History
A 73-year-old black female presented with a chief complaint of itchy, burning eyes (the right eye more so than the left) for the past 10 days.
She said that her medical doctor had prescribed some cream (sulfacetamide) and hot compresses, but these did not seem to be working. She also asked if I knew what could be done about a lesion in the corner of her lip.
Her systemic history was remarkable for hypertension, for which she was compliant and properly medicated with a thiazide diuretic. Her history of present illness was remarkable for a cold.
Her ocular history was unremarkable, and she denied having allergies of any kind.
|
|
|
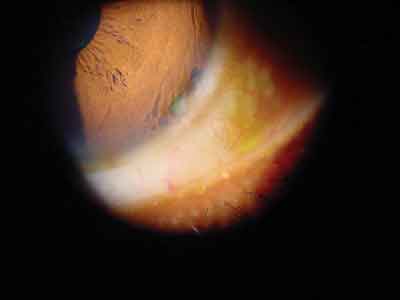
The patients eye demonstrated this appearance in the anterior segment. |
Diagnostic Data
Her best-corrected visual acuity was 20/25 O.U. at distance and near. External examination was completely normal with no afferent pupillary defect.
The pertinent anterior segment finding is demonstrated in the photograph. There was sodium fluorescein pooling, but no staining or corneal epitheliopathy was detected.
The anterior chamber was free of any inflammation. Goldmann intraocular pressure measured 14mm Hg in both eyes. The dilated fundus examination was normal.
Your Diagnosis
How would you approach this case? Does this patient require
additional tests?
What is your diagnosis? How would you manage this patient? What is the likely prognosis?
Discussion
Additional tests included rechecking the history for surgical etiologies of the defect; eversion of the eyelids to ensure health of the palpebral conjunctiva; assessment of tear volume, quality and coverage; assessment of lid-to-globe congruity and eyelid posture; assessment of blink rate and blink posture; and corneal sensitivity testing.
The diagnosis in this case is corneal dellen secondary to incomplete eyelid closure upon blinking. Although the eye was cosmetically free from the signs of irritation, inflammation or dryness (i.e., white and quiet), we initiated copious topical tear therapy (solution and ointment) because of the asthenopic symptoms and clinical tissue changes. We also educated the patient about potential punctal occlusion and/or tarsorrhaphy. We will become increasingly aggressive in her therapy as needed.
As of press time, the patient maintained a stable cornea with topical tears only. We are currently following her bimonthly.
Any globe or eyelid defect that produces suboptimal lid-globe apposition during lid closure can lead to dellen formation due to focal corneal dehydration as the result of an altered tear meniscus.1 Typically, the phenomena are observed at the inferior corneal-limbal junction, adjacent to pingueculae, pterygia or limbal surgical sites (such as a filtering bleb). Dellen rarely perforate the cornea and are not subject to inflammatory processes. They are associated with corneal dehydration.1-3
Dellen defects can be reversed using surgical eyelid procedures such as tarsoconjunctival surface contour or by nonsurgical moisture/tear restoration.1,2 In surgical cases, the goal is to flatten the dome shape of the tarsal plate, which is interrupting the eyelid posture and tear coverage. With sufficient relubrication, the area will rehydrate and stabilize.1 Exercise caution, however, as a cornea without proper cellular constituents cannot be expected to easily repair itself.
The stomatitis (canker sore), possibly the result of oral dryness or herpetic breakout, was treated with bland ointment and resolved over the course of one month.
1. Kwok SK, Tse DT. Central corneal dellen: a complication of upper eyelid tarsotomy. Ophthal Plast Reconstr Surg 2000 May;16(3):237-40.
2. Tsai YY, Lin JM, Shy JD. Acute scleral thinning after pterygium excision with intraoperative mitomycin C: A case report of scleral dellen after bare sclera technique and review of the literature. Cornea. 2002 Mar;21(2):227-9.