 |
A 68-year-old African American female presented for an initial comprehensive ocular examination with a chief complaint of intermittent burning of both eyes over the past two years. The patient denied any additional ocular history and reported a medical history of hypertension for which she was properly medicated with lisinopril/hydrochlorothiazide, an angiotensin-converting enzyme (ACE) inhibitor. She denied having allergies of any kind.
Diagnostic Data
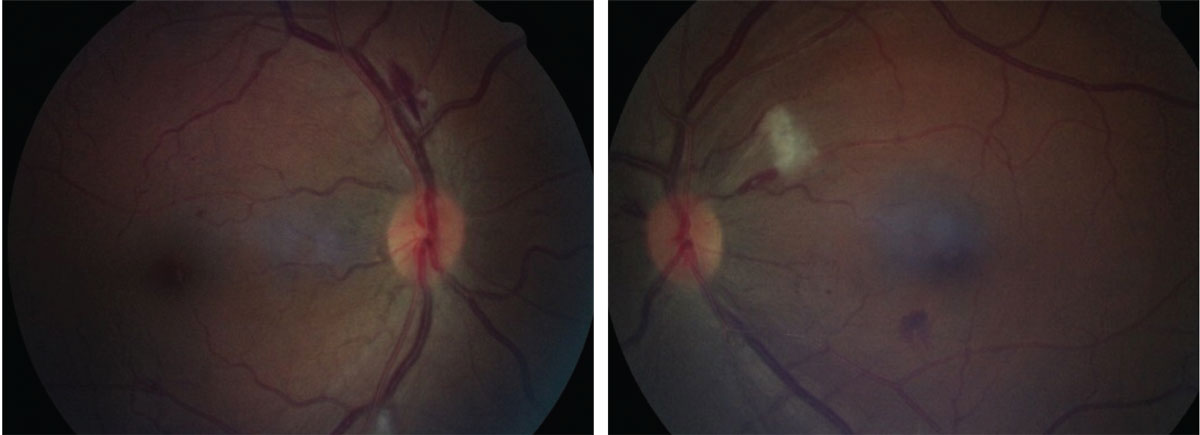
Her best-corrected entering visual acuity was 20/20 OU. Her external examination was unremarkable with no evidence of afferent pupillary defect. Biomicroscopic evaluation of the anterior segment was normal. Goldmann applanation tonometry measured 17mm Hg OU. The pertinent bilateral retinal findings are demonstrated in the photographs.
Additional testing included a lab workup for diseases capable of producing cotton wool spots, intraretinal flame-shaped hemorrhages and Roth spots, including coagulopathy, hyperviscosity, diabetes, hypertension, dyslipidemia, cardiopathy and carotid artery disease. The tests included a complete blood count with differential and platelets (CBC), an erythrocyte sedimentation rate (ESR), liver function studies (LFT), C-reactive protein (CRP), fibrinogen, fasting blood glucose, lipid panel, electrocardiogram (ECG) and carotid duplex.
 |
|
Dilated exam revealed the presentations shown here. How might they relate to the case history she described? Click image to enlarge. |
Discussion
The diagnosis in this case is retinopathy associated with multiple myelogenous leukemia. When leukemia cells infiltrate the retina, they have the potential to cause leukemic retinopathy characterized by intra-retinal hemorrhages, Roth spots (white centered intraretinal hemorrhages), vitreous hemorrhage, dilated and tortuous retinal veins and cotton-wool spots.1-9 These changes can also occur in the choroid; however, they are less common.3
Acute promyelocytic leukemia (APL) is the type of leukemia with a myeloid population (cells relating to bone marrow or spinal cord) dominated by the promyelocytes, a granulocyte precursor that develops from the myeloblast. These are bone marrow cells that give rise to the granulocytes found in blood.4
There are two types of promyelocytic leukemia classifications: (1) the French-American-British approach, composed of the morphological and cytochemical aspects of the cells, which notes that APL is acute myeloid leukemia subtype M3 and (2) the World Health Organization classification system, which describes it as APL with translocation between chromosomes 15 and 17.4
In both classifications, clinically the disease is considered a disseminated intravascular hematological coagulation characterized by the activation of circulating thrombin and plasmin, which can cause thrombosis and hemorrhage in small and midsize vessels, resulting in eventual multiple organ failure.4
These patients are generally young, with a sudden-onset hemorrhagic syndrome that is characterized by mucosal cutaneous hemorrhage and thrombotic manifestations.4
Clinically, deep thrombophlebitis, pulmonary embolism, cerebral thrombosis and renal thrombosis can occur.4 In this instance, hypercoagulability is induced by the tissue factors of the leukemic M3 cells.4 These bind in the presence of calcium and activate the X factor (extrinsic clotting pathway), inducing thrombin and then fibrin production.4
The diagnostic timeframe from the discovery of the ocular findings to systemic management is considered urgent.4 The leukocyte count prior to the onset of therapy is the most prognostic factor for survival (high risk WBC >10.000/µl).4,5 Age is another important factor, with individuals of younger age having a better profile.4 Prognosis after treatment is favorable, with very high rates of complete remission—as high as 90% of cases.4,5 In one study evaluating the extent of retinopathy, investigators concluded those cases that presented with multiple intraretinal hemorrhages, Roth spots, cotton-wool spots and macular hemorrhages had a poorer prognosis.4,6
Leukemic retinopathy is typically bilateral but may occur with asymmetry or even present unilaterally.9 The condition is characterized by general venous congestion, areas of retinal edema and Roth spots.3,5,7,8 The retinal vessels become dilated, tortuous and sheathed, due to the leukocytic infiltration of the vessel walls.8 This may also produce a granular appearance of a blood column.8 The Roth spots are formed by accumulations of white blood cells and fibrous exudation.3,5,7,8
Systemically, leukemia alters the integrity of blood vessels.1-10 In the retinal and choroidal vasculature, it can lead to neovascularization, hemorrhage and neoplastic infiltrates in potentially all ocular structures.1-10 Bilateral leukemic hypopyon is considered an early sign of central nervous system involvement or systemic relapse.10 Chronic myeloid leukemia (CML) is an indolent neoplasia often characterized by a 9/22 chromosomal translocation.9 Patients with CML or any kind of leukemia often present with fatigue, unwanted weight loss and hepatosplenomegaly, with isolated ocular findings only occurring in a minority of patients.9
Treatment of acute promyelocyte leukemia requires a sustained therapy as well as a therapeutic response to a non-cytostatic agent: isotretinoin. A dose of 45mg/m2/day PO can induce full remission in most patients with LAM3 possessing translocation t(15;17).4 When remission is not long-lasting, classical chemotherapy should be considered.4
This patient was referred to their general internal medicine practitioner for an extensive laboratory workup to rule out coagulopathy, hyperviscosity, diabetes, hypertension, dyslipidemia, cardiac and carotid etiologies. Suggested bloodwork included a complete blood count with differential and platelets, complete metabolic panel, fasting blood glucose and glycosylated hemoglobin, blood pressure, lipid panel, erythrocyte sedimentation rate, C-reactive protein testing, fibrinogen, electrocardiogram) and a Doppler ultrasound of the carotid arteries. The testing uncovered multiple myelogenous leukemia, for which the patient is now treated and doing well. The intraretinal hemorrhages resorbed months after appropriate management was initiated and have not recurred.
Dr. Gurwood thanks Chris Brennan, OD, for his contributions to this case.
Dr. Gurwood is a professor of clinical sciences at The Eye Institute of the Pennsylvania College of Optometry at Salus University. He is a co-chief of Primary Care Suite 3. He is attending medical staff in the department of ophthalmology at Albert Einstein Medical Center, Philadelphia. He has no financial interests to disclose.
1. Vadlamudi S, Annapareddy SN. Multiple myeloma: Diagnosis and management issues in patients with pre-existing chronic kidney disease. Saudi J Kidney Dis Transpl. 2016 ;27(1):9-14. Katagiri D, Noiri E, Hinoshita F. Multiple myeloma and kidney disease. Scientific World Journal. 2013;27(10);2013:487285. 2. Takita A, Hashimoto Y, Saito W, Kase S, Ishida S. Changes in blood flow velocity and thickness of the choroid in a patient with leukemic retinopathy. Am J Ophthalmol Case Rep. 2018;12:68-72. 3. Scripcă OR, Pădurariu C, Boricean NG, Botoș L. Leukemic retinophaty, the first manifestation in a case of acute myelogenous leukemia. Rom J Ophthalmol. 2018;62(1):72-77. 4. Testa U, Lo-Coco F. Prognostic factors in acute promyelocytic leukemia: strategies to define high-risk patients. Ann Hematol. 2016;95(5):673–680. 5. Reddy SC, Quah SH, Low HC, Jackson N. Prognostic significance of retinopathy at presentation in adult acute leukemia. Ann Hematol. 1998;76(1):15-8. 6. Ilo OT, Adenekan AO, Alabi AS, Onakoya AO, Aribaba OT, Kehinde MO, Salako O. Ocular manifestations of leukaemia: A teaching hospital experience. Niger Postgrad Med J. 2019;26(4):205-210. 7. Lyu S, Zhang M, Gao Y. Acute bilateral retina hemorrhages beneath internal limiting membrane: An unusual ophthalmological case report of acute leukemia during complete clinical remission. Medicine (Baltimore). 2018;97(7):e0000. 8. Seraly MP, Gupta SK, Mehmi I, Veltri L, Ghorayeb GR. A unique case of chronic myeloid leukemia presenting as monocular vision loss with unilateral retinopathy. Am J Ophthalmol Case Rep. 2019;14:67-69. 9. Tyagi M, Govindhari V, Pappuru RR, Ambiya V. Bilateral Hypopyon Uveitis in Chronic Myeloid Leukemia. Ocul Oncol Pathol. 2017;4(1):12-15. |

