In the accident, he was hit on the right side of his body and reported having sudden vision loss in the right eye.
His medical history was significant for a stroke involving the left hemisphere, also four years prior, as well as Type 2 diabetes, which was diagnosed nine years ago and is being treated with metformin and insulin injections.
Upon exam, best-corrected visual acuity was 20/200 OD and 20/20 OS. Confrontation visual fields were full-to-careful finger counting OU. Pupils were equal, round and reactive, but there was an afferent pupillary defect in the right eye. The anterior segment exam was unremarkable except for mild cataracts OU, and there were no cells or flare in either eye.
On dilated fundus exam of the right eye, a posterior vitreous detachment was present. There was a large fibrotic scar with areas of pigment surrounding in the macula (Figure 1). Upon careful examination, a suspicious orange area was noted temporal to that lesion (see yellow arrow in Figure 1). An OCT was performed and is available for review (see red arrow in Figure 2). The retinal exam of the left eye was completely normal.
 |
| Fig. 1. Fundus photo of the right eye. What might that central fibrotic lesion represent? Click image to enlarge. |
Take the Retina Quiz
1. Which element of the patient’s history could have caused this retinal finding?
a. Type 2 diabetes.
b. Stroke of the left hemisphere.
c. Car accident injury to the right side of his body.
d. Onset of floaters two years prior.
2. What does the orange lesion adjacent to the fibortic area represent?
a. A retinal detachment.
b. A subretinal hemorrhage.
c. A drusenoid PED.
d. A PED secondary to choroidal neovascularization (CNV).
3. What is the correct diagnosis for this fundus presentation?
a. Chorioretinal scar from toxoplasmosis.
b. CHRPE.
c. Choroidal rupture with secondary CNV.
d. Proliferative diabetic retinopathy.
4. Which of the following is not a treatment option for this condition?
a. Observation.
b. Injection of anti-VEGF agent.
c. Azithromycin PO.
d. Combination of A and B.
5. Which imaging technique would be helpful in order to get a definitive diagnosis?
a. B-scan ultrasound.
b. Fluorescein angiography/ OCT angiography.
c. Electroretinogram.
d. All of the above.
For answers, see below.
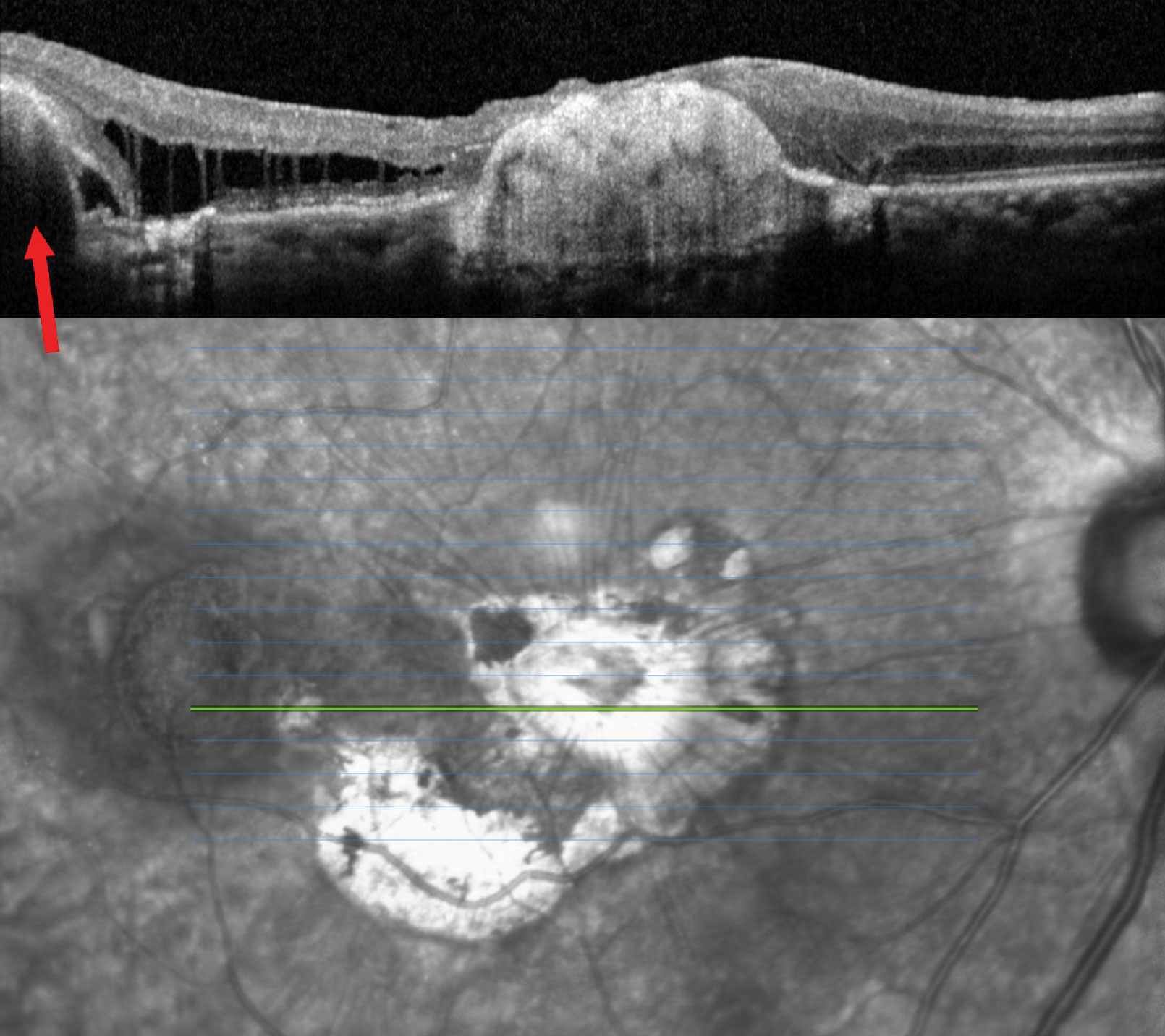 |
| Fig. 2. OCT of the right eye. What could the area of RPE elevation possibly correspond to? Click image to enlarge. |
Discussion
There is an obvious chorioretinal scar involving the macula of right eye in our patient. In the absence of history, there are a lot of possible etiologies, including an old toxoplasmosis scar which might be the immediate conclusion given the location and characteristic appearance. However, the history offers a critical clue to the actual etiology. Our patient describes having an motor vehicle accident four years prior that resulted in a sudden loss of his central vision. So, how does the clinical presentation fit into our patient having a traumatic event?
Ocular trauma can present in myriad ways depending on the type and location of the injury. Blunt force trauma can cause a contrecoup injury in which direct displacement and deformation of the globe can occur. In commotio retina, the hydraulic forces on the eye as a result of the injury can cause disruption and swelling of the photoreceptors, which can even lead to death of these cells.1 The shock waves from the trauma coursing through the eye can result in hemorrhagic or non-hemorrhagic posterior vitreous detachments, retinal breaks and even retinal detachment, as well as traumatic optic neuropathy and choroidal rupture, to name a few.
A choroidal rupture happens when there is disruption of the choriocapillaris, Bruch’s membrane and the retinal pigment epithelium (RPE) from the direct result of the trauma or indirectly from the shock waves that are transferred through the vitreous and/or eye walls of the globe as a result of the trauma. When this occurs, stretching and folding of these structures leads to a break in Bruch’s membrane and the RPE.
Choroidal ruptures are typically located in the posterior pole and most often concentric to the optic disc.2 Sports injuries and car accidents involving the deployment of airbags are common causes, although systemic conditions such as pseudoxanthoma elasticum, Ehlers-Danlos syndrome, Paget’s disease, sickle cell anemia or virtually any condition involving angioid streaks may predispose a patient to choroidal ruptures during an impact of even minimal intensity, as these represent breaks in Bruch’s membrane as well.
In the acute phase, these breaks are commonly associated with subretinal and sub-RPE hemorrhages and may also be associated with other traumatic findings. In the chronic phase, CNV may develop and can be found at the edges of the rupture.2 CNV may occur months to years after the traumatic event and can result in fibrotic scarring.3
The prognosis for choroidal rupture is highly dependent on location and whether it involves the foveal area, and also if subretinal or sub-RPE hemorrhages are present. Patients with choroidal rupture should be followed carefully for potential secondary CNV post-trauma, which may further decrease visual acuity.3
The treatment of choroidal rupture often involves observation and close follow-up to monitor for spontaneous improvement of vision, as there is no medical or surgical therapy indicated to treat acute episodes. Patients are often provided with an Amsler grid as a way to self-monitor for any changes in vision, as they carry the risk of developing CNV in the future. In cases where it develops, intraocular injections of anti-VEGF can improve visual outcomes.
Concluding Thoughts
No doubt the vision loss that our patient suffered is from his motor vehicle accident. The large chorioretinal scar involving the macula is due to a large choroidal rupture. Unfortunately, the rupture involves his macula, which explains the sudden loss of vision.
Regrettably, that’s not the end of it. The OCT and clinical finding temporal to the macula are quite revealing. The orange area that was noted with the arrow is elevated and confirmed on the OCT scan where we can see an RPE detachment. There is also intra- and subretinal fluid adjacent to the RPE detachment, all consistent with an active CNV.
Our patient was referred to a retina specialist for possible treatment; ultimately, the MD decided to monitor him without treatment because of his poor visual prognosis.
Retina Quiz Answers
1) c; 2) d; 3) c; 4) c; 5) b.
Dr. Dunbar is the director of optometric services and optometry residency supervisor at the Bascom Palmer Eye Institute at the University of Miami. He is a founding member of the Optometric Glaucoma Society and the Optometric Retina Society. Dr. Dunbar is a consultant for Carl Zeiss Meditec, Allergan, Regeneron and Genentech.
Dr. Fitoussi is an optometrist at the Bascom Palmer Eye Institute at the University of Miami. He earned his bachelor’s of science degree in optometry at Bar-ilan University in Tel Aviv in 2014 and his doctorate of optometry at Nova Southeastern University in 2020.
| 1. Wood CM, Richardson, J. Indirect choroidal ruptures: aetiological factors, patterns of ocular damage, and final visual outcome. Br J Ophthalmol. 1990;74(4): 208-11. 2. Bailey Freund K, Sarraf D, Mieler WF, et al. Choroidal rupture. the retinal atlas, 2nd Edition. 2017; 1011. 3. Fineman MS, Ho AC. Choroidal rupture. Color Atlas & Synopsis of Clinical Ophthalmology, 2nd Edition. 2012; 316. |

