Q. I have a new patient who had LASIK five years ago and has a significant decrease in best-corrected vision. I suspect macrostriae, but how can I be sure?

A. First, perform a meticulous refraction. Thats going to tell us: Is there a problem with the patients optics? Or, is there just a residual refractive error that we need to correct? says Peter S. Hersh, M.D., of New Jersey Medical School in Newark, N.J. If there is a problem with the patients optics, these four diagnostic steps can help you determine whether macrostriae are the culprit:
Slit lamp examination. Examine the quality of the ocular surface, starting with the tear film. Are there areas in which the surface epithelial cells are not meticulously smooth, resulting in early tear break-up in a ridge-like pattern? This is a good indication that were dealing with macrostriae, Dr. Hersh says.
Also, evaluate the patient with retroillumination after he or she has been dilated. The more broad the striae and the closer to the visual axis, the more likely they are to have an effect on vision, says optometrist Jimmy Jackson, president and clinical director for Insight LASIK in Lafayette, Colo.
Manual keratometry of the mires. Look for non-pristine mires that do not overlap well or are irregular, as this will help you determine whether the striae are clinically significant. Irregular mires are suggestive of striae, whereas grossly distorted mires are secondary to an irregular optical topography, Dr. Hersh explains.
Corneal topography. Dr. Hersh says corneal topography must be done to rule out other optical irregularities such as astigmatism, which may be secondary to the laser ablation itself. In addition, the video-keratography of the corneal topography along with the kera-tometry readings will show us if the surface optical architecture is smooth or irregular, he says.
Assess with a gas permeable lens. Jason Stahl, M.D., of Durrie Vision in Olathe, Kan., says that if the patients best corrected vision is improved with the gas permeable (GP) lens, then you know that the surface irregularity is likely due to the striae. The tear film underneath the contact lens smoothes out the gross optical topography irregularities caused by the striae, he says.
Q. So, what treatment options can help this patient?
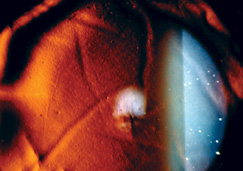
Flap macrostriae as seen via slit lamp with retroillumination. Photo courtesy: Greg Hoffmeyer
A. Flap lift. Refer the patient to a surgeon for lifting and smoothing of the corneal flap. Once the flap is smoothed, the vision problem will be alleviated, Dr. Stahl says. How-ever, he notes sometimes this procedure does not work because the striae may have become fixed.
In this case, he would suture the flap back into position, as the sutures provide traction to the flap and help stretch the striae out. To prevent the striae from developing again, I will typically leave the sutures in place for approximately one month, he says.
Photorefractive therapy (PRK). For recalcitrant striae, Dr. Jackson suggests you refer the patient for PRK with a small spot scanning laser. Unless the patient is myopic, this will cause a refractive shift and necessitate a two-step procedure, he says. To correct any residual hyperopia following PRK, conductive keratoplasty (CK) would be my recommendation.
A successful alternative to PRK is phototherapeutic keratectomy (PTK), as the epithelium acts as a masking agent, causing only a minimal hyperopic shift.1 PTK can decrease the level of the hills, so they match more smoothly with the valleys of the striae, Dr. Hersh says.
Fit with a GP lens. Fit the patient with a gas permeable lens if he or she does not want or qualify for surgery. The tear film fills in those hills (or peaks) and valleys, providing patients with a vast visual improvement, Dr. Hersh says.
1. Steinert RF, Ashrafzadeh A, Hersh PS. Results of phototherapeutic keratectomy in the management of flap striae after LASIK. Ophthalmology 2004 Apr;111(4):740-6.

